Continuing Education Activity
Chigger is the common name for species of the Trombiculid family of mites. Bites from the larva of these mites can cause local pruritus and irritation. This is called trombiculiasis or trombiculosis. The reaction is usually mild and self-limited, but the bites can transmit disease or result in bacterial superinfection. While there are many species of parasitic mites in a variety of habitats worldwide, the species most commonly referred to as chiggers include Eutrombicula alfreddugesi in the south of the United States, Trombicula autumnalis in Europe, and species of the Leptotrombidium genus in Asia and Oceania. This activity reviews the presentation of chigger bites and highlights the role of the interprofessional team in its management and prevention.
Objectives:
- Describe the pathophysiology of chigger bites.
- Review the presentation of chigger bites.
- Outline the treatment and management options available for chigger bites.
- Explain interprofessional team strategies for improving care coordination and outcomes in patients with chigger bites.
Introduction
Chigger is the common name for species of the Trombiculid family of mites. Bites from the larva of these mites can cause local pruritus and irritation. This is called trombiculiasis or trombiculosis. The reaction is usually mild and self-limited, but the bites may rarely transmit disease or result in a bacterial superinfection.[1]
While there are many species of parasitic mites in a variety of habitats worldwide, the species most commonly referred to as chiggers include Eutrombicula alfreddugesi in the south of the United States, Trombicula autumnalis in Europe, and species of the Leptotrombidium genus in Asia and Oceania.[2] The larvae of these species feed on the skin of a variety of animals, including humans. Adult mites burrow into the soil and feed on detritus, while the larvae of these species accumulate on the edges of leaves and grass before hitching on to a passing host. They then migrate to a preferred feeding site, attach themselves to the host’s skin, and secrete proteolytic enzymes to digest host epidermal cells.[3] This provokes an inflammatory reaction with surrounding erythema, a variable degree of swelling, and intense pruritus.
The larvae easily dislodge by scratching and rarely remain attached to humans for more than 48 hours, but the intense pruritus, inflammation, and localized allergic response may last for weeks. Rarely, the light-red to orange-colored larva, measuring 0.15 to 0.3 mm in length, may be identified on the skin. More typically, the diagnosis of trombiculiasis will depend on exposure to a trombiculid habitat, the pattern of the lesions, and the exclusion of other possible diagnoses.[1]
Etiology
Trombiculiasis, by definition, is caused by the bite of trombiculid mites and requires exposure to the preferred habitat of these larval mites. Once bitten, digestive enzymes secreted by the mite cause liquefaction of the host's epidermis, leading to a localized hypersensitivity reaction. This causes the papules, erythema, and urticaria that characterize the condition.[1][4]
Epidemiology
Larval mites mature to their parasitic stage between June and September in the Northern Hemisphere. Therefore, nearly all instances of trombiculiasis occur in the summer and fall. In tropical areas worldwide, however, exposure may occur at any time of the year.[1] Chigger bites can occur in patients of any age with a history of exposure to chigger habitats. These habitats include overgrown fields, wooded areas, or ground with moist soil near bodies of water. Trombiculiasis has traditionally been associated with occupational exposure among harvest workers, but it can also occur in suburban or urban areas where there is exposure to a grassy field, an overgrown lawn, or a garden. Therefore, the true incidence of trombiculiasis is largely unknown and limited to case reports.[5] This is largely due to the self-limited nature of the disease, which frequently leads to underreporting.
