Osteopathic Manipulative Treatment: Muscle Energy and Counterstrain Procedure - Piriformis Muscle
Osteopathic Manipulative Treatment: Muscle Energy and Counterstrain Procedure - Piriformis Muscle
Introduction
Osteopathic manipulative treatment (OMT) is a group of techniques developed using manual manipulation to treat somatic dysfunction. Its goal is to improve the range of motion of muscles/joints, enhance neuromuscular function, decrease overall pain, and improve biochemical balance.[1]
Two particular techniques often used in osteopathic practice are muscle energy technique (MET) and counterstrain technique.
- Muscle energy is an active and direct technique that engages the patient’s restrictive barrier. The patient contracts the muscle of interest while the physician introduces a counterforce.[2] The counterforce can either be isometric or isotonic, and isotonic forces can be concentric or eccentric.
- Counterstrain technique is a passive and indirect technique that involves identifying a tender point or trigger point and using myofascial planes to maneuver the patient into a position that relieves pain.[3]
Piriformis Muscle/Syndrome
- Often, hypertrophy, irritation, or overuse of the piriformis muscle can lead to piriformis syndrome. Pain resulting from hypertrophy and overuse is an often overlooked cause of back or buttock pain. Additionally, due to the location of the muscle within the pelvis, it can mimic sciatic pain with radiation to the lower extremities.[4] The piriformis muscle can cause sciatic nerve entrapment syndrome.
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
The piriformis muscle is a flat and pyramid or pear-shaped muscle that is part of a larger group of muscles responsible for external or lateral rotation of the hip; gemellus superior, obturator internus, gemellus inferior, quadratus femoris, and obturator externus muscles.[5]
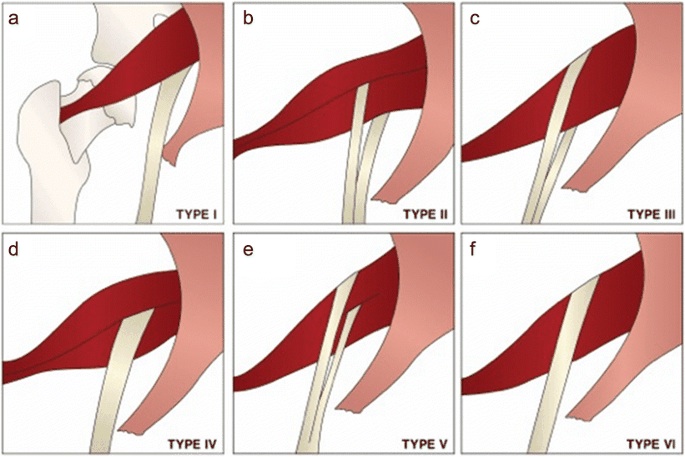
The piriformis muscle proximally attaches to the anterior and lateral surfaces of the sacrum and sacrotuberous ligament, exiting the pelvis through the greater sciatic foramen, and distally attaches to the greater trochanter of the femur. Dependent on if the hip is extended or flexed, the piriformis will externally rotate or abduct the hip, respectively.[6] The muscle is innervated by the nerve to the piriformis muscle supplied by S1-S2. Due to the position on the piriformis muscle within the pelvis, many nerves course above, below, and sometimes even through the muscle.[7] In particular, the sciatic nerve has a close passage relationship (above, through, or below).
Muscle energy techniques (METs) were born from the American Fred Mitchell in 1974. These techniques are a manipulative diagnosis and treatment methodology in which the patient's muscles are the active, intrinsic part. Everything is performed with precise and controlled positions, with directions that follow certain axes and against a specific resistance, more or less intense, by the operator. There are nerve reflexes that regulate the posturo-dynamic system: the neuromuscular unit that first controls this system is the reflex arc. This concept works according to a closed circuit: the nerve impulse originating from the muscle penetrates the posterior horn of the gray matter of the spinal cord and transmits the impulse, through a synaptic contact, to the motor neurons of the anterior horn, causing a contractile response. The monosynaptic reflex is referred to as the myotatic reflex. The receptor that coordinates this mechanism is the neuromuscular spindle, which is particularly sensitive to the stretching stimulus.
