Palliative Sedation in Patients With Terminal Illness
Palliative Sedation in Patients With Terminal Illness
Introduction
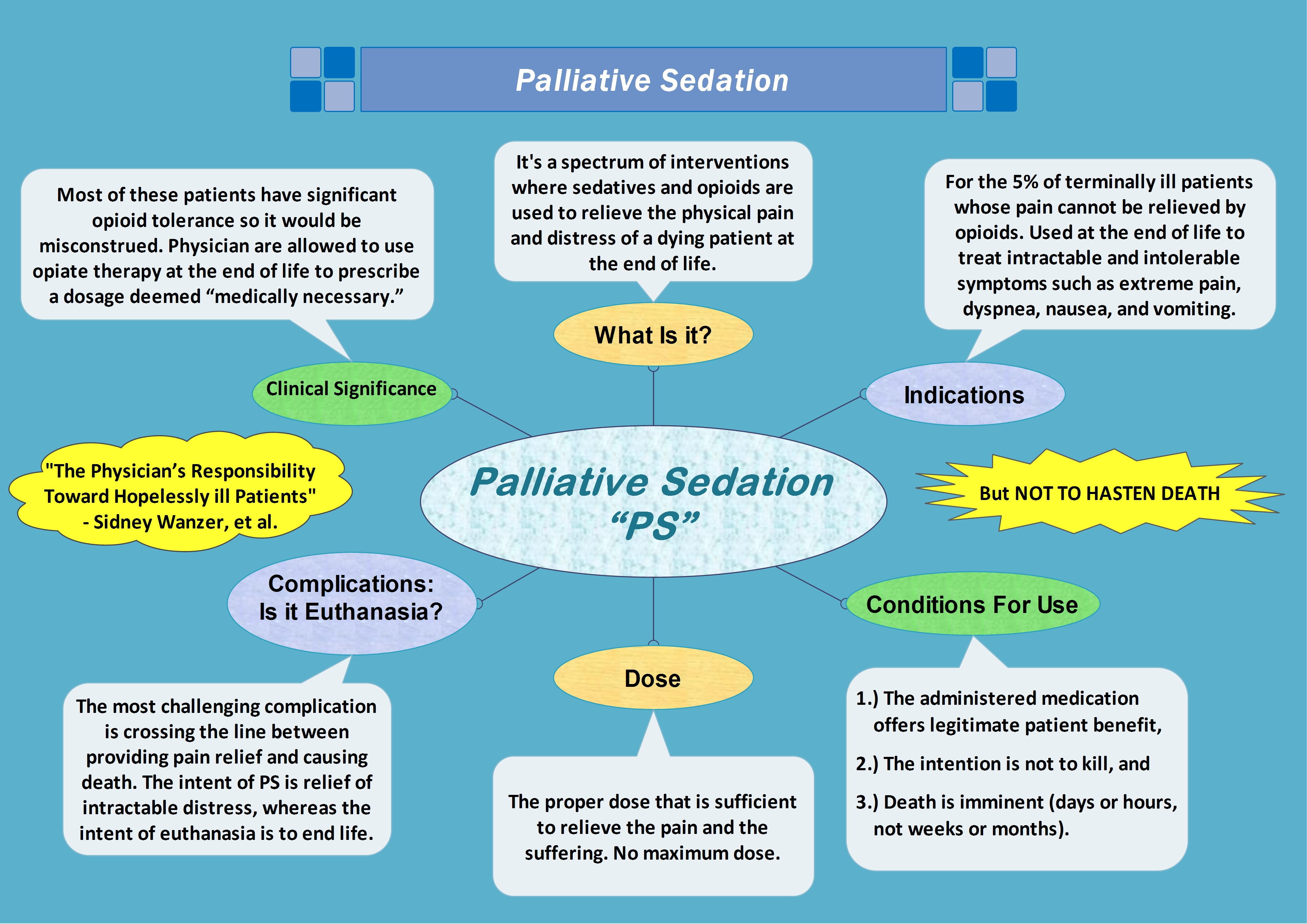
Palliative sedation encompasses a broad range of activities aimed at relieving distress in terminally ill patients. Palliative sedation involves therapy to resolve or alleviate refractory symptoms at the end of life.[1][2][3] The most common refractory symptoms in terminally ill patients are delirium, intractable pain, and shortness of breath.[4][5] There is a well-established practice and relative acceptance of the use of palliative sedation to relieve these symptoms. However, there is still open controversy and ethical debate about the use of palliative sedation for the relief of existential or psychological distress in terminally ill patients.[4][6]
Some controversy arises over a lack of consistency in defining "refractory symptoms" and a lack of adequate knowledge among patients, family members, and healthcare workers alike regarding the issue of palliative sedation.[3] Additionally, ethical and legal issues surrounding this topic, as it appears, at least superficially similar to the process of physician-assisted suicide or euthanasia, discourage physicians from initiating conversations or planning for palliative sedation in patients.[6][7] For clarity, the goal of palliative sedation is truly aimed at sedation, not a cessation of life, and studies have shown that palliative sedation overall is not associated with a shortened life span. Also, one of the guiding principles of palliative sedation is that it is applied when the anticipated life span of a terminally ill patient is in the range of hours to days.[5][8]
