Doppler Extra-Cranial Carotid Assessment, Protocols, and Interpretation
Doppler Extra-Cranial Carotid Assessment, Protocols, and Interpretation
Introduction
Over the past few decades, Doppler ultrasound has become a primary modality for extracranial carotid assessment because it is readily available, non-invasive, and relatively inexpensive. [1] The sonographic evaluation of extracranial carotids is done for screening, diagnosis, and monitoring of atherosclerotic disease, as well as post-intervention analysis. [2] The evaluation is crucial since the stroke risk increases with the degree of atherosclerotic narrowing leading to flow disturbances. [3] Doppler imaging provides a quantitative assessment of velocity, which in combination with grayscale imaging provides a qualitative and quantitative assessment of plaque and stenosis. This is of utmost clinical importance for stroke risk stratification as well as providing indications for surgical intervention. [4]
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
Extracranial vessels represent vessels outside the brain and skull. The most common configuration is the three-vessel arch anatomy, where the first branch is the brachiocephalic artery which further branches into the right common carotid artery (CCA) and right subclavian artery. The second branch is the left CCA, with the left subclavian artery as the third branch. [5]
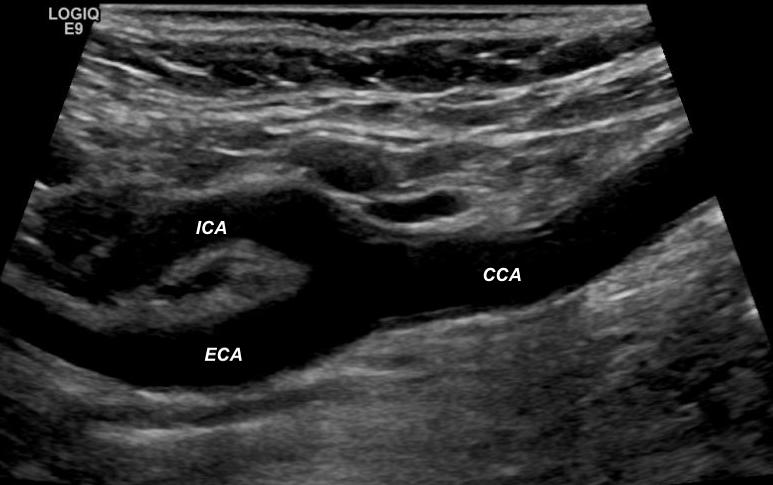
The most common variant to this anatomy is the common origin of the brachiocephalic artery and left CCA from the aortic arch. The common carotid arteries bifurcate into the external carotid artery (ECA) and internal carotid artery (ICA) at the upper border of the thyroid. The carotid bulb is the location of a bifurcation and the ICA origin. [6] ICA is generally posterior and lateral to ECA and is usually bigger in caliber compared to ECA (Figure 1). ECA supplies the musculature of the face and neck and tapers distally, giving off extracranial branches.[7]
Indications
Indications for extracranial carotid doppler ultrasound include hemispheric or nonhemispheric neurologic symptoms, cervical bruit, pulsatile neck mass, preoperative evaluation for major cardiovascular surgery, follow-up of known carotid disease, and subclavian steal syndrome.[8]
Equipment
Since carotid vessels are superficial, a high-frequency linear transducer operating between 5.0 to 7.5 MHz is used. This is because the frequency of the ultrasound probe is inversely proportional to the depth of insonation. Doppler US is usually performed in combination with grayscale imaging. Grayscale images are obtained with a 5.0 to 12.0 MHz transducer.
Preparation
The patient should be placed supine with head slightly extended and turned 45 degrees away from the examined side. The sonographer position is based on individual preference; some prefer to sit behind the patient’s head facing caudally, while others may prefer sitting to the side facing superiorly. The patient’s bed height should be adjusted according to the sonographer’s comfort to avoid hunching over.