The most important receptor part is at the spindle poles and is the portion most directed towards the points of insertion of the striated muscle, which is closely related to the connective system of the muscle itself. The spindle is in parallel with the muscle fibers that surround it. In the excitation of the spindle, a dynamic component is distinguished, which occurs during the elongation of the spindle (signaled to the nerve centers through the discharge of the primary fibers; predominantly phasic signaling), and a static component, given by the new length that the muscle reaches (signaled by the discharge of secondary fibers, mainly tonic signaling). In the direct myotatic reflex, in addition to the stimulation of the agonist by more or less mild strains, there is also the automatic release of the antagonist. From this last notion comes the concept of MET techniques, as it is possible to gain a greater articular excursion thanks to the co-traction / release balance of the musculature that involves a given joint. Furthermore, METs help the musculature with a dysfunctional tonicity condition decrease its tone and recover a more physiological muscle length.[3][8][9]
The strain counterstrain technique, formerly called "spontaneous release from positioning," was devised in the 1950s by the American osteopathic physician Dr. Lawrence H. Jones, who developed this innovative approach to treating musculoskeletal disorders. The key concept of the technique is to find a comfortable position for each ailment that the patients accused: the doctor spent over twenty years of study to develop and create the definitive strain and counterstrain technique with its "tender points" (TP) anterior and posterior to the body, its ninety seconds of repositioning and the right sequence of diagnosis and treatment. The TPs, tense points, are small areas of tension in the tissues of the whole body, which, once localized, orient the diagnosis and guide the operator in his evaluation and treatment strategy.
The ideal position in which there is at least a two-thirds reduction in tension in the (TP) indicates correct body positioning. When Dr. Lawrence Jones died, there were approximately 180 TPs and related techniques. To date, his successors have developed and improved the technique covering over 200 TPs. TPs are not like trigger points because TPs have a different location. Therefore, the strain counterstrain technique is an osteopathic manual approach, which consists of a procedure of passive repositioning of the body towards a position of greater comfort. The technique consists of a gentle over-stretch directed in the opposite direction to the erroneous stretch message. This passive position relieves the patient of pain and restores the dysfunctional area, reducing and stopping the inappropriate proprioceptive activity that maintains the somatic dysfunction in the affected area. One theory to explain the benefits of this approach is the reduction of nociceptive afferents, which improves muscle efferences and prevents non-physiological muscle reflexes.
Indications
- Somatic dysfunction
- Shortened/spastic muscle
- Low back pain with or without resulting neuropathy
- Pelvic imbalance
- Limited ROM of muscle and/or extremity/joint
- Localized edema
- Trigger points
- Pain
Contraindications
- Fracture
- Torn ligament and/or tendon
- Joint instability
- Recent surgery
- Absence of somatic dysfunction and/or symptoms
- Patient refusal or nonconsenting/uncooperative patient
- Active infection/open wounds
- Neuropathic pain
- Pain caused by infections
Equipment
- Preferably an osteopathic manipulative treatment (OMT) table, but an exam table or massage table is also acceptable as long as it is maneuverable to accommodate for positioning of patient and physician.
- Stool
- Pillow for patient comfort
Personnel
- A clinician trained in osteopathic medicine
- A patient that has consented to the procedure and has no contraindications for treatment
Preparation
It is important to evaluate the piriformis muscle before engaging in treatment for two reasons, first to address and note the severity of the dysfunction prior to treatment, and second, to assess improvement of the dysfunction after treatment.
Evaluation of the piriformis muscle can occur in one of three ways depending on which technique an osteopathic physician is using to treat
- Supine
- Grab the ankles above the medial malleolus bilaterally (apply gentle traction to ensure that any rotation is coming from the hip and not the knees) and internally rotate to compare both sides
- The extremity that does not internally rotate can potentially have a spasm within the piriformis muscle.
- Prone
- Bend knees at 90 degrees and have the patient drop their legs laterally
- The extremity that laterally drops the least can potentially have a spasm within the piriformis muscle.
- Tender-point/trigger-point
- Find the point of tenderness at the body of the piriformis muscle.
Technique or Treatment
Counterstrain
- Lay the patient in the prone position and have the practitioner sit on the same side as the affected piriformis muscle
- Locate the tender point at the body of the piriformis muscle
- Classically this can be found 2 to 3 inches medial and slightly cephalad to the greater trochanter, or;
- Bisect the distance between the PSIS and ILA of the ipsilateral side, then bisect the distance between this point and the ipsilateral greater trochanter
- Have the practitioner suspend the patient's lower extremity off the edge of the table, flex the hip (approximately 135 degrees) while also abducting and externally rotating as needed until tenderness is relieved
- Hold the position for 90 seconds and slowly return the patient to a neutral position
- Reassess patient for tenderness
Muscle Energy
- Lay the patient in the supine position and have the practitioner stand on the same side as the affected piriformis muscle
- Bend the knee of the affected side and place the foot of that side on the lateral aspect of the opposite knee
- Have the practitioner push knee medially until meeting the restrictive barrier
- Have the patient push against the practitioner's resistance for 3 to 5 seconds, allow for a period of isometric relaxation, then engage a new barrier; repeat three times.[10]
- Return the patient to a neutral position and reassess using supine or prone piriformis testing.
