Introduction
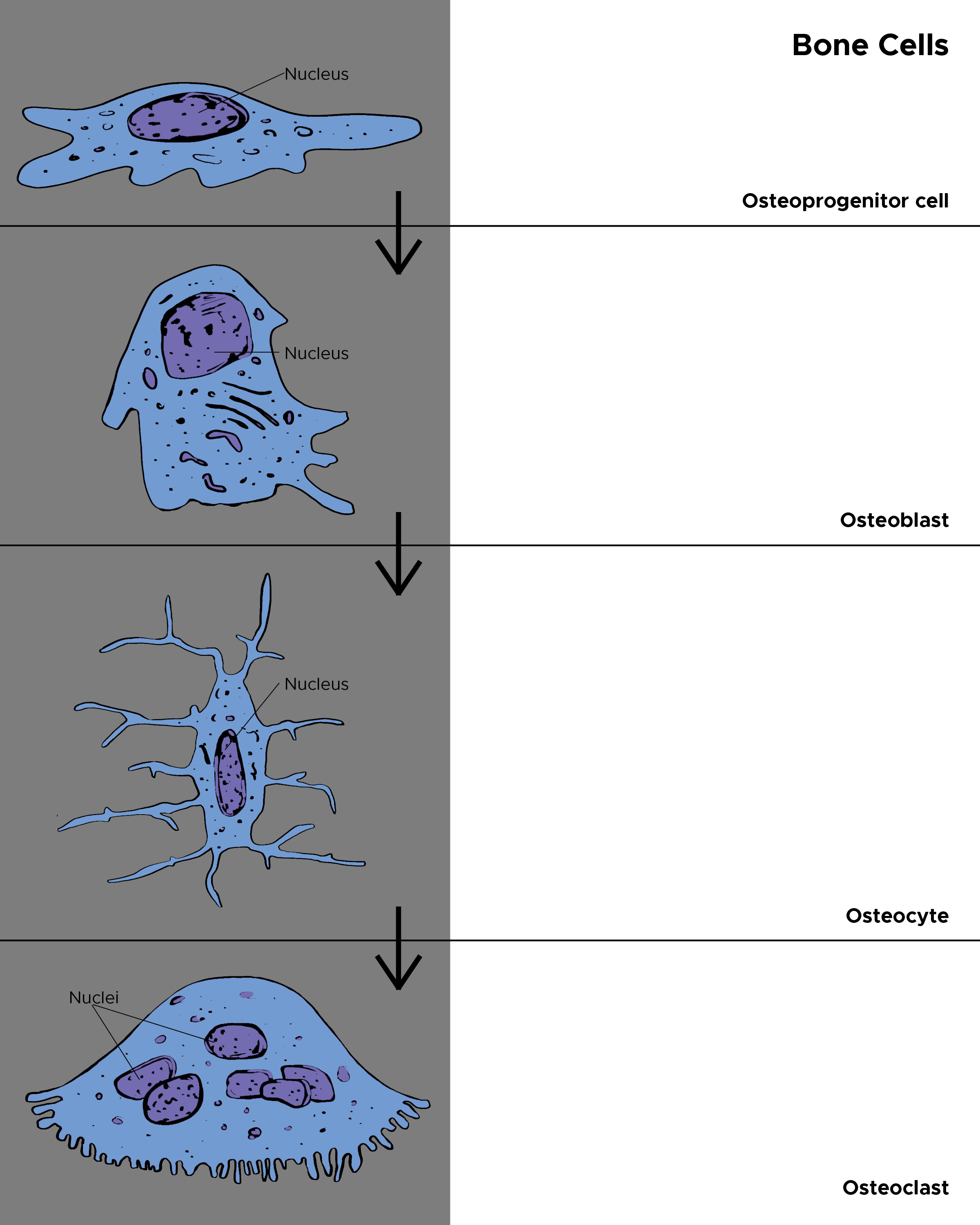
Osteoprogenitor cells, also known as osteogenic cells, are stem cells in the bone that play a prodigal role in bone repair and growth (see Image. Cells in the Bone).[1] These cells are the precursors to the more specialized bone cells (osteocytes and osteoblasts) and reside in the bone marrow. Osteoprogenitor cells originate from infant mesenchymal cells and turn into spindle cells at the surface of matured bones. In developing bones, they appear more frequently and activate multifunctional stages to remodel the bones. The body loses the ability to synthesize or utilize more osteoprogenitor cells with age. Dysfunction of osteoprogenitor cells may delay ossification and lead to a spectrum of diseases such as dwarfism and Kashin-Beck disease.[2]
Structure
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure
Osteoprogenitor cells are often referred to as preosteoblasts. They can be present within the endosteum, the cellular layer of the periosteum, and the lining of the osteogenic cells. In matured bones that no longer display active bone remodeling or formation, osteoprogenitor cells exist as flattened spindle-shaped structures. They attach to the bone surface and are referred to as inactive osteoblasts during this period. In maturing bones, however, these cells appear in their largest form. During fetal development or high turnover periods in adult osteogenesis, numerous osteoprogenitor cells function to give rise to osteoblasts. These structures display plump oval nuclei and emboldened abundant spindle-shaped cytoplasm at this stage, later converting to characteristic cuboidal active osteoblasts.[3][4]
Function
Osteoprogenitors can self-proliferate and self-renew. They participate in osteogenic differentiation and play a role in regulating angiogenesis.[5] Osteoprogenitor cells can differentiate into osteoblasts through mitotic division or by dividing into two stem cells via a highly regulated mechanism, which remains static during the proliferation process. After completing DNA synthesis and cell expansion, the cell retains its original genetic information. The endocrine system and local factors (growth factors and cytokines) mainly regulate osteogenesis.