Technique or Treatment
The technique is built on the principle of the Doppler effect, with measurement of the change in the frequency and wavelength of a sound wave transmitted and reflected by moving red blood cells within the vessel, termed as Doppler frequency shift. [9] Velocity is calculated using the Doppler formula, where frequency shift is proportional to the velocity times the cosine of the Doppler angle.[10] This allows the determination of the speed and direction of the flow. Grayscale imaging, which is also called B (brightness)-mode, is usually performed first, where carotid arteries are evaluated in their entirety from the jugular notch to the angle of the mandible in the transverse and longitudinal plane. [11] B-mode imaging evaluates the course and caliber of the vessel with the evaluation of intimal-media thickness and quality of plaque. The morphology of plaque is associated with the severity of atherosclerotic disease. The vulnerable plaques are more prone to rupture and acute thrombosis. The plaque echogenicity, surface characteristic (i.e., regular vs. irregular), and presence of calcification should be assessed and reported. [12] The time-gain compensation should be optimized to account for ultrasound attenuation from deeper structures. Some vessels, especially if they are tortuous, require the angle of the probe to be adjusted accordingly. At the jugular notch, the transducer is angulated causally, while at the angle of the mandible, it is cephalic angulated. This is then followed by the Doppler examination.[13][14]
There are many parameters that should be optimally adjusted to achieve reliable results. The actual angle of insonation / Doppler angle should be less than <60 degrees (as close as possible to parallel) to improve the accuracy of measurements (the calculated velocity will be less precise if calculated/extrapolated from a nearly perpendicular angle). [15] The technologist needs to correctly set the angle correction parallel to the flow direction to correctly calculate the velocity (the calculated velocity will be incorrect if calculated using an inaccurate angle, not corresponding to flow direction). The velocity of the common carotid artery is usually 30-40 cm/sec but may vary in a diseased vessel. [16] Gain is adjusted so that color is seen only within the lumen of the vessel to avoid bleeding artifact. [17] Sample volume should be placed into the center of the lumen and should be moved along the entire vessel. Color Doppler should be evaluated at the minimum at (a) “long axis of the distal common carotid artery” (b) “long axis of proximal and mid internal carotid artery” (c) “long axis of the external carotid artery” (d) “long axis of the vertebral artery.” Any abrupt change in the systolic velocity or area of slow flow should be carefully evaluated and documented.[8][18]
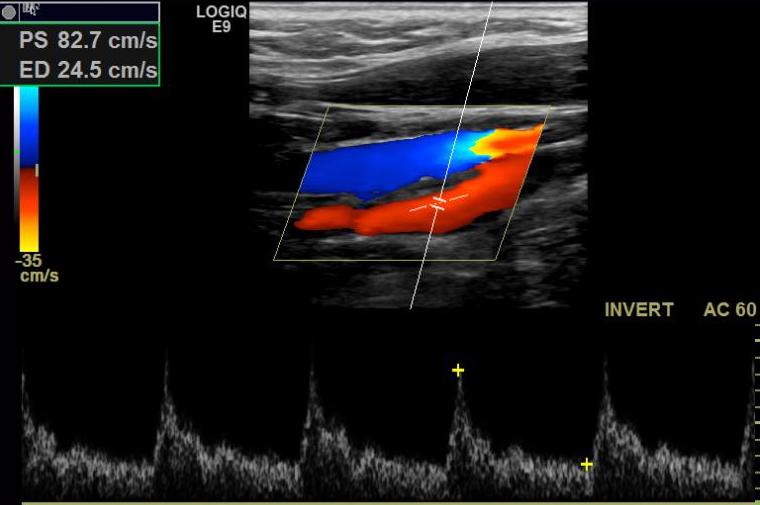
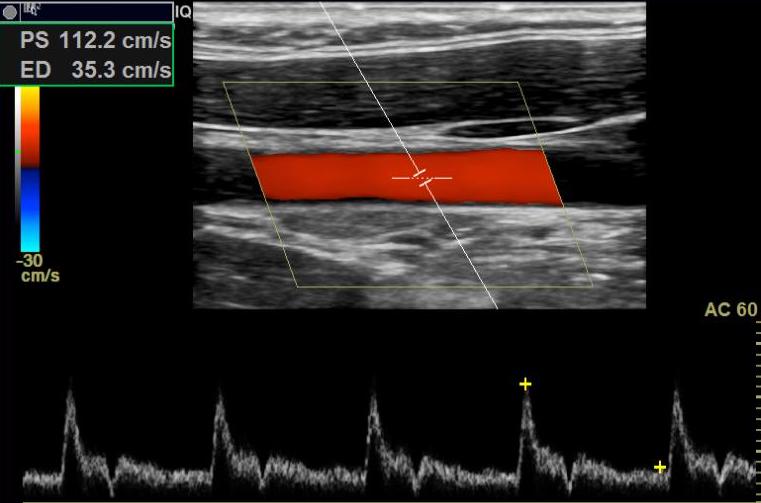