Prior studies have demonstrated several communication barriers between clinicians, patients, and surrogates that prevent timely planning for end-of-life issues, leading to increased anxiety and frustrations towards the medical team.[8][9][10][11][12][13][14] Furthermore, several misconceptions remain among patients and their families regarding palliative care issues, including hospice, pain control, and palliative sedation.[15][16] This review discusses the indications for palliative sedation, legal/ethical dynamics associated with its use, common misconceptions, and pharmacological agents used.
Indications
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Indications
There is no universal definition for refractory symptoms; thus, it is up to the clinician and the hospital staff's discretion to determine if certain intractable symptoms would warrant the initiation of palliative sedation. However, in general, the following are considered to fit the criteria for palliative sedation:
- The candidate for palliative sedation must have a terminal illness where death is almost certain.
- The patient's clinical presentation must be such that conventional therapies are incapable of providing relief despite maximal doses, and symptom relief cannot be obtained without affecting consciousness.
- Alternatively, a scenario can exist when conventional therapies are associated with potential adverse outcomes in patients at high doses or frequent administration of agents and thus warranting the use of palliative sedation, eg, use of frequent and high doses of Ondansetron to relieve nausea and vomiting can be associated with QTc prolongation and cardiac arrhythmias. Using sedating agents such as benzodiazepine (midazolam) might be a suitable alternative that can relieve nausea and avoid the risk of cardiac arrhythmias.
- Palliative sedation can be considered if traditional therapies cannot provide relief of symptoms in a timely manner, eg, using intravenous or intramuscular antipsychotics in acutely agitated and delirious patients with a terminal illness offers quicker results compared to standard reorientation techniques in patients, and may be necessary for the safety of the patient or caregivers.
