Nuclear Medicine Pediatric Assessment, Protocols, and Interpretation
Nuclear Medicine Pediatric Assessment, Protocols, and Interpretation
Introduction
Pediatric imaging relies heavily on morphological imaging using mostly nonionizing radiation techniques such as ultrasound (US) and magnetic resonance imaging (MRI). Computed tomography (CT) and nuclear medicine (NM) techniques still hold value and are used in high-yield indications. Although nuclear medicine exams have been around for a century, it is only with recent software and hardware improvements that they have gained an impactful clinical role.
Even though the Society for Nuclear Medicine was founded in 1954, the pediatric nuclear medicine organization known nowadays as the Pediatric Council was only created in the 1970s; we can date to 1946 an NRC report in pediatrics looking at radioisotopes in thyroid pathology. The American medical association (AMA) recognized nuclear medicine as an independent specialty in 1971, leading to the creation of the American Board of Nuclear Medicine (ABNM). The various modalities of nuclear medicine in children have led to prompt diagnosis, selection of appropriate procedures, and treatment resulting in improved outcomes.
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
Children do not act as a scaled-down version of adults. They are unique in terms of anatomy, physiology, and pathology. The biology can be different even within the same disease type. For similar pathology, age can also be a critical prognostic determinant. Radiation exposure is a concern in pediatrics compared to adults. It is felt that children depending on their age, might be slightly more radiosensitive. Additionally, some nuclear medicine procedures evaluate physiological changes in vivo and real-time as they occur through pharmacologic interventions.
In other cases, nonradioactive drugs are used to prepare the patient and optimize radiopharmaceutical uptake for a specific study. There should also be special attention to potential interfering drugs with the uptake mechanism of the radiopharmaceutical. Examples of non-radioactive medications used for the preparation or during the exam include furosemide, acetazolamide, phenobarbital, cholecystokinin analog, angiotensin-converting enzyme inhibitors, adenosine analogs, and dobutamine.
Indications
Nuclear medicine techniques are highly sensitive. They play a major role in several instances in pediatrics. The major aspect that needs to be considered is that they are used as a standard of care or problem-solving tool, occasionally both, and how they will guide clinical management. The key indications for nuclear medicine techniques are the evaluation of:
- Lymphoma
- Sarcoma
- Neuroblastoma
- Pheochromocytoma and paraganglioma
- Miscellaneous tumors
- Thyroid cancer
- Congenital hypothyroidism
- Hyperparathyroidism
- Chronic urinary tract infections and kidney scarring
- Vesicoureteral reflux and scarring
- Obstructive uropathies
- Lymphodysplasias
- Biliary atresia
- Myocardial ischemia
- Meckel's diverticulum
- Medically refractory epilepsy
- Encephalitis
- Brain tumors
- Child abuse
- Lung perfusion pathology
- Gastrointestinal motility disorders
- Chronic microaspirations
- Gastroesophageal reflux
- Fever of unknown origin
- Evaluation of infectious foci/device infections
Contraindications
Nuclear medicine scans are very safe as the radiopharmaceutical contains a trace amount of the biological compound and therefore has no pharmacological effect. Contraindications would relate to the appropriateness of the test ordered according to the latest guidelines and appropriateness use criteria.
Other contraindications would be related to the use of sedation which is frequently needed in pediatrics. Additionally, when performed, close attention should be paid to any contraindications specific to administering a medication required for the test, including a pharmacological stressor, vasodilator, diuretic, or an angiotensin-converting enzyme inhibitor, or other.
Equipment
The latest equipment should be obtained. This is especially critical in pediatrics as newer scanners offer much higher temporal and spatial resolutions at lower injected doses, minimizing radiation exposure to the patient. Following strict quality control protocols in the radiopharmacy and the scanner, rooms are critical in delivering the highest quality and safe patient care.
Proper planned maintenance and upkeep of the nuclear medicine equipment is also essential in order to avoid equipment failures and artifacts that may affect the interpretation of studies. The latest total-body PET scanners offer the potential of imaging with a radiation exposure equivalent to a chest X-ray.[1][2][3] This is likely to be valuable and transformative in pediatric oncology patients that may require multiple successive scans to assess response to treatment and monitor disease progression.
Personnel
Fully trained, board-certified, and licensed nuclear medicine technologists under the supervision of a qualified, licensed, and board-certified nuclear medicine physician oversees the full spectrum of pediatric nuclear medicine. Specific expertise in pediatric nuclear medicine is also important. Certified child life specialists are an integral part of the care team. Qualified pediatric nurses are important for difficult intravenous access and for studies that require the administration of medications.
The anesthesiologist and anesthesiologist technologist play an important role in adult nuclear medicine practice that requires very rarely any sedatives. Proper communication between all these team members and advanced group coordination and planning for challenging cases is necessary.
Preparation
Preparation for an exam in pediatric nuclear medicine involves several aspects:
- As a rule, proper hydration is essential to optimize the study itself and decrease radiation exposure since hydration enhances rapid clearance of the radiopharmaceutical.