Spectral analysis including peak systolic velocity (PSV), peak diastolic velocity (PDV), mean maximum velocity, and pulsatility index can then be obtained. Spectral Doppler waveform evaluation gives critical information about flow dynamics at the point of sampling, which depends on hemodynamic factors affecting a proximal or distal portion of the vessel. [19] ICA demonstrates low resistance flow, ECA has high resistance flow, while CCA has a hybrid of ICA and ECA (Figure 2, 3, 4). The resistive index is the term used to describe waveforms, which signifies resistance of the vessel distal to the examined vessel. [20] The Pulsus Parvus and Pulsus Tardus waveform results from delayed and diminished arterial pulsation and is observed distal to stenosis in 91% of cases. [21] Pulsus Bisferiens denotes two prominent systolic peaks with mid systolic retraction and is usually found in hypertrophic cardiomyopathy and aortic valvular disease. [22][22] Alternating peak systolic height in line with cardiac rhythm is called pulsus alternans, which can be seen in myocardial disease, metabolic disease, or IVC compression. [23]
With complete occlusion of ICA, the external carotid doppler waveform can change from high resistance to low resistance due to the development of low resistance collateral pathways. This is known as the internalization of the external carotid. [24] Patients with severe aortic regurgitation typically have water hammer spectral appearance of common carotid with sharp systolic peak and deceleration of flow in late systole and reversal of flow in diastole. [25] Spectral doppler should be evaluated at a minimum at (a) proximal, mid, and distal common carotid artery (b) proximal, mid, and distal internal carotid artery (c) proximal carotid artery (d) vertebral artery. Any significant stenosis should be carefully evaluated and documented distal and proximal to the stenosis.[26][24][27]
Peak systolic velocity of greater than 125 cm/s correlates with 50% or higher ICA stenosis. [28] PSV greater than 230 cm/s correlates with 70% or higher stenosis, a potential indication for surgical endarterectomy. Secondary criteria for stratification include ICA/CCA PSV ratios greater than 2.0 and 4.0. The degrees of stenosis derived above are expressed as percentage per North American Symptomatic Carotid Endarterectomy Trial (NASCET) criteria. [29] Percent stenosis is defined as (normal distal vessel diameter - luminal diameter at stenosis ) / normal distal vessel diameter. Using the expected luminal diameter of a stenotic carotid bulb for the denominator would calculate a higher numerical measurement of the stenosis.[30][31]
The final assessment is done on vertebral arteries to determine the direction of flow. Vertebral arteries are located deep in the neck. Therefore, time gain compensation should be optimized. [32] They are found by directing the beam posteriorly and laterally between the vertebral foramen and turning the color and pulsed Doppler. The flow in the vertebral artery should be the same as the common carotid artery, i.e., antegrade. It is a low resistance vessel with prominent diastolic flow and spectral broadening. Any change in normal flow gives indirect evidence of occlusion or near occlusion of more proximal vessels such as a subclavian or brachiocephalic artery. Three types of patterns known as “subclavian steal” can be described. [33] [34]The flow can be antegrade with mid-systolic deceleration ("pre-steal") and may convert to reversed late systolic flow with ipsilateral arm exercise. Systolic flow reversal is seen with a partial subclavian steal, while with a complete subclavian steal, the flow is completely reversed throughout systole and diastole. By comparing the flow in vertebral and carotid arteries from the left to the right side, the location of stenosis can be determined.[27] CT angiography potentially has a greater capacity to grade vertebral artery stenosis when compared to ultrasound. [35]