Neuropeptide Y is a potent regulator of osteogenesis, and recent studies have confirmed that osteoprogenitor cells originating from hypothalamic Y2-/- mice have enhanced osteogenic activities.[6] Proline-rich tyrosine kinase 2 supposedly regulates the differentiation of early osteoprogenitors, and proline-rich tyrosine kinase 2 inhibitors promote osteogenesis and could act as a treatment for osteoporosis.[7] Osteoprogenitor cells also reside in the perichondrium. These osteoprogenitors hyper-regulate bone morphogenetic proteins during differentiation into mature osteoblasts responsible for the production of bone matrix.[8]
Tissue Preparation
Bone marrow stromal cells (BMSCs) yield testable osteoprogenitors. The cell samples are diluted with phosphate-buffered saline (PBS) at a ratio of 1:3 then nucleated cells are isolated with a density gradient solution. Preparatory phase complete medium (CM) consists of 0.1 mmol/L nonessential amino acids, alpha-MEM with 10% fetal bovine serum, 4.5 mg/mL d-glucose, 1 mmol/L sodium pyruvate, 100 U/mL penicillin, 100 mmol/L HEPES buffer, 100 μg/mL streptomycin, and 0.29 mg/mL l-glutamine.[9]
The collected nucleated cells are plated at a density of 100,000 cells/cm^2 in supplemented CM. The CM supplement requires an additional 5 ng/mL fibroblast growth factor-2 (GF2) and 10 nmol/L dexamethasones; both elements proliferate osteogenic commitment of bone marrow stromal cells. The supplemental process undergoes humidification at 37 degrees C in a 5% CO2 incubator.[10]
Histochemistry and Cytochemistry
The development of osteoprogenitor cells has been studied by several research groups. A study suggests that the perichondrial Thy-1–positive cells demonstrate potential osteogenic activity and participate in osteoblast formation during endochondral ossification. Another study shows intense alkaline phosphatase activity two weeks after osteogenic induction and the presence of mineralized nodules. The expression of bone sialoprotein, dentin matrix protein-1, and osteocalcin increases due to ALP proliferation. 55 to 65% of cells, as confirmed by flow cytometry, display the cell-surface markers Sca1+ and Thy1+ in vitro expansion for an alpha-SMA-GFP positive population. The alpha-SMA–GFP-positive population also exhibits high proliferative and osteogenic probabilities when compared to an alpha-SMA–GFP-negative population.[8][11]
Microscopy, Light
Final visualization of osteoprogenitor cells under the microscope involves a delicate preparation phase: the explants are fixed in 4% buffered formalin for one whole day, and samples are decalcified with 0.5 mol/L ethylenediaminetetraacetic acid (pH 8) for 7 to 10 days. The samples are deposited in paraffin, and the cross-sections of the samples are prepared with 5 um thickness at three different strata.[12]
The samples are stained with hematoxylin/eosin and Masson/Trichrome, and both a qualitative exam for the presence of bone tissue and a quantitative exam by computerized bone histomorphometry is conducted. For each hematoxylin/eosin-stained cross-section, 3 or 4 images (adequate to fill the construct cross-sections) are required to calculate the bone tissue area and available area for tissue ingrowth (net implant area - undegraded scaffold area) by digital imaging analysis. Under the visuals of scanning electron microscopy (SEM), the red color in the slides that are stained by Masson/Trichrome indicates lamellar and remodeled bone, while the blue color shows freshly deposited and immature bone.[9]
Pathophysiology
Bone tumors are formed within osteoprogenitor or stromal cell lineage during Paget disease (PD), which likely derive from genetic alterations related to familial Paget’s disease. During Paget’s disease, the endosteal surface undergoes active remodeling, and abnormal osteoclasts bearing nuclear inclusions occur. The fibrotic tissues in bone biopsies from PD patients are considered to be made of surplus elongated, sophisticatedly branched stromal cells that display high alkaline phosphatase levels; these cells are similar to the pre-osteogenic stromal cells located within the normal bone marrow.[13]