Chiggers are known vectors of scrub typhus in humans.[6] Scrub typhus is caused by the bacteria Orientia tsutsugamushi. The risk of disease in humans in urban areas is not well established; however, a recent study from Thailand reported a high prevalence of chigger infestation (76.8%) in animals trapped in urban public parks from Bangkok.[6] They did not, however, detect any O. tsutsugamushi in their study. Chigger-associated scrub typhus has a broad geographical distribution. It was previously thought to occur only in the Asian-Pacific area and northern Australia, with the area being identified as the "Tsutsugamushi Triangle."[7] However, reports of scrub typhus in Africa, southern Chile, and the Middle East have broadened the endemic area of this disease. A recent study reported evidence of Rickettsia infection in chiggers in North Carolina, USA.[7]
Pathophysiology
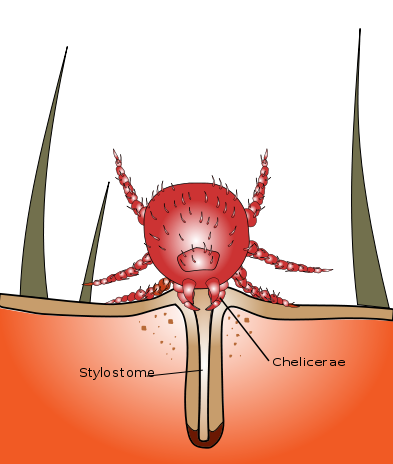
Trombiculid mites gain access to human skin via direct contact through pant cuffs, open sleeves, or shirt collars. The larvae then migrate on the skin. Barriers to this migration, such as a belt or elastic waistband, cause the clustering of larvae in these areas.[8] Once attached to the skin, they secrete digestive enzymes to liquefy epidermal cells for feeding. This induces local irritation and inflammation at the bite site.
As the larval mite liquefies epidermal cells, the skin around the bite will become edematous. This forms a papule around the mite, leading to the impression that the mite has burrowed into the skin. The mite can sometimes be seen on or within the papule but will usually have become dislodged before the irritation begins. The pruritus usually resolves within a few days but may last for as long as two weeks.
Chigger bites form erythematous papules that may occur in clusters. Surrounding macules, vesicles, and rarely, bullae may develop. Because the mites migrate on the host's body to a protected area with thin skin, they will often accumulate along the borders of tightly fitting clothing. Several bites in a linear pattern may occur along the waistband, the in-seam of underwear, or above the socks or shoes.[4]
History and Physical
Trombiculosis
Chigger bites can occur in any person exposed to the appropriate habitat during the summer months. Patients with occupational exposure will probably be familiar with chigger bites, but even working in a suburban yard, garden, or a casual walk in the park may expose a patient to trombiculid mites.
Cutaneous inflammation and intense pruritus followed by a papular and papulovesicular cutaneous rash are typical of trombiculosis.[1] A typical patient will present after a few days of intense itching with grouped or linear patterns of papules on exposed skin or along a line next to tight-fitting clothes. The papules may develop surrounding dark red to violaceous macules, or they may develop into vesicles. Rarely, bullae may form.[2] Pruritis usually resolves within a few days. Prolonged cutaneous eruption with pruritus is rare but can occur.[1] As stated before, the location of the rash/bites tends to be around the legs and waistline.
Summer Penile Syndrome
Penile swelling, pruritus, and dysuria can occur in young boys due to a local hypersensitivity response to chigger bites on the penis.[9] This tends to be a seasonal phenomenon and is hence described as "the summer penile syndrome" or lion's mane penis.[4] Affected patients usually range in age from seven months to 11 years. Pruritis is the most common symptom (reported in up to 84% of the patients in one study). Penile edema, a papule or bite puncture mark, and erythema are frequently noted. The duration of symptoms is about four days (ranging from 1 to 18 days).[9] Itching usually resolves without intervention after 2 to 3 days but may last as long as two weeks.[2]
Scrub Typhus
Chiggers are known vectors of scrub typhus, which is a bacterial infection caused by a gram-negative coccobacillus, Orientia tsutsugamushi.[10] Although Hantavirus,[11] Borrelia burgdorferi,[12] and Ehrlichia phagocytophila[13] have been detected in trombiculid mites, the transmission of these diseases from trombiculid mites to humans has not been reported.