- Well-documented goals of care discussions with the patient or surrogates must be present to outline the plan of care and potential risks of using palliative sedation.[17][18]
Ethical and Legal Issues
Although there has been a well-demonstrated benefit of better symptom control in patients with a terminal illness treated with palliative sedation, the topic continues to garner some controversy. Most clinicians and organizations' chief concern regarding the administration of palliative sedation is that it may inadvertently hasten or quicken someone's demise. Due to this concern, the practice of palliative sedation is still compared with physician-assisted suicide and euthanasia. Below, we will briefly describe the fundamental concept and differences between these therapies in terminally ill patients.[7][19][20]
Euthanasia
Euthanasia constitutes the process by which a health care worker caring for a patient intentionally uses medications to terminate a patient's life to end their pain and suffering. Euthanasia can either be performed with the patient's consent (voluntary euthanasia) or performed independently by the health care providers (involuntary euthanasia). The practice of involuntary euthanasia is illegal in all countries.[19][21]
Physician-Assisted Suicide
Physician-assisted suicide is the process by which a physician acts as a facilitator for a patient to hasten death by providing lethal doses of prescription medication. It differs from euthanasia in that the healthcare worker assumes a passive role of supervision, and the actual administration of medication that leads to death has to be done by the patients on their own.[22]
In the United States, physician-assisted suicide is legal in some states but not all. In these states, "death with dignity" statutes ensure that the adult is mentally competent, is a state resident who has a terminal illness with a confirmed prognosis of having 6 or fewer months to live, and can voluntarily request a prescription for medication that hastens death.[23]
Differentiating Palliative Sedation from Euthanasia and Physician-assisted Suicide
Palliative sedation as a practice differs from euthanasia and physician-assisted suicide on 2 fronts: intention and the desired outcome. Palliative sedation intends to relieve refractory symptoms in dying patients, whereas the intention of physician-assisted suicide and euthanasia is the termination of a patient's life. Similarly, the desired outcome of palliative sedation is to achieve a level of sedation in patients that controls their symptoms. Whereas in physician-assisted suicide and euthanasia, the desired outcome is always the death of the patient. Although some healthcare workers still raise ethical concerns regarding its use, palliative sedation is legal in most countries, including the United States.
Preparation
Timing of Palliative Sedation
Determining the most appropriate time to initiate palliative sedation is often a challenging process. Firstly, there are inconsistencies in defining what to label as "refractory symptoms" due to the lack of consensus among clinicians. In general, a refractory symptom is one that has not responded to multiple conventional treatments, and other treatment options that would not cause sedation are unlikely to provide adequate relief within a tolerable time frame or are associated with excessive and intolerable adverse effects.[17] Secondly, as palliative sedation is usually reserved for the end of life of terminally ill patients, determining the prognosis of the disease is an important step in planning for palliative sedation. Prior literature has demonstrated that healthcare workers are not always accurate when predicting the prognosis or estimated timing of decline due to diseases. Thus, labeling a disease as "terminal" and without a cure remains a difficult task for clinicians.[24][25]
Understanding Proportional Treatment and the Doctrine of "Double Effect"
The goal of palliative sedation is to relieve intractable distressing symptoms, not to keep the patient unresponsive or unconscious. Thus, the concept of proportional treatment must be understood while using palliative sedation. Medications such as benzodiazepines, opiates, and antipsychotics are often used to alleviate patients' respiratory distress, agitation, and anxiety and can also cause sedation. However, the dose and frequency with which benzodiazepines, opiates, and antipsychotics should be titrated and always be proportional to the desired clinical benefit, which is relief from suffering and disturbing symptoms. Extreme cases in which a patient has to be given a high dose of sedatives exist when keeping them obtunded is the only way to alleviate their symptoms, eg, extreme agitation or seizures. However, the goal of treatment is adequate relief of symptoms, not to achieve sedation or unconsciousness in its own right.
An additional ethical concept that needs to be understood regarding palliative sedation is the doctrine of "double effect." This doctrine originated from Thomas Aquinas in the 13th century and parallels the principles of beneficence and non-maleficence. [26]
This doctrine asserts the following:
"An action in the pursuit of a good outcome is acceptable, even if it is achieved through means with an unintended but foreseeable negative outcome if that negative outcome is outweighed by the good outcome."