Early and full-blown pagetic lesions show dynamic transformations in the arrangement, number, and function of stromal cells within endosteal/medullary tissue. An excessive amount of bone marrow osteoprogenitor cells in pagetic lesion areas verify earlier data on static and dynamic histomorphometry in patients with Paget’s disease. Previous data revealed that the rate of osteogenesis increases during Paget disease, but research has confirmed that there is also a surge in the birthrate of osteoblasts.[14]
The quality of the new bones depends on nature and hypermineralization taking place. Most stromal/osteoblastic abnormalities result from bone mass increment, characterized by denser and thicker trabecular structures. Compromised mechanical integrity caused by poor architectural organization and transformations within the mineralized matrix material is an additional characteristic.[15]
Clinical Significance
Mesenchymal stem cells (MSCs) collected from adipose and bone marrow tissue hold therapeutic value for various bone disease treatments. Current studies demonstrate the benefit of bone grafts based on combinations of MSC, biomimetic scaffolds, and growth factor delivery, which showed an increased osteogenic regeneration rate with minimal side effects. The specific mechanisms of cellular signaling in bone remodeling are essential in understanding the incorporation of newer effective treatment methods for numerous bone diseases.[16]
Various transplant therapies involving osteogenic autologous bone grafts are less frequently used; patient-specific cell therapies involving autologous BM-MNCs (bone marrow mononuclear cells) composed of stem cells, monocytes, lymphocytes, and dendritic cells are rising in popularity for bone pathology treatments. All patients suffering from long-bone pseudoarthrosis attained full bone consolidation when treated with autologous BM-MNCs and allogeneic cancellous bone grafts. Bone marrow aspirate utilized during osteonecrosis treatment via minimally invasive decompression of the femoral head decreased disease progress and yielded overall pain and symptom relief. Bone marrow concentrated injections lead to better osteogenic unions, resulting in complete recovery in post-operative achondroplastic dwarf patients within 2 to 10 months after femoral lightning surgeries. Intravenous BMC injections, mixed with iloprost, proliferate fracture healing in patients with avascular necrosis. Patients receiving Intra-articular BMNc displayed better chewing and maximum interincisal opening with integral pain relief.[17][16]
Media
(Click Image to Enlarge)
References
Friedenstein AJ, Chailakhyan RK, Gerasimov UV. Bone marrow osteogenic stem cells: in vitro cultivation and transplantation in diffusion chambers. Cell and tissue kinetics. 1987 May:20(3):263-72 [PubMed PMID: 3690622]
Level 3 (low-level) evidenceRen X, Zhou Q, Foulad D, Tiffany AS, Dewey MJ, Bischoff D, Miller TA, Reid RR, He TC, Yamaguchi DT, Harley BAC, Lee JC. Osteoprotegerin reduces osteoclast resorption activity without affecting osteogenesis on nanoparticulate mineralized collagen scaffolds. Science advances. 2019 Jun:5(6):eaaw4991. doi: 10.1126/sciadv.aaw4991. Epub 2019 Jun 12 [PubMed PMID: 31206025]
Level 3 (low-level) evidenceXu J, Wang Y, Hsu CY, Gao Y, Meyers CA, Chang L, Zhang L, Broderick K, Ding C, Peault B, Witwer K, James AW. Human perivascular stem cell-derived extracellular vesicles mediate bone repair. eLife. 2019 Sep 4:8():. doi: 10.7554/eLife.48191. Epub 2019 Sep 4 [PubMed PMID: 31482845]
Clines GA, Prospects for osteoprogenitor stem cells in fracture repair and osteoporosis. Current opinion in organ transplantation. 2010 Feb; [PubMed PMID: 19935065]