- Specific preparation will depend on the study performed and the radiopharmaceutical administered. For example, fasting for 4 to 6 hours is required for certain studies such as FDG PET (positron emission tomography) scans. However, this fast may be shortened to 2 or 3 hours in babies and for HIDA scans and gastric emptying studies.
- Special attention should be made to withhold any interfering medications.
- Child life involvement is frequently needed before the test to alleviate the child and family's anxiety and assist with the exam.
- A visit to nuclear medicine before the scan day and a tour of the scan room by the child may help prepare the child for the test.
- Making sure toys, snacks, ambiance, mood, relaxing music, and atmosphere are available is essential.
- Distraction devices are helpful in babies and younger children.
- Making sure that safe immobilization devices are available. This includes head holders or straps fitted to the patient's size; otherwise, they will not be effective.
- Informing the anesthesia team and other team members of the specific requirements of the nuclear medicine test allows for a smooth and safe workflow on the day of the test.
Technique or Treatment
Over the past decade, nuclear medicine has witnessed significant advances in software, hardware, and novel radiopharmaceutical approvals. This includes SPECT, PET, and hybrid imaging. Many of these advancements have improved the quality of nuclear medicine imaging in children. The field has benefitted from a higher sensitivity and lower radiation exposure in pediatrics.
In children, the acquisition and reconstruction protocols require to be closely monitored. Lower doses may require longer acquisition times. A good balance between dose and imaging time is needed. Motion has to be closely monitored. Strapping, swaddling, and use of varying levels of sedation may be required. Involving the parents and child life experts is essential. Dynamic imaging may be useless if affected by artifacts and cannot be repeated without adding another radiopharmaceutical dose to the patient.
Using the latest software with at least half-time acquisitions and iterative reconstruction techniques is necessary when available. Special expertise is needed to optimize and not hinder quality. Knowledge of all these techniques and how they apply to each patient and what factors may affect them is essential.
Complications
Radiotracers have a very high safety profile because the active component used to target the specific biological process is present in trace amounts. Complications can be related to the intravenous cannulation process. The radiopharmaceutical injection rarely may cause a rash or swell at the injection site in case of extravasation. Very rarely, headaches and nausea have been reported. Additionally, complications/adverse events related to medication injected as a part of the procedure may be encountered, such as acetazolamide, dobutamine, adenosine, captopril, furosemide, and others.
Clinical Significance
Nuclear medicine techniques play an important role in the care of pediatric patients. They can diagnose, change management, monitor progression and assess response to therapies.[4][5][6] One should note that children are not small adults, and they frequently require adjustments.
- Time requirements: Nuclear medicine exams require at least 2 to 3 times the time it takes to perform a similar test in adults. Therefore, proper planning and scheduling are required, especially in a medical practice with a mixed adult and pediatrics patient population, to avoid mistakes in scheduling and allow for the proper time to perform the test.
- Early team involvement (child life, nursing, and anesthesia) in difficult cases.
- Proper understanding that there is a spectrum of findings in normal--negative exams. This ranges from a typical/textbook normal to a normal variant versus atypical normal.
- Proper understanding that there is a spectrum of findings in abnormal--positive exams. This ranges from a typical/textbook abnormal to an abnormal variant versus atypical abnormal.
- This spectrum knowledge is critical to avoid confusion every time an atypical presentation occurs.
- Proper understanding of the indication of the nuclear medicine exam. Some exams are ordered as a standard of care in all patients with similar pathology. At the same time, others are ordered as problem-solving tools. At other times both apply.
- Appropriate use criteria: Because nuclear medicine exams involve exposure to ionizing radiation, it is essential to follow the best medical practice, guidelines, and appropriate use criteria as defined by leading medical societies and the literature.[7][8][9][10]
- Optimized scanning time: Because children cannot lay still for the duration of scans, anesthesia may be used at times. Choosing the most appropriate imaging protocol that will provide diagnostic value in the least amount of time is needed. Purchasing the latest technology scanners will allow diagnostic quality imaging with a rapid scanning time with the equivalent of a chest X-ray or lower radiation exposure dose.[1][2][3][11]
- Optimized radiopharmaceutical activity: Purchasing the latest technology scanners will allow diagnostic quality imaging at very low radiopharmaceutical doses, the equivalent of a chest x-ray, or lower radiation exposure dose.[1][2][3][11] The image gently campaign was developed in late 2007 and since then has been advocating for lower radiation doses in nuclear medicine and diagnostic radiology. This campaign was accompanied by a harmonization in the injected radiopharmaceutical activities in pediatrics aiming for the ALARA principle.[12][13] As low as reasonably achievable to get a diagnostic scan. The clinical shift occurred from pretty images to diagnostic images with no artifacts.[14]
- Benefits/risk estimate: Physicians should carefully weigh the benefit-risk ratio before ordering an exam, as with any procedure or test. The benefit of using diagnostic and therapeutic nuclear medicine techniques in pediatrics is huge when best medical practice and guidelines are followed.