Some recent studies have shown that palliative sedation is safe in terminally ill patients and is not associated with an increased risk of death. However, it is important to highlight the use of potential risks of excess sedation. Palliative sedation can be associated with an increased risk of aspiration, respiratory depression, and worsening agitation due to delirium. These adverse outcomes are unintended effects of therapy and not the primary intended outcome of palliative sedation. Thus, as per the doctrine of "double effect," as long as the patient, family, and physicians are aware of the potential adverse effects coupled with palliative sedation, it can be administered without any hesitation.[27][28][29][28]
Initiating Goals of Care Discussion with Patients, Family Members, or Surrogates
Initiating conversations regarding goals of care with patients with terminal illness and their family members can be challenging. Clinicians and healthcare workers benefit from additional training, including communication skills and navigating challenging and often emotional conversations. They need to identify patients with poor prognoses and refractory symptoms who are likely to benefit from palliative sedation. Prior studies have demonstrated several communication barriers and misconceptions regarding end-of-life issues in physicians and patients/family members.[13][14] There is ample evidence that shows that there is room for improvement when it comes to discussing issues such as reviewing the code status of patients, conveying poor prognosis of the disease, converting to hospice care, and initiating palliative sedation. Due to a lack of consensus regarding the definition of palliative sedation and its indications, there are often misconceptions among patients and family members regarding the use of palliative sedation.[15][16]
Given its close resemblance to euthanasia and physician-assisted suicide, every attempt must be made to delineate the patient's/family's wishes and manage expectations properly. Often, interdisciplinary teams can assist these challenging conversations and will often include the medical providers (including palliative care providers, specialists, and primary care providers), patients, family members (or surrogates), social workers, and chaplains. These conversations need to address the prognosis of the disease and define the specific symptoms that have not abated with standard therapy. The pros and cons of palliative sedation should be explained during this meeting. Potential adverse effects, such as the risk of inadvertently hastening death, aspiration, and excess sedation, must be addressed while clearly expressing the treatment goals, including the relief of intolerable symptoms and suffering.
Discussing Ongoing Care and Obtaining Consent
After a thorough goals-of-care discussion, written or verbal consent must be documented from the patient or surrogate decision-maker regarding their willingness to initiate palliative sedation. For patients who cannot communicate their wishes due to a decreased level of cognitive capacity, consciousness, or nonverbal state, we must follow the patient's advance directives, or if there is no advance directive, consent must be obtained from a legally recognized proxy. Patients and families should be assured that being started on palliative sedation does not imply that any ongoing medical or nursing care that has been beneficial to the patient will be withdrawn by default. Detailed goals of care should address what therapies would be added or continued for the patient's care and those that can be discontinued. For example, there should be a detailed discussion regarding issues such as feeding and artificial nutrition in terminally ill patients. Clinicians should clearly explain the prognosis and life expectancy and discuss with patients/family members whether it is prudent to continue feeding tubes and nutrition or to discontinue it entirely to limit patient distress (mainly if life expectancy is in the range of hours to days).
Technique or Treatment
Pharmacology
The following are the common pharmacological agents that can be used in palliative sedation.[30][31][32][33]
|
Drug Class |
Mechanism of Action |
Indication |
Adverse Effects |
|
Benzodiazepines, eg, lorazepam, midazolam |
GABA agonist with CNS depression.
|
Agitated delirium, anxiety.
|
Worsening of delirium, confusion, and agitation. When administered with other agents, such as opioids, it can cause respiratory depression. |
|
Antipsychotics (first generation), eg, haloperidol, chlorpromazine.
|
Greater dopamine 2 receptor antagonism with high potency first-generation antipsychotics (eg, haloperidol) and serotonin, histamine, alpha, and a muscarinic receptor antagonism with low potency antipsychotics (eg, chlorpromazine). |
Agitated delirium.
|
Anticholinergic effects, orthostatic hypotension (which can be severe) with rapid IV administration, akathisia, acute dystonic reactions, seizures, and cardiotoxicity associated with QT prolongation.
|
|
Propofol
|
GABA agonist and potentially by inhibition of glutamate.
|
For agitated delirium in patients with poor response to antipsychotics and benzodiazepines. |
Hypotension, thrombophlebitis, propofol infusion syndrome.