Level 3 (low-level) evidenceIbrahim A, Bulstrode NW, Whitaker IS, Eastwood DM, Dunaway D, Ferretti P. Nanotechnology for Stimulating Osteoprogenitor Differentiation. The open orthopaedics journal. 2016:10():849-861. doi: 10.2174/1874325001610010849. Epub 2016 Dec 30 [PubMed PMID: 28217210]
Lundberg P, Allison SJ, Lee NJ, Baldock PA, Brouard N, Rost S, Enriquez RF, Sainsbury A, Lamghari M, Simmons P, Eisman JA, Gardiner EM, Herzog H. Greater bone formation of Y2 knockout mice is associated with increased osteoprogenitor numbers and altered Y1 receptor expression. The Journal of biological chemistry. 2007 Jun 29:282(26):19082-91 [PubMed PMID: 17491022]
Level 3 (low-level) evidenceHan S, Mistry A, Chang JS, Cunningham D, Griffor M, Bonnette PC, Wang H, Chrunyk BA, Aspnes GE, Walker DP, Brosius AD, Buckbinder L. Structural characterization of proline-rich tyrosine kinase 2 (PYK2) reveals a unique (DFG-out) conformation and enables inhibitor design. The Journal of biological chemistry. 2009 May 8:284(19):13193-201. doi: 10.1074/jbc.M809038200. Epub 2009 Feb 25 [PubMed PMID: 19244237]
Nakamura H,Yukita A,Ninomiya T,Hosoya A,Hiraga T,Ozawa H, Localization of Thy-1-positive cells in the perichondrium during endochondral ossification. The journal of histochemistry and cytochemistry : official journal of the Histochemistry Society. 2010 May; [PubMed PMID: 20124093]
Level 3 (low-level) evidenceJaquiéry C, Schaeren S, Farhadi J, Mainil-Varlet P, Kunz C, Zeilhofer HF, Heberer M, Martin I. In vitro osteogenic differentiation and in vivo bone-forming capacity of human isogenic jaw periosteal cells and bone marrow stromal cells. Annals of surgery. 2005 Dec:242(6):859-67, discussion 867-8 [PubMed PMID: 16327496]
Level 3 (low-level) evidenceDupree MA, Pollack SR, Levine EM, Laurencin CT. Fibroblast growth factor 2 induced proliferation in osteoblasts and bone marrow stromal cells: a whole cell model. Biophysical journal. 2006 Oct 15:91(8):3097-112 [PubMed PMID: 16861274]
Level 3 (low-level) evidenceSan Miguel SM, Fatahi MR, Li H, Igwe JC, Aguila HL, Kalajzic I. Defining a visual marker of osteoprogenitor cells within the periodontium. Journal of periodontal research. 2010 Feb:45(1):60-70. doi: 10.1111/j.1600-0765.2009.01201.x. Epub 2009 Apr 30 [PubMed PMID: 19453851]
Level 3 (low-level) evidenceDhouskar S, Tamgadge S, Tamgadge A, Periera T, Mudaliar U, Pillai A. Comparison of Hematoxylin and Eosin Stain with Modified Gallego's Stain for Differentiating Mineralized Components in Ossifying Fibroma, Cemento-ossifying Fibroma, and Cementifying Fibroma. Journal of microscopy and ultrastructure. 2019 Jul-Sep:7(3):124-129. doi: 10.4103/JMAU.JMAU_2_19. Epub [PubMed PMID: 31548923]
Roodman GD, Windle JJ. Paget disease of bone. The Journal of clinical investigation. 2005 Feb:115(2):200-8 [PubMed PMID: 15690073]
Level 3 (low-level) evidenceSabharwal R, Gupta S, Sepolia S, Panigrahi R, Mohanty S, Subudhi SK, Kumar M. An Insight in to Paget's Disease of Bone. Nigerian journal of surgery : official publication of the Nigerian Surgical Research Society. 2014 Jan:20(1):9-15. doi: 10.4103/1117-6806.127098. Epub [PubMed PMID: 24665195]
Cortini M,Baldini N,Avnet S, New Advances in the Study of Bone Tumors: A Lesson From the 3D Environment. Frontiers in physiology. 2019 [PubMed PMID: 31316395]
Level 3 (low-level) evidencePoon Z, Lee WC, Guan G, Nyan LM, Lim CT, Han J, Van Vliet KJ. Bone marrow regeneration promoted by biophysically sorted osteoprogenitors from mesenchymal stromal cells. Stem cells translational medicine. 2015 Jan:4(1):56-65. doi: 10.5966/sctm.2014-0154. Epub 2014 Nov 19 [PubMed PMID: 25411477]
Level 3 (low-level) evidenceHutchings G, Moncrieff L, Dompe C, Janowicz K, Sibiak R, Bryja A, Jankowski M, Mozdziak P, Bukowska D, Antosik P, Shibli JA, Dyszkiewicz-Konwińska M, Bruska M, Kempisty B, Piotrowska-Kempisty H. Bone Regeneration, Reconstruction and Use of Osteogenic Cells; from Basic Knowledge, Animal Models to Clinical Trials. Journal of clinical medicine. 2020 Jan 4:9(1):. doi: 10.3390/jcm9010139. Epub 2020 Jan 4 [PubMed PMID: 31947922]
Level 3 (low-level) evidence