Complications
While OMT is generally very safe, common side effects of non-high-velocity techniques are fatigue, headache, or localized and radiating pains, but typically resolve within 24 hours after treatment.[11]
Clinical Significance
Although muscle relaxants, NSAIDs, and steroid injections are possible options to treat the piriformis muscle, the use of counterstrain and muscle energy on patients is an effective and conservative alternative or adjunct to other treatment modalities.
The manual approach must be repeated with other osteopathic sessions because if the problem derives from a chronic condition, it is necessary to have sufficient time to change the texture of the tissue and the related neurological reflexes. Additional sessions will depend on the patient's physiological response and the cause of the dysfunction.
Enhancing Healthcare Team Outcomes
While osteopathic medicine has existed for over 130 years, many healthcare professionals still poorly understand it. This lack of understanding is partly due to differences in training during residency and medical school education and lack of practice in the inpatient and outpatient settings. Modalities such as muscle energy and counterstrain technique, when appropriate, can help enhance outcomes of patients and their symptoms. It is crucial for the interdisciplinary teams treating patients to understand the role of OMT in treatments and that OMT can serve as an adjunct therapy to existing therapies in place.
Media
(Click Image to Enlarge)
References
Bodine WA. Osteopathic Manipulative Treatment: A Primary Care Approach. American family physician. 2019 Feb 15:99(4):214 [PubMed PMID: 30763051]
Goodridge JP. Muscle energy technique: definition, explanation, methods of procedure. The Journal of the American Osteopathic Association. 1981 Dec:81(4):249-54 [PubMed PMID: 7319853]
Wong CK, Abraham T, Karimi P, Ow-Wing C. Strain counterstrain technique to decrease tender point palpation pain compared to control conditions: a systematic review with meta-analysis. Journal of bodywork and movement therapies. 2014 Apr:18(2):165-73. doi: 10.1016/j.jbmt.2013.09.010. Epub 2013 Oct 2 [PubMed PMID: 24725782]
Level 1 (high-level) evidenceNatsis K, Totlis T, Konstantinidis GA, Paraskevas G, Piagkou M, Koebke J. Anatomical variations between the sciatic nerve and the piriformis muscle: a contribution to surgical anatomy in piriformis syndrome. Surgical and radiologic anatomy : SRA. 2014 Apr:36(3):273-80. doi: 10.1007/s00276-013-1180-7. Epub 2013 Jul 31 [PubMed PMID: 23900507]
Hernando MF, Cerezal L, Pérez-Carro L, Abascal F, Canga A. Deep gluteal syndrome: anatomy, imaging, and management of sciatic nerve entrapments in the subgluteal space. Skeletal radiology. 2015 Jul:44(7):919-34. doi: 10.1007/s00256-015-2124-6. Epub 2015 Mar 5 [PubMed PMID: 25739706]
Probst D, Stout A, Hunt D. Piriformis Syndrome: A Narrative Review of the Anatomy, Diagnosis, and Treatment. PM & R : the journal of injury, function, and rehabilitation. 2019 Aug:11 Suppl 1():S54-S63. doi: 10.1002/pmrj.12189. Epub 2019 Jul 22 [PubMed PMID: 31102324]
Level 3 (low-level) evidenceVarenika V, Lutz AM, Beaulieu CF, Bucknor MD. Detection and prevalence of variant sciatic nerve anatomy in relation to the piriformis muscle on MRI. Skeletal radiology. 2017 Jun:46(6):751-757. doi: 10.1007/s00256-017-2597-6. Epub 2017 Mar 10 [PubMed PMID: 28280851]
Korr IM. Proprioceptors and somatic dysfunction. The Journal of the American Osteopathic Association. 1975 Mar:74(7):638-50 [PubMed PMID: 124754]
Katz R, Penicaud A, Rossi A. Reciprocal Ia inhibition between elbow flexors and extensors in the human. The Journal of physiology. 1991 Jun:437():269-86 [PubMed PMID: 1890635]
Baxter DA, Shergis JL, Fazalbhoy A, Coyle ME. Muscle energy technique for chronic obstructive pulmonary disease: a systematic review. Chiropractic & manual therapies. 2019:27():37. doi: 10.1186/s12998-019-0256-9. Epub 2019 Aug 20 [PubMed PMID: 31452871]
Level 1 (high-level) evidenceEarley BE, Luce H. An introduction to clinical research in osteopathic medicine. Primary care. 2010 Mar:37(1):49-64. doi: 10.1016/j.pop.2009.09.001. Epub [PubMed PMID: 20188997]