|
|
Barbiturates
|
GABA agonist and inhibition of glutamate.
|
For agitated delirium in patients with poor response to antipsychotics and benzodiazepines. |
Hemodynamic instability (low blood pressure and heart rate), nausea, vomiting. Enzyme induction and resultant decreased efficacy of other drugs. |
|
Opioids, eg, morphine, fentanyl, oxycodone |
Binds to opioid receptors (eg, mu) in the CNS and causes CNS depression.
|
For pain relief and respiratory distress.
|
Can lead to respiratory depression. |
Respite Sedation vs Continuous Sedation
Respite sedation refers to the temporary use of sedative agents to relieve symptoms such as pain, nausea, and agitation. These symptoms may or may not be refractory. Patients are typically started on sedative agents for a brief, predetermined period (eg, 1 to 48 h) with frequent reassessment. The dose of the sedating agent is then decreased until the patient is fully conscious after the predetermined period.
Most patients with a terminal illness and refractory pain who have shown poor response to conventional therapy are placed on continuous sedation. As the name suggests, with this form of sedation, no attempt is made to wean the sedative medication off, and it is typically continued until the patient's demise.
Complications
The use of palliative sedation continues to be a controversial topic, given that its use can potentially hasten death. As such, the pros and cons of palliative sedation should be clearly outlined to the patient/family to manage expectations. Excess sedation can theoretically cause an increased risk of aspiration pneumonia and respiratory suppression. However, contrary to this belief, recent studies have demonstrated that palliative sedation can be safely administered without any disproportionate increase in the incidence of aspiration pneumonia or respiratory failure.[34][35][34] Additionally, other studies have demonstrated that the time till death is not significantly shortened in patients receiving palliative sedation compared to patients receiving standard or alternative therapy.[36][37]
Clinical Significance
Identifying terminally ill patients with refractory symptoms and the timely initiation of goals-of-care discussions are paramount to patient care. This will not only ensure that the patient's wishes are honored but also assist in withholding any redundant therapies or invasive procedures that are unlikely to improve the patient's symptoms or delay disease progression. Prior studies have demonstrated that palliative care has enormous benefits in patients beyond just pain control. These studies reveal that providing interprofessional care and family meetings enhances the bond between the patient, family, and caregivers and relieves stress, anxiety, and frustration.[38][39]
Enhancing Healthcare Team Outcomes
Providing palliative care requires an interprofessional team approach. It includes managing a broad range of refractory symptoms, including shortness of breath, agitation, delirium, and pain. Currently, most healthcare institutions have a palliative care management team that assesses patients for their palliative care needs. The team usually consists of a physician, nurse, pharmacist, pain specialist, religious figure, and ethics committee members. Palliative care should be individualized for each patient based on goals of care discussions with the patient and family. Nurses and pharmacists are vital team members as they closely monitor the patient for adverse effects and effectiveness of the sedative medications. In addition to pharmacological methods to relieve pain, several nonpharmacological methods are available. Some of these nonpharmacological methods are radiation therapy, radiofrequency ablation, heat, ice, or coolant sprays, and may warrant the inclusion of other specialties such as pain medicine and radiation oncology.