Clinical Significance
Stroke is the third leading cause of death and major disability in the united states. Atherosclerosis of extracranial and intracranial cerebral arteries has been identified as the major cause of ischemic stroke. The evaluation of atherosclerotic burden, therefore, is very crucial for stroke risk stratification. Grayscale ultrasound imaging combined with color Doppler and spectral waveform analysis is a widely available tool that can assess the morphology of plaques and detect hemodynamically significant stenosis. Besides the screening, doppler examination of extracranial carotid is also beneficial to evaluate the potential complications of vascular interventions such as pseudoaneurysm formation, restenosis of carotid arteries, fistula formation, and stent deformation and fracture.
Enhancing Healthcare Team Outcomes
Stroke risk stratification through evaluation of extracranial arterial atherosclerotic burden has proven to be beneficial with improved outcomes. This requires an interprofessional team, including primary care provider/internist, mid-level practitioners (PAs and MPs), interventional radiologist, vascular surgeon, neurologist, and ultrasound technologist. Communication between these health professionals is crucial for patient-centered care. [Level 5]
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Sigel B. A brief history of Doppler ultrasound in the diagnosis of peripheral vascular disease. Ultrasound in medicine & biology. 1998 Feb:24(2):169-76 [PubMed PMID: 9550175]
Fleming SE, Bluth EI, Milburn J. Role of sonography in the evaluation of carotid artery stents. Journal of clinical ultrasound : JCU. 2005 Sep:33(7):321-8 [PubMed PMID: 16196004]
Level 2 (mid-level) evidenceFlaherty ML, Kissela B, Khoury JC, Alwell K, Moomaw CJ, Woo D, Khatri P, Ferioli S, Adeoye O, Broderick JP, Kleindorfer D. Carotid artery stenosis as a cause of stroke. Neuroepidemiology. 2013:40(1):36-41. doi: 10.1159/000341410. Epub 2012 Oct 11 [PubMed PMID: 23075828]
Nezu T, Hosomi N. Usefulness of Carotid Ultrasonography for Risk Stratification of Cerebral and Cardiovascular Disease. Journal of atherosclerosis and thrombosis. 2020 Oct 1:27(10):1023-1035. doi: 10.5551/jat.RV17044. Epub 2020 Aug 29 [PubMed PMID: 32863299]
Kau T, Sinzig M, Gasser J, Lesnik G, Rabitsch E, Celedin S, Eicher W, Illiasch H, Hausegger KA. Aortic development and anomalies. Seminars in interventional radiology. 2007 Jun:24(2):141-52. doi: 10.1055/s-2007-980040. Epub [PubMed PMID: 21326792]
Dungan DH, Heiserman JE. The carotid artery: embryology, normal anatomy, and physiology. Neuroimaging clinics of North America. 1996 Nov:6(4):789-99 [PubMed PMID: 8824131]
Schulz UG, Rothwell PM. Major variation in carotid bifurcation anatomy: a possible risk factor for plaque development? Stroke. 2001 Nov:32(11):2522-9 [PubMed PMID: 11692011]