- Indications:
- Lymphoma: 3rd most common malignancy in children. There are mostly two types: Hodgkin's lymphoma and non-Hodgkin's lymphoma. Better outcomes are noted in children compared to adults. However, long-term complications from treatment are center stage. Therefore, de-escalation treatment regimens are being explored that would improve outcomes and decrease immediate and late adverse effects. The role of FDG-PET is established in pediatric lymphomas and has become the standard of care in pediatric Hodgkin lymphoma initial staging, restaging, and response to therapy assessments.[15][16] Early PET response in HL is an important prognostic indicator. Newer protocols use dynamic response assessments with FDG PET to modulate therapy or deescalate treatments. This latter is a crucial element to decrease long-term adverse effects from anti-cancer treatment.[17][18][19][20][21][22][23]
- Sarcomas: Bone sarcomas account for approximately 6 percent of all childhood cancers, and osteosarcomas account for approximately 3 percent of childhood cancers overall. Bone scans can be used to evaluate multifocal disease. However, this is being replaced nowadays with FDG PET-CT scans for staging and restaging assessments. Although whole-body MRI (magnetic resonance imaging) is the mainstay of imaging, it may have some limitations at follow-up with prostheses artifacts and assessing response to treatment. A CT scan with thin slices is required to monitor for any lung metastasis. FDG PET-CT is very good at initial staging, restaging, therapy response assessments, and reports showing sensitivity and specificity in the '90s. One should pay close attention to the PET-CT protocol used and adjust the attenuation correction CT protocol to be able to detect small lung nodule metastasis. This is crucial considering the lung is the site of 80% of metastasis.[24][25][26] Quantitative parameters such as metabolic tumor volume and total lesion glycolysis may be best used to assess response to treatment.[27] FDG PET at 6 weeks can predict neoadjuvant chemotherapy effect on time to progression and pathologic response. FDG PET was also described to be of prognostic value.[28][24][29][30][31][24] The Children's oncology group recommends FDG PET and or SPECT Bone scanning at initial diagnosis and before any surgery or local control intervention. FDG PET or SPECT bone scanning is also recommended at follow-up surveillance on chemotherapy or post-chemotherapy patients if symptoms arise or if metastatic disease is present on a prior scan.
- Neuroblastoma: Represents 10% of solid tumors in children. It is the most common extracranial solid tumor.[32] 123-I Metaiodobenzylguanadine (MIBG) is used in conjunction with MRI or CT to stage these patients. MIBG is structurally similar to norepinephrine and concentrates in secretory granules of catecholamine-producing neural crest cells. It has high sensitivity and specificity of up to 90%.[33] Using the latest hybrid imaging SPECT-CT techniques is recommended.[34] Bone scans are rarely used nowadays but may be helpful if MIBG or PET radiopharmaceuticals are not readily available. Novel PET radiopharmaceuticals such as Iodine 124 MIBG, 18F FDOPA, and 68Ga DOTATATE show higher sensitivities and specificities.[35][36][37][38][39] The higher spatial resolution of PET imaging also allows for improved dosimetry when radionuclide therapies are contemplated.[40][41] FDG PET is also used in MIBG negative cases and may offer some prognostic value.[42][43][44] Considering the heterogeneity of the disease, combining two radiopharmaceuticals may potentially play an important role.[45] A novel fluorinated MFBG PET imaging probe is shown to be almost twice more sensitive than Iodine123 MIBG on a lesional analysis basis.[46]
- Pheochromocytoma/paraganglioma: These are rare pediatric tumors. Pheochromocytomas usually arise from the adrenals and paragangliomas from extra-adrenal locations. Pheocromoyctomas frequently will secrete catecholamines, and paragangliomas are quite variable. About two-thirds are sporadic, but several germline mutations have been described, such as RET, SDHD, SDHB, SDHC, SDHAF2, or SDHA, VHL, TMEM127, or MAX genes.[47][48][49] MIBG scans have traditionally been used to evaluate pheochromocytoma and paragangliomas. The overall limited accuracy has been partially overcome by the use of novel hybrid SPECT-CT techniques. However, newer techniques using PET radiopharmaceuticals are more sensitive and should preferably be used when available. FDG PET scans seem to be superior in patients with SDH mutations, and FDOPA scans are superior in non-SDH mutations.[50] FDA or FDG PET would be preferable for staging paragangliomas with RET mutations.[51] Alternatively, Gallium DOTATATE can be used with high accuracy to stage SDH-related paragangliomas located in the head and neck region. Some reports have also suggested the overall superior sensitivity on a lesional basis in paragangliomas in general.[50][52][48] In Pheochromocytomas, FDOPA and FDG are superior. Considering the heterogeneity of disease and lesions and considering the Theranostic paradigm using different radiotracers in the same patient may hold additional value.[53][54][52][55] MFBG, a newer PET analog to MIBG, demonstrates superior sensitivity and accuracy to the traditional SPECT MIBG scans with about twice the amount of lesions detected.[46][56][57] Further larger studies with pooled data from multiple centers are necessary to further elucidate the preferred radiopharmaceutical in a complex mutational landscape.
- Miscellaneous tumors: FDG PET scans are proven to be highly accurate in staging and restaging gastrointestinal stromal tumors and mixed germ cell tumors.[58][59][60][61][62][63] On the other hand, neuroendocrine tumors and insulinomas are easily characterized and staged with Gallium DOTATATE.[64][65][66][67] Note should be made that Gallium DOTATATE could be most of the time interchangeable with other similar Gallium DOTANOC, DOTATOC, or copper-based somatostatin receptor-based ligands.