Media
References
Sulmasy DP. Sedation and care at the end of life. Theoretical medicine and bioethics. 2018 Jun:39(3):171-180. doi: 10.1007/s11017-018-9441-4. Epub [PubMed PMID: 29967981]
Bobb B. A Review of Palliative Sedation. The Nursing clinics of North America. 2016 Sep:51(3):449-57. doi: 10.1016/j.cnur.2016.05.008. Epub [PubMed PMID: 27497018]
Patel C, Kleinig P, Bakker M, Tait P. Palliative sedation: A safety net for the relief of refractory and intolerable symptoms at the end of life. Australian journal of general practice. 2019 Dec:48(12):838-845. doi: 10.31128/AJGP-05-19-4938. Epub [PubMed PMID: 31774984]
Garetto F, Cancelli F, Rossi R, Maltoni M. Palliative Sedation for the Terminally Ill Patient. CNS drugs. 2018 Oct:32(10):951-961. doi: 10.1007/s40263-018-0576-7. Epub [PubMed PMID: 30259395]
Maltoni M, Scarpi E, Rosati M, Derni S, Fabbri L, Martini F, Amadori D, Nanni O. Palliative sedation in end-of-life care and survival: a systematic review. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2012 Apr 20:30(12):1378-83. doi: 10.1200/JCO.2011.37.3795. Epub 2012 Mar 12 [PubMed PMID: 22412129]
Level 2 (mid-level) evidenceMiccinesi G, Caraceni A, Maltoni M. Palliative sedation: ethical aspects. Minerva anestesiologica. 2017 Dec:83(12):1317-1323. doi: 10.23736/S0375-9393.17.12091-2. Epub 2017 Jul 12 [PubMed PMID: 28707846]
Curlin FA. Palliative sedation: clinical context and ethical questions. Theoretical medicine and bioethics. 2018 Jun:39(3):197-209. doi: 10.1007/s11017-018-9446-z. Epub [PubMed PMID: 30136127]
Claessens P, Menten J, Schotsmans P, Broeckaert B. Palliative sedation: a review of the research literature. Journal of pain and symptom management. 2008 Sep:36(3):310-33. doi: 10.1016/j.jpainsymman.2007.10.004. Epub 2008 Jul 25 [PubMed PMID: 18657380]
Level 1 (high-level) evidenceMyers J, Cosby R, Gzik D, Harle I, Harrold D, Incardona N, Walton T. Provider Tools for Advance Care Planning and Goals of Care Discussions: A Systematic Review. The American journal of hospice & palliative care. 2018 Aug:35(8):1123-1132. doi: 10.1177/1049909118760303. Epub 2018 Mar 12 [PubMed PMID: 29529884]
Level 1 (high-level) evidenceChilders JW, Back AL, Tulsky JA, Arnold RM. REMAP: A Framework for Goals of Care Conversations. Journal of oncology practice. 2017 Oct:13(10):e844-e850. doi: 10.1200/JOP.2016.018796. Epub 2017 Apr 26 [PubMed PMID: 28445100]
Kaldjian LC, Curtis AE, Shinkunas LA, Cannon KT. Goals of care toward the end of life: a structured literature review. The American journal of hospice & palliative care. 2008 Dec-2009 Jan:25(6):501-11. doi: 10.1177/1049909108328256. Epub [PubMed PMID: 19106284]
Benítez-Rosario MA, Morita T. Palliative sedation in clinical scenarios: results of a modified Delphi study. Supportive care in cancer : official journal of the Multinational Association of Supportive Care in Cancer. 2019 May:27(5):1647-1654. doi: 10.1007/s00520-018-4409-5. Epub 2018 Aug 10 [PubMed PMID: 30094733]
Spineli VM, Kurashima AY, De Gutiérrez MG. The process of palliative sedation as viewed by physicians and nurses working in palliative care in Brazil. Palliative & supportive care. 2015 Oct:13(5):1293-9. doi: 10.1017/S1478951514001278. Epub 2014 Oct 31 [PubMed PMID: 25359102]