Scrub typhus presents with headache, anorexia, and malaise, which is usually slow in onset.[14] Some patients may have an abrupt onset of high fever, intense headache, and diffuse myalgias.[14] A centrifugal maculopapular rash is seen in 50% of the patients, which usually begins on the abdomen and then spreads to involve the extremities and the face. Petechiae formation is rare. In contrast to the rash associated with chigger bites, this rash is nonpruritic. At the site of the chigger bite, however, an eschar with central necrosis will be seen.[15]
Other signs and symptoms of scrub typhus include nausea, vomiting, diarrhea, generalized lymphadenopathy, and relative bradycardia.[16] In elderly patients, acute kidney injury with altered sensorium is more prevalent than in younger patients infected with scrub typhus.[17] A recent case report identified QT prolongation with focal ischemic changes on an electrocardiogram (ECG) of a patient with afebrile scrub typhus and a normal coronary angiogram.[18] His ECG changes resolved after treatment with doxycycline.
Evaluation
No evaluation other than a thorough history and physical is necessary to diagnose or treat trombiculiasis. As previously described, a history of outdoor exposure during the summer or early fall, along with a pattern of scattered urticarial papules, can establish trombiculiasis as the presumed diagnosis.[1]
Similarly, there is no laboratory test that reliably identifies scrub typhus in the early phase of the infection. Clinical assessment is the key to the diagnosis of this infection. When suspected, serologic testing can be used to confirm the diagnosis. A fourfold increase in titers drawn at least two weeks apart using an indirect fluorescent antibody (IFA) confirms the diagnosis of acute scrub typhus.[19] Polymerase chain reaction (PCR) assays for scrub typhus have been developed but are not widely available.
Treatment / Management
The management of chigger bites is focused on symptom control with oral antihistamines or topical corticosteroid creams. Cold compresses may also help decrease discomfort and localized swelling. There is no role for covering the bite in nail polish, vaseline, or cream intended to suffocate the parasite.[1][4]
Itching can be treated with topical menthol or calamine lotion. In severe cases, potent topical corticosteroids with occlusion may be used.[20] If topical therapy fails, intralesional corticosteroid injections of triamcinolone acetonide can be used.[20] In the vast majority of cases, however, this is unnecessary. Exposed clothing should be washed in hot water or treated with insecticides to kill the larvae.[21]
Scrub typhus is treated with doxycycline.
Differential Diagnosis
The appearance of scattered papules along exposed skin or clustered around tightly fitted clothing after an outdoor exposure naturally suggests arthropod bites. Consideration should be given to scabies, bedbug bites, and exposure to mosquitoes or ants. The bites of fleas may sometimes also be in a linear pattern along tightly fitting clothing and should especially be considered if there are animals in the patient's home.
Rashes from many other infectious agents, autoimmune conditions, or sensitivity reactions may appear similarly. The history of outdoor exposure, the seasonal nature of symptoms, and the absence of recurrence are important to distinguish trombiculiasis from other causes of rash. Trombiculiasis should not be the presumed diagnosis in any ill-appearing patient, any patient with abnormal vital signs, any patient with extensive vesicles or bullae, or whose lesions are painful instead of pruritic.[1][4]
Summer penile syndrome, as a particular and localized form of trombiculiasis, has its own differential diagnosis, including balanitis, phimosis, and paraphimosis. Balanitis is a painful inflammation of the glans penis, which may be associated with purulent exudate and erosion of the skin covering the glans. Phimosis is a constriction of the foreskin, preventing it from fully retracting over the glans. Paraphimosis is a constriction of the foreskin in which the foreskin is stuck over the glans or shaft of the penis, restricting circulation to the glans. Both conditions may also be associated with penile swelling. In summer penile syndrome, the edematous skin should be minimally tender and retract easily over the glans in uncircumcised males. Cellulitis and abscesses must be excluded as well.[9]
Prognosis
In the vast majority of cases, trombiculiasis will resolve spontaneously within a few weeks as long as there is no re-exposure. The risk of super-imposed bacterial infection or transmission of other bacterial diseases is generally quite low. Therefore, the prognosis of chigger bites is almost invariably good. If there is a possibility of re-infection, the provider should counsel the patient on avoiding chigger habitats, covering the skin when passing through infested areas, or using repellents and insecticides to avoid exposure.[1][4]