. AIUM Practice Parameter for the Performance of an Ultrasound Examination of the Extracranial Cerebrovascular System. Journal of ultrasound in medicine : official journal of the American Institute of Ultrasound in Medicine. 2016 Sep:35(9):1-11. doi: 10.7863/ultra.35.9.1. Epub [PubMed PMID: 27574121]
FRANKLIN DL, SCHLEGEL W, RUSHMER RF. Blood flow measured by Doppler frequency shift of back-scattered ultrasound. Science (New York, N.Y.). 1961 Aug 25:134(3478):564-5 [PubMed PMID: 13701432]
Level 3 (low-level) evidenceBurns PN. The physical principles of Doppler and spectral analysis. Journal of clinical ultrasound : JCU. 1987 Nov-Dec:15(9):567-90 [PubMed PMID: 2960698]
Crişan S. Carotid ultrasound. Medical ultrasonography. 2011 Dec:13(4):326-30 [PubMed PMID: 22132407]
Scoutt LM, Gunabushanam G. Carotid Ultrasound. Radiologic clinics of North America. 2019 May:57(3):501-518. doi: 10.1016/j.rcl.2019.01.008. Epub 2019 Feb 22 [PubMed PMID: 30928074]
Park TH. Evaluation of Carotid Plaque Using Ultrasound Imaging. Journal of cardiovascular ultrasound. 2016 Jun:24(2):91-5. doi: 10.4250/jcu.2016.24.2.91. Epub 2016 Jun 22 [PubMed PMID: 27358696]
Lafont A. Basic aspects of plaque vulnerability. Heart (British Cardiac Society). 2003 Oct:89(10):1262-7 [PubMed PMID: 12975444]
Logason K, Bärlin T, Jonsson ML, Boström A, Hårdemark HG, Karacagil S. The importance of Doppler angle of insonation on differentiation between 50-69% and 70-99% carotid artery stenosis. European journal of vascular and endovascular surgery : the official journal of the European Society for Vascular Surgery. 2001 Apr:21(4):311-3 [PubMed PMID: 11359330]
Meyer JI, Khalil RM, Obuchowski NA, Baus LK. Common carotid artery: variability of Doppler US velocity measurements. Radiology. 1997 Aug:204(2):339-41 [PubMed PMID: 9240517]
Saad AA, Loupas T, Shapiro LG. Computer vision approach for ultrasound Doppler angle estimation. Journal of digital imaging. 2009 Dec:22(6):681-8. doi: 10.1007/s10278-008-9131-2. Epub 2008 May 17 [PubMed PMID: 18488268]
Tahmasebpour HR, Buckley AR, Cooperberg PL, Fix CH. Sonographic examination of the carotid arteries. Radiographics : a review publication of the Radiological Society of North America, Inc. 2005 Nov-Dec:25(6):1561-75 [PubMed PMID: 16284135]
Zwiebel WJ. Spectrum analysis in carotid sonography. Ultrasound in medicine & biology. 1987 Oct:13(10):625-36 [PubMed PMID: 3318070]
Frauchiger B, Schmid HP, Roedel C, Moosmann P, Staub D. Comparison of carotid arterial resistive indices with intima-media thickness as sonographic markers of atherosclerosis. Stroke. 2001 Apr:32(4):836-41 [PubMed PMID: 11283379]
Level 1 (high-level) evidencePark JH, Shin JW, Lee JH. Unilateral Pulsus Parvus et Tardus Waveform Discovered during Carotid Artery Doppler Examination: a Clue of Proximal Carotid Artery Occlusion. Korean circulation journal. 2019 Dec:49(12):1203-1205. doi: 10.4070/kcj.2019.0178. Epub [PubMed PMID: 31760708]
Goudar RB, ElBebawy B. Pulsus Bisferiens. StatPearls. 2023 Jan:(): [PubMed PMID: 33085355]
Walker HK, Hall WD, Hurst JW, Morris DC. The Carotid Pulse. Clinical Methods: The History, Physical, and Laboratory Examinations. 1990:(): [PubMed PMID: 21250154]