Benítez-Rosario MA, Ascanio-León B. Palliative sedation: beliefs and decision-making among Spanish palliative care physicians. Supportive care in cancer : official journal of the Multinational Association of Supportive Care in Cancer. 2020 Jun:28(6):2651-2658. doi: 10.1007/s00520-019-05086-4. Epub 2019 Oct 21 [PubMed PMID: 31637516]
Duhamel F, Dupuis F. Families in palliative care: exploring family and health-care professionals' beliefs. International journal of palliative nursing. 2003 Mar:9(3):113-9 [PubMed PMID: 12682573]
Taber JM, Ellis EM, Reblin M, Ellington L, Ferrer RA. Knowledge of and beliefs about palliative care in a nationally-representative U.S. sample. PloS one. 2019:14(8):e0219074. doi: 10.1371/journal.pone.0219074. Epub 2019 Aug 15 [PubMed PMID: 31415570]
Cherny NI, Portenoy RK. Sedation in the management of refractory symptoms: guidelines for evaluation and treatment. Journal of palliative care. 1994 Summer:10(2):31-8 [PubMed PMID: 8089815]
Bruera E. Patient assessment in palliative cancer care. Cancer treatment reviews. 1996 Jan:22 Suppl A():3-12 [PubMed PMID: 8625346]
ten Have H, Welie JV. Palliative sedation versus euthanasia: an ethical assessment. Journal of pain and symptom management. 2014 Jan:47(1):123-36. doi: 10.1016/j.jpainsymman.2013.03.008. Epub 2013 Jun 4 [PubMed PMID: 23742736]
Olsen ML, Swetz KM, Mueller PS. Ethical decision making with end-of-life care: palliative sedation and withholding or withdrawing life-sustaining treatments. Mayo Clinic proceedings. 2010 Oct:85(10):949-54. doi: 10.4065/mcp.2010.0201. Epub 2010 Aug 30 [PubMed PMID: 20805544]
Hahn MP. Review of palliative sedation and its distinction from euthanasia and lethal injection. Journal of pain & palliative care pharmacotherapy. 2012:26(1):30-9. doi: 10.3109/15360288.2011.650353. Epub [PubMed PMID: 22448939]
Level 3 (low-level) evidenceEly EW. Ethics and the Legalization of Physician-Assisted Suicide. Annals of internal medicine. 2018 Jun 5:168(11):834. doi: 10.7326/L18-0078. Epub [PubMed PMID: 29868807]
Emanuel EJ, Onwuteaka-Philipsen BD, Urwin JW, Cohen J. Attitudes and Practices of Euthanasia and Physician-Assisted Suicide in the United States, Canada, and Europe. JAMA. 2016 Jul 5:316(1):79-90. doi: 10.1001/jama.2016.8499. Epub [PubMed PMID: 27380345]
Christakis NA, Lamont EB. Extent and determinants of error in physicians' prognoses in terminally ill patients: prospective cohort study. The Western journal of medicine. 2000 May:172(5):310-3 [PubMed PMID: 18751282]
White N, Reid F, Harris A, Harries P, Stone P. A Systematic Review of Predictions of Survival in Palliative Care: How Accurate Are Clinicians and Who Are the Experts? PloS one. 2016:11(8):e0161407. doi: 10.1371/journal.pone.0161407. Epub 2016 Aug 25 [PubMed PMID: 27560380]
Level 1 (high-level) evidenceLatham SR. Aquinas and morphine: notes on double effect at the end of life. DePaul journal of health care law. 1997 Spring:1(3):625-44 [PubMed PMID: 15282891]
Gillon R. The principle of double effect and medical ethics. British medical journal (Clinical research ed.). 1986 Jan 18:292(6514):193-4 [PubMed PMID: 3080130]
Lindblad A, Lynöe N, Juth N. End-of-life decisions and the reinvented Rule of Double Effect: a critical analysis. Bioethics. 2014 Sep:28(7):368-77. doi: 10.1111/bioe.12001. Epub 2012 Oct 1 [PubMed PMID: 23025921]