Complications
Notable complications from trombiculiasis include cellulitis from excoriations, summer penile syndrome, and the transmission of scrub typhus. Untreated scrub typhus can result in severe disease with multi-organ failure and death.[22] Other systemic manifestations of scrub typhus include arrhythmias, ischemic changes, and QT prolongation.[18]
Deterrence and Patient Education
Prevention is the key to limiting chigger bite-associated illnesses. Avoiding areas of chigger infestation is the easiest way to prevent trombiculiasis. If exposure is unavoidable, patients can be advised to use elastic bands to close the hems of sleeves and pant legs tightly against the skin, to cover the skin completely, or to tuck the hems of their pants into socks or boots. DEET repellent and permethrin are also effective deterrents to chigger bites.[1][4] Insect repellents are highly effective in repelling these mites and should be used when exposure is a possibility.[23]
DEET
DEET (N, N-diethyl-meta-toluamide or N, N-diethyl-3-methylbenzamide) repellent is highly effective against these larvae and is considered the "gold standard" treatment for prevention.[24] DEET has been regarded as the most efficacious insect repellent for the last six decades and has a strong safety record with excellent protection against ticks, mosquitoes, and other arthropods.[24] Although it is available in many different formulations, its effectiveness plateaus at around 30% concentration.[25] However, a higher percentage formulation is expected to provide a longer duration of protection.[24] Serious adverse effects are uncommon. Excessive exposure through the skin has been associated with dermatitis and allergic reactions. In rare cases, neurotoxicity with seizures may occur.[26] DEET is safe to use in children older than two months of age, but caution is needed to ensure accidental oropharynx exposure and ingestion do not occur.
Permethrin
Permethrin is a synthetic compound that is neurotoxic to insects but does not cause any systemic toxicity in humans.[21] It is applied to clothing and bedding and is effective against ticks and chiggers. Permethrin-treated clothing maintains its efficacy through multiple wash cycles; however, compared to 50% DEET spray, permethrin's repellency is significantly inferior.[27]
Pearls and Other Issues
- Chigger bites typically occur during summer and early fall in those with recent outdoor exposure. However, in tropical areas of the world, chigger bites can occur year-round.
- Patients usually display pruritic papules, sometimes clustered around tightly fitting clothes.
- Itching usually lasts a few days but can sometimes extend as long as two weeks.
- Lesions can sometimes form vesicles or bullae and may have surrounding violaceous macules.
- Treatment is usually restricted to oral antihistamines, cold compresses, and topical corticosteroids.
- Prevention in those with recurrent exposure can be achieved by completely covering the skin or using insect repellents such as DEET and/or permethrin.
- Notable complications of chigger bites include secondary cellulitis, summer penile syndrome, and transmission of other diseases such as scrub typhus.
Enhancing Healthcare Team Outcomes
Trombiculiasis is easy to diagnose in the right clinical scenario. It has an excellent prognosis, and symptomatic management is all that is required. However, given the potential for transmission of serious infections through chigger bites, it is essential to prevent future exposures, and this requires an interprofessional team approach to care. Patients and caregivers should be educated regarding appropriate clothing and the use of insect repellents to prevent these bites. The clinical nurse plays an essential role in providing this education as a primary or secondary preventive measure. Occupational nurses play a pivotal role in ensuring workers exposed to chigger-infested environments are properly protected. The clinical provider should ensure there are no signs of chigger-borne infections when a patient presents for the evaluation of a chigger bite. Pharmacists can counsel patients on medical options and consult with the clinician if needed. All care team members should maintain accurate, updated medical records and communicate with other caregivers if necessary. A well-integrated interprofessional team of clinicians and nurses can decrease the incidence of chigger bites and their associated infections. [Level 5]