Rohren EM, Kliewer MA, Carroll BA, Hertzberg BS. A spectrum of Doppler waveforms in the carotid and vertebral arteries. AJR. American journal of roentgenology. 2003 Dec:181(6):1695-704 [PubMed PMID: 14627599]
Chirinos JA, Akers SR, Vierendeels JA, Segers P. A Unified Mechanism for the Water Hammer Pulse and Pulsus Bisferiens in Severe Aortic Regurgitation: Insights from Wave Intensity Analysis. Artery research. 2018 Mar:21():9-12. doi: 10.1016/j.artres.2017.12.002. Epub 2017 Dec 21 [PubMed PMID: 29576810]
Ginat DT, Bhatt S, Sidhu R, Dogra V. Carotid and vertebral artery Doppler ultrasound waveforms: a pictorial review. Ultrasound quarterly. 2011 Jun:27(2):81-5. doi: 10.1097/RUQ.0b013e31821c7f6a. Epub [PubMed PMID: 21606790]
Horrow MM, Stassi J. Sonography of the vertebral arteries: a window to disease of the proximal great vessels. AJR. American journal of roentgenology. 2001 Jul:177(1):53-9 [PubMed PMID: 11418397]
Kronick MD, Chopra A, Swamy S, Brar V, Jung E, Abraham CZ, Liem TK, Landry GJ, Moneta GL. Peak systolic velocity and color aliasing are important in the development of duplex ultrasound criteria for external carotid artery stenosis. Journal of vascular surgery. 2020 Sep:72(3):951-957. doi: 10.1016/j.jvs.2019.10.099. Epub 2020 Jan 19 [PubMed PMID: 31964570]
Ferguson GG, Eliasziw M, Barr HW, Clagett GP, Barnes RW, Wallace MC, Taylor DW, Haynes RB, Finan JW, Hachinski VC, Barnett HJ. The North American Symptomatic Carotid Endarterectomy Trial : surgical results in 1415 patients. Stroke. 1999 Sep:30(9):1751-8 [PubMed PMID: 10471419]
Level 1 (high-level) evidenceGrant EG, Benson CB, Moneta GL, Alexandrov AV, Baker JD, Bluth EI, Carroll BA, Eliasziw M, Gocke J, Hertzberg BS, Katanick S, Needleman L, Pellerito J, Polak JF, Rholl KS, Wooster DL, Zierler RE. Carotid artery stenosis: gray-scale and Doppler US diagnosis--Society of Radiologists in Ultrasound Consensus Conference. Radiology. 2003 Nov:229(2):340-6 [PubMed PMID: 14500855]
Level 3 (low-level) evidenceNorth American Symptomatic Carotid Endarterectomy Trial Collaborators, Barnett HJM, Taylor DW, Haynes RB, Sackett DL, Peerless SJ, Ferguson GG, Fox AJ, Rankin RN, Hachinski VC, Wiebers DO, Eliasziw M. Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. The New England journal of medicine. 1991 Aug 15:325(7):445-53 [PubMed PMID: 1852179]
Level 1 (high-level) evidenceGrogan SP, Mount CA. Ultrasound Physics and Instrumentation. StatPearls. 2023 Jan:(): [PubMed PMID: 34033355]
Osiro S, Zurada A, Gielecki J, Shoja MM, Tubbs RS, Loukas M. A review of subclavian steal syndrome with clinical correlation. Medical science monitor : international medical journal of experimental and clinical research. 2012 May:18(5):RA57-63 [PubMed PMID: 22534720]
Liljeqvist L, Ekeström S, Nordhus O. Monitoring direction of vertebral artery blood flow by Doppler shift ultrasound in patients with suspected "subclavian steal'. Acta chirurgica Scandinavica. 1981:147(6):421-4 [PubMed PMID: 7324774]
Khan S, Cloud GC, Kerry S, Markus HS. Imaging of vertebral artery stenosis: a systematic review. Journal of neurology, neurosurgery, and psychiatry. 2007 Nov:78(11):1218-25 [PubMed PMID: 17287234]
Level 1 (high-level) evidence