Belar A, Arantzamendi M, Payne S, Preston N, Rijpstra M, Hasselaar J, Radbruch L, Vanderelst M, Ling J, Centeno C. How to measure the effects and potential adverse events of palliative sedation? An integrative review. Palliative medicine. 2021 Feb:35(2):295-314. doi: 10.1177/0269216320974264. Epub 2020 Dec 14 [PubMed PMID: 33307989]
Bodnar J. A Review of Agents for Palliative Sedation/Continuous Deep Sedation: Pharmacology and Practical Applications. Journal of pain & palliative care pharmacotherapy. 2017 Mar:31(1):16-37. doi: 10.1080/15360288.2017.1279502. Epub 2017 Mar 1 [PubMed PMID: 28287357]
Prommer E. Midazolam: an essential palliative care drug. Palliative care and social practice. 2020:14():2632352419895527. doi: 10.1177/2632352419895527. Epub 2020 Jan 13 [PubMed PMID: 32215374]
Truog RD, Berde CB, Mitchell C, Grier HE. Barbiturates in the care of the terminally ill. The New England journal of medicine. 1992 Dec 3:327(23):1678-82 [PubMed PMID: 1279424]
Level 3 (low-level) evidenceHui D, Dev R, Bruera E. Neuroleptics in the management of delirium in patients with advanced cancer. Current opinion in supportive and palliative care. 2016 Dec:10(4):316-323 [PubMed PMID: 27661210]
Level 3 (low-level) evidenceMorita T, Chinone Y, Ikenaga M, Miyoshi M, Nakaho T, Nishitateno K, Sakonji M, Shima Y, Suenaga K, Takigawa C, Kohara H, Tani K, Kawamura Y, Matsubara T, Watanabe A, Yagi Y, Sasaki T, Higuchi A, Kimura H, Abo H, Ozawa T, Kizawa Y, Uchitomi Y, Japan Pain, Palliative Medicine, Rehabilitation, and Psycho-Oncology Study Group. Efficacy and safety of palliative sedation therapy: a multicenter, prospective, observational study conducted on specialized palliative care units in Japan. Journal of pain and symptom management. 2005 Oct:30(4):320-8 [PubMed PMID: 16256896]
Level 2 (mid-level) evidenceSimon ST, Mori M, Ekström M, Pralong A, Yamaguchi T, Hui D. Should Benzodiazepines be Used for Reducing Dyspnea in Patients with Advanced Illnesses? Journal of pain and symptom management. 2023 Mar:65(3):e219-e223. doi: 10.1016/j.jpainsymman.2022.11.018. Epub 2022 Nov 29 [PubMed PMID: 36455801]
Maltoni M, Pittureri C, Scarpi E, Piccinini L, Martini F, Turci P, Montanari L, Nanni O, Amadori D. Palliative sedation therapy does not hasten death: results from a prospective multicenter study. Annals of oncology : official journal of the European Society for Medical Oncology. 2009 Jul:20(7):1163-9. doi: 10.1093/annonc/mdp048. Epub [PubMed PMID: 19542532]
Level 2 (mid-level) evidenceSchur S, Weixler D, Gabl C, Kreye G, Likar R, Masel EK, Mayrhofer M, Reiner F, Schmidmayr B, Kirchheiner K, Watzke HH, AUPACS (Austrian Palliative Care Study) Group. Sedation at the end of life - a nation-wide study in palliative care units in Austria. BMC palliative care. 2016 May 14:15():50. doi: 10.1186/s12904-016-0121-8. Epub 2016 May 14 [PubMed PMID: 27180238]
Tursunov O, Cherny NI, Ganz FD. Experiences of Family Members of Dying Patients Receiving Palliative Sedation. Oncology nursing forum. 2016 Nov 1:43(6):E226-E232 [PubMed PMID: 27768142]
Morita T, Ikenaga M, Adachi I, Narabayashi I, Kizawa Y, Honke Y, Kohara H, Mukaiyama T, Akechi T, Uchitomi Y, Japan Pain, Rehabilitation, Palliative Medicine, and Psycho-Oncology Study Group. Family experience with palliative sedation therapy for terminally ill cancer patients. Journal of pain and symptom management. 2004 Dec:28(6):557-65 [PubMed PMID: 15645586]