- Thyroid cancer: Thyroid cancer is uncommon in children compared to adults. Papillary thyroid cancer is the most common type. Although locoregional lymph node and distant metastasis are more frequent than in adults, the prognosis is significantly better, and survival rates are extremely high even with distant metastasis with appropriate treatment.[68] Iodine scans with or without SPECT-CT and ultrasound are the standard imaging techniques.[69][70][71][72] The non-iodine avid disease can be imaged successfully with FDG PET.[73][74][75] Medullary thyroid cancer is rare but is best served by using FDOPA PET for staging and restaging when calcitonin levels are higher than 100 pg/ml.[74][76]
- Congenital hypothyroidism: Pertechnetetate scan is a fairly simple exam to perform. It can pretty accurately distinguish between several etiologies: athyrogenesis (no thyroid uptake), ectopic thyroid/lingual thyroid (uptake is noted outside the expected thyroid bed/lower neck), and thyroid hormone dysgenesis (normal thyroidal uptake).
- Hyperparathyroidism: Hyperparathyroidism is rarely encountered in pediatrics and can be evaluated by a sestamibi scan. It can localize parathyroid adenomas. Precise localization in a eutopic or ectopic location can be obtained using hybrid imaging techniques.
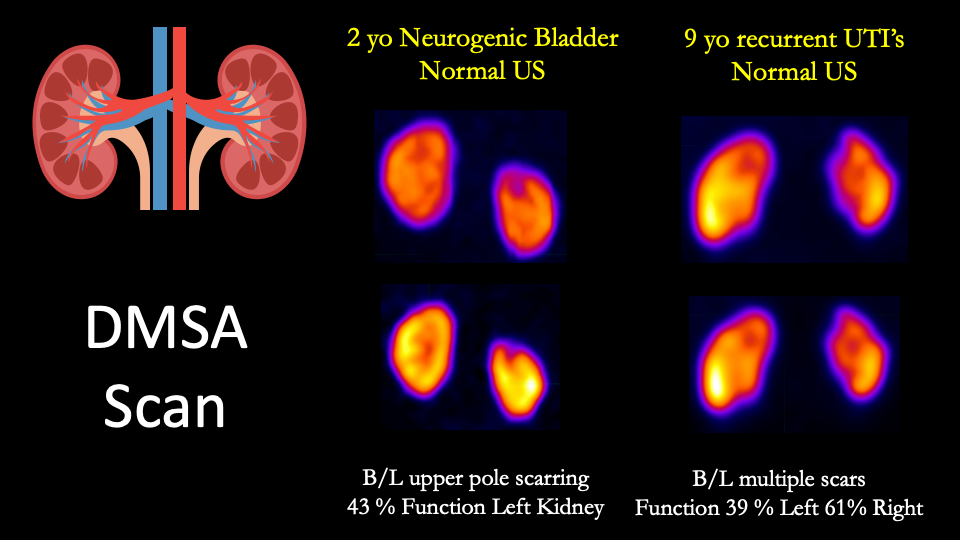
- Chronic urinary tract infections and kidney scarring: DMSA scan with planar and SPECT imaging is the most sensitive technique currently available for clinical use to evaluate kidney scarring.[77][78][79][80][81] An initial report with PSMA PET has been published, although this is expensive and not widely available. PSMA PET is also not FDA-approved yet.
- Vesicoureteral reflux and scarring: A DMSA scan is also quite effective in detecting renal scarring in patients with vesicoureteral reflux.[82][83]
- Obstructive uropathies: Ultrasound is the imaging of choice for patients' initial evaluation and follow-up with suspicion of obstructive uropathy. However, diuretic renograms are frequently used to confirm an obstruction and risk-stratify dilated collecting systems.[84][85]
- Lymphodysplasias: Lymphoscintigrams with or without newer hybrid imaging SPECT-CT techniques are simple and accurate studies to evaluate abnormalities of the lymphatic system. It involves the intradermic, more or less subcutaneous injection of a colloid radiopharmaceutical. Indications include congenital lymphodysplasias, lymphedema, lymphatic leaks, lymphangiomas, lymphangiomatosis, Gorham Stout disease, and lymphangiectasia.[86][87][88][89][90][91] It is also helpful in the evaluation of chyluria, chyloperitoneum, and chylothoraces. Protein-losing enteropathies are more effectively evaluated using an HSA scan.[92][93][94][95]
- Biliary atresia (BA): Biliary atresia is deadly without early surgical intervention (Kasai procedure). Optimal outcomes occur when surgery is performed before 45 days of life. Delay in diagnosis can be accompanied by complications such as cirrhosis, portal hypertension, liver failure, a decrease in the success rate of the Kasai procedure, and even death. HIDA scans/hepatobiliary scans evaluate uptake in the liver as well as the hepatobiliary system. Radiopharmaceutical excretion into the bowel excludes BA. Proper preparation with phenobarbital 5-7 days before the scan is essential.[96][97][98][99][100] Jancelewicz et al. reported in a cohort of 212 babies (45 with BA) that a normal percutaneous cholangiogram, bowel excretion on a HIDA scan, and blood work variables consisting of a GGT <150U/L and conjugated bilirubin <2.5mg/dL excluded BA with a 100% sensitivity.[100]
- Myocardial perfusion: Cardiac MRI, echocardiography, and cardiac CT are the mainstays of pediatric imaging. Anatomical information is essential in cardiac congenital anomalies. MRI is nowadays able to provide reproducible stress-induced functional parameters. However, nuclear medicine myocardial perfusion imaging can still be used as a problem-solving tool. It is seldom needed but can be helpful to evaluate for ischemia and risk stratify patients alone or in combination with MR. Common indications are congenital heart disease repair, Kawasaki disease, hypoplastic heart, anomalous origin of the coronaries, coronary bridging, cardiac transplants, and other cardiomyopathies. SPECT or PET can be used with pharmacological stress. Although PET offers the advantage of absolute myocardial blood flow quantification, this should be used with caution, and proper expertise in children should be sought as normal values are quite different and higher compared to adults.[101][102][103][104][105][106][107][108]
- Meckel diverticulum: Meckel scan is a simple and highly accurate test to evaluate Meckel diverticulum with a reported sensitivity and specificity in the mid-'90s.[109] In the few negative cases with high clinical suspicion, a repeat exam may have an additional value in detecting the Meckel's diverticulum.[110] The addition of novel hybrid imaging techniques with SPECT-CT can be, in some cases, of additional value.[111]
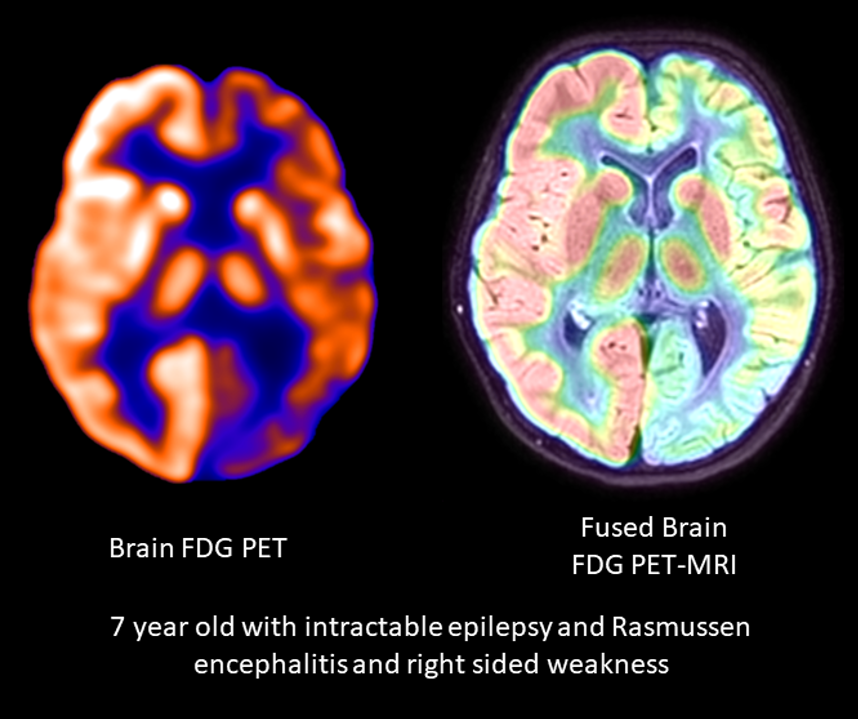
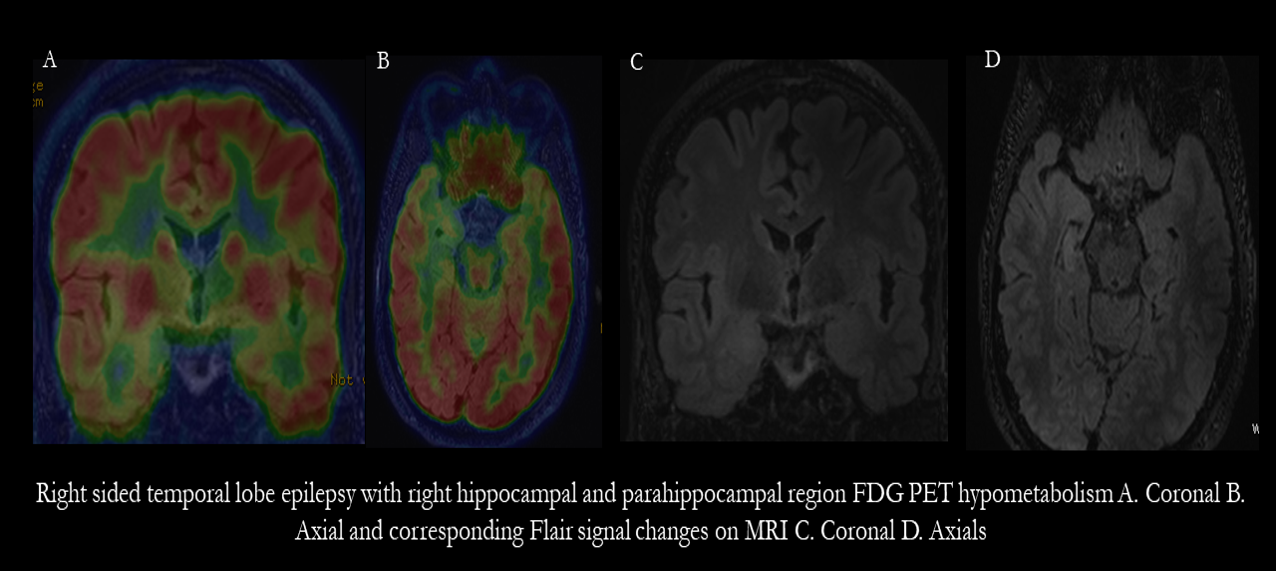
- Medically refractory epilepsy: Nuclear medicine techniques are valuable in the presurgical workup of medically refractory epilepsy patients. Cerebral blood flow (CBF) SPECT and FDG PET imaging are essential exams to delineate the seizure onset zone (SOZ) required to be resected. Successful SOZ localization is needed for postsurgical seizure freedom. In patients with a clinical semiology amenable to CBF imaging, ictal-interictal subtraction offers accuracy in the '90s. Inter-ictal FDG PET imaging is also very useful in MRI negative cases to detect the SOZ. In MRI-positive cases, FDG PET delineation of the SOZ has also been reported to correlate with outcomes.
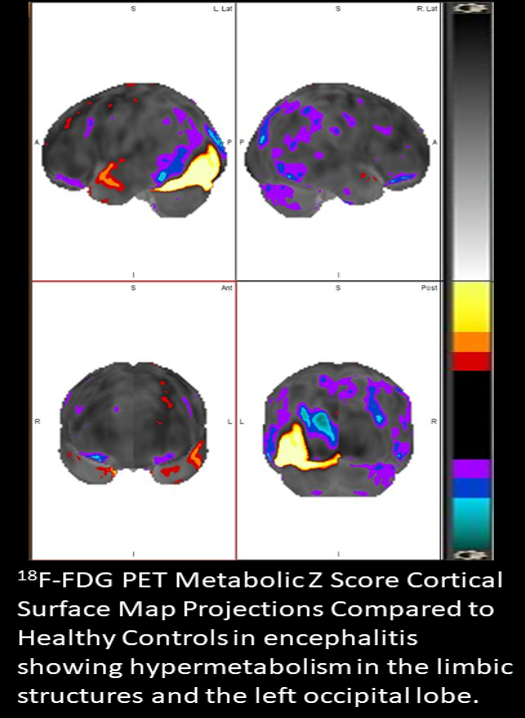
- Encephalitis: FDG PET is the most sensitive imaging technique to evaluate brain changes in encephalitis. It can also be used to monitor treatment response and metabolic brain changes in cases that later on develop epilepsy.[112][113][114]
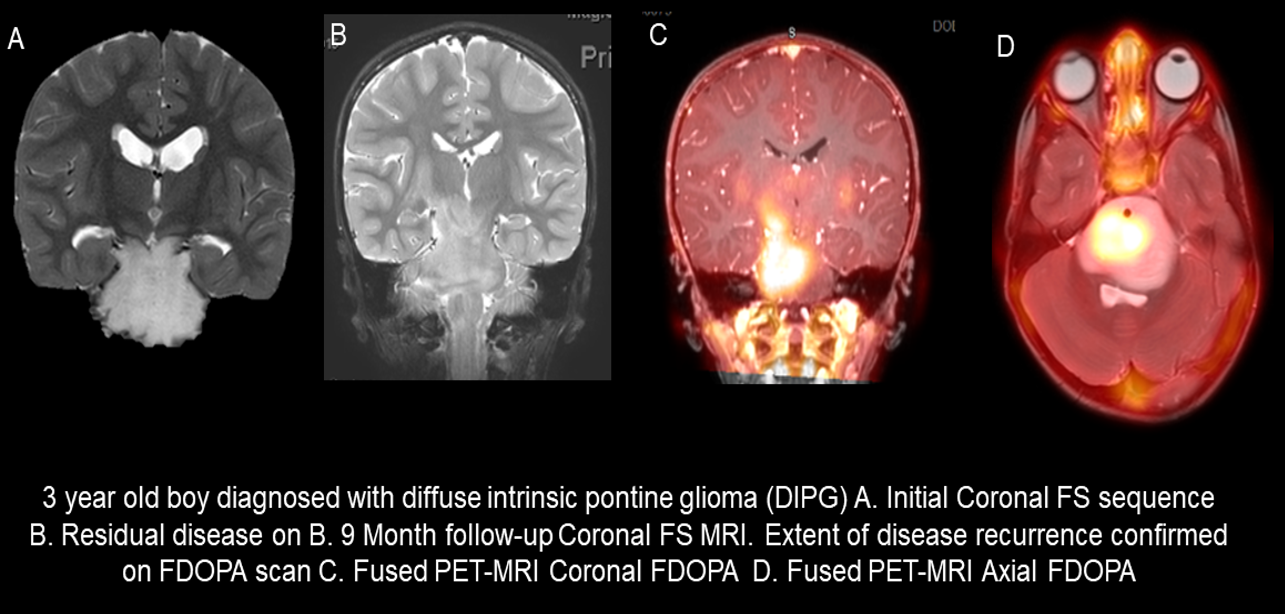
- Brain tumors: MRI is the gold standard and workhorse of imaging in pediatric brain tumors. However, in some cases, MRI fails to fully characterize a lesion. Aminoacid imaging with C11-methionine, FDOPA, or FET PET can be used as a problem-solving tool in differentiating radiation necrosis changes versus recurrence in radiation treatment planning, defining the surgical extent, and guiding biopsies.[115][116][117][118][119][120]
- Child abuse: Non-accidental injury in babies and children is a challenging clinical conundrum. Diagnosis is crucial, and a high suspicion should always be maintained. Bone scan offers a high sensitivity exam that adds value as an adjunct to the traditional skeletal survey.[121][122][123][124][125][126] Bone scans can also be used in additional pathologies such as sports injuries, scoliosis, trauma, back pain after surgery, osteoid osteoma, and Langerhans histiocytosis. Fluoride PET bone scans offer a high resolution and may replace the traditional bone SPECT scan when available.[127]
- Lung perfusion pathology: Pulmonary artery anomalies and congenital cardiac malformations can be evaluated with MAA scans. Lung perfusion can be evaluated before and after an intervention.[128][129][130][131] Ventilation-perfusion scans can be used to assess unilateral hyperlucent lung.[132][128]
- Gastrointestinal motility disorders: Delayed gastric emptying is frequently encountered in children. Solid or liquid-based gastric emptying studies can be used to assess gastric emptying.[133][134][135][136] The solid-based protocol is the most sensitive and preferred when the child can tolerate eating solid foods. Otherwise, the liquid-based protocol is more frequently used as pediatric patients frequently have feeding tubes. The gastric emptying liquid is also used in babies and very young children.
- Chronic microaspirations: Patients with chronic microaspirations have frequent repeated pulmonary infections. Salivagrams are relatively easy nuclear medicine tests that require little preparation and can detect microaspirations.[137][138] One drop of Technetium sulfur colloid or DTPA is administered on the tongue of the child/baby. Visualization of radiotracer accumulation in the lungs is consistent with aspiration. Using a technique administering 3 drops serially has a higher yield and sensitivity in detecting aspirations. Kim et al. showed that salivagrams and videofluoroscopic exams are complementary in detecting aspirations.[139] On the other hand, it showed that in 290 children, indwelling nasogastric tubes did not affect the positivity rate of salivagrams compared to pediatric patients without nasogastric tubes.[140]
- Gastroesophageal reflux: In contrast to salivagrams, gastroesophageal reflux studies or milk scans are also used to detect pulmonary aspiration. Jigang et al. compared both techniques in a cohort of 4186 patients and concluded that salivagrams have a much higher detection rate of 20.3% vs. 0.4% for gastroesophageal reflux studies.
- Fever of unknown origin: A variety of etiologies can be explored using FDG PET scans ranging from systemic inflammatory conditions, rheumatologic diseases/vasculidities, infectious processes, and oncology pathology.[141][142][143][144][145][146][147] Additionally, FDG PET scans are useful in evaluating conditions with increased inflammatory markers, even in the absence of fever. FDG PET scans can be used to evaluate response to therapies as well.
- Evaluation of device infections: FDG PET scans are used to evaluate cardiovascular devices and implanted musculoskeletal hardware.[148][149][147][150][151][152] They have demonstrated very high sensitivity and specificity.[153] It has been shown to be superior to echocardiography and cardiac CT. It has also been shown to be prognostic and correlates well with outcomes.[154][155] In contrast, white blood cell scans can also be used in the absence of FDG PET availability and, when used with hybrid imaging, SPECT-CT techniques offer high sensitivity, high specificity, and high reader confidence.[156][157]
Enhancing Healthcare Team Outcomes
Pediatric nuclear medicine is a niche field and requires expertise for optimal outcomes. Appropriate use of nuclear medicine exams and their impact on clinical management obviates concerns about radiation exposure. Highly skilled experts such as child life specialists, pediatric anesthesia technologists, pediatric anesthesiologists, pediatric nuclear medicine technologists, pediatric nurses, and pediatric nuclear medicine physicians are needed.
Proper communication and planning are essential. Following best medical practice and society guidelines is paramount. Standardized, harmonized protocols must be followed. An integrated simple and advanced collaborative pathway and constant case discussions between the nuclear medicine team and referring pediatricians and pediatric subspecialists (in oncology, surgery, neurology, neurosurgery, urology, nephrology, rheumatology, gastroenterology, and orthopedics) will deliver optimized outcomes. [Level 3, 4, and 5]
Media
References
Cherry SR, Jones T, Karp JS, Qi J, Moses WW, Badawi RD. Total-Body PET: Maximizing Sensitivity to Create New Opportunities for Clinical Research and Patient Care. Journal of nuclear medicine : official publication, Society of Nuclear Medicine. 2018 Jan:59(1):3-12. doi: 10.2967/jnumed.116.184028. Epub 2017 Sep 21 [PubMed PMID: 28935835]
Level 2 (mid-level) evidenceVandenberghe S, Moskal P, Karp JS. State of the art in total body PET. EJNMMI physics. 2020 May 25:7(1):35. doi: 10.1186/s40658-020-00290-2. Epub 2020 May 25 [PubMed PMID: 32451783]
Badawi RD, Shi H, Hu P, Chen S, Xu T, Price PM, Ding Y, Spencer BA, Nardo L, Liu W, Bao J, Jones T, Li H, Cherry SR. First Human Imaging Studies with the EXPLORER Total-Body PET Scanner. Journal of nuclear medicine : official publication, Society of Nuclear Medicine. 2019 Mar:60(3):299-303. doi: 10.2967/jnumed.119.226498. Epub 2019 Feb 7 [PubMed PMID: 30733314]
Bellini C, Bonioli E, Boccardo F. Lymphoscintigraphy in paediatric patients. Phlebology. 2009 Oct:24(5):237; author reply 238. doi: 10.1258/phleb.2009.009012. Epub [PubMed PMID: 19767489]
Level 3 (low-level) evidenceSzuba A, Shin WS, Strauss HW, Rockson S. The third circulation: radionuclide lymphoscintigraphy in the evaluation of lymphedema. Journal of nuclear medicine : official publication, Society of Nuclear Medicine. 2003 Jan:44(1):43-57 [PubMed PMID: 12515876]
Bellini C, Boccardo F, Campisi C, Villa G, Taddei G, Traggiai C, Bonioli E. Lymphatic dysplasias in newborns and children: the role of lymphoscintigraphy. The Journal of pediatrics. 2008 Apr:152(4):587-9, 589.e1-3. doi: 10.1016/j.jpeds.2007.12.018. Epub [PubMed PMID: 18346521]
Expert Panel on Pediatric Imaging, Brown BP, Simoneaux SF, Dillman JR, Rigsby CK, Iyer RS, Alazraki AL, Bardo DME, Chan SS, Chandra T, Dorfman SR, Garber MD, Moore MM, Nguyen JC, Peters CA, Shet NS, Siegel A, Waseem M, Karmazyn B. ACR Appropriateness Criteria® Antenatal Hydronephrosis-Infant. Journal of the American College of Radiology : JACR. 2020 Nov:17(11S):S367-S379. doi: 10.1016/j.jacr.2020.09.017. Epub [PubMed PMID: 33153550]
Lee SB, Cho YJ, Lee S, Choi YH, Cheon JE, Kim WS. Korean Society of Thyroid Radiology Guidelines for the Management of Pediatric Thyroid Nodules: Suitability and Risk Factors. Thyroid : official journal of the American Thyroid Association. 2021 Oct:31(10):1472-1480. doi: 10.1089/thy.2020.0875. Epub 2021 May 19 [PubMed PMID: 33832344]
Vali R, Alessio A, Balza R, Borgwardt L, Bar-Sever Z, Czachowski M, Jehanno N, Kurch L, Pandit-Taskar N, Parisi M, Piccardo A, Seghers V, Shulkin BL, Zucchetta P, Lim R. SNMMI Procedure Standard/EANM Practice Guideline on Pediatric (18)F-FDG PET/CT for Oncology 1.0. Journal of nuclear medicine : official publication, Society of Nuclear Medicine. 2021 Jan:62(1):99-110. doi: 10.2967/jnumed.120.254110. Epub [PubMed PMID: 33334912]
Level 1 (high-level) evidenceMajd M, Bar-Sever Z, Santos AI, De Palma D. The SNMMI and EANM Procedural Guidelines for Diuresis Renography in Infants and Children. Journal of nuclear medicine : official publication, Society of Nuclear Medicine. 2018 Oct:59(10):1636-1640. doi: 10.2967/jnumed.118.215921. Epub [PubMed PMID: 30275286]
Magill D, Alavi A. Radiation Safety Concerns Related to PET/Computed Tomography Imaging for Assessing Pediatric Diseases and Disorders. PET clinics. 2020 Jul:15(3):293-298. doi: 10.1016/j.cpet.2020.03.012. Epub [PubMed PMID: 32498985]
Lassmann M, Treves ST, EANM/SNMMI Paediatric Dosage Harmonization Working Group. Paediatric radiopharmaceutical administration: harmonization of the 2007 EANM paediatric dosage card (version 1.5.2008) and the 2010 North American consensus guidelines. European journal of nuclear medicine and molecular imaging. 2014 May:41(5):1036-41. doi: 10.1007/s00259-014-2731-9. Epub 2014 Mar 6 [PubMed PMID: 24599377]
Level 3 (low-level) evidenceFahey FH, Ziniel SI, Manion D, Baker A, Treves ST. Administered Activities in Pediatric Nuclear Medicine and the Impact of the 2010 North American Consensus Guidelines on General Hospitals in the United States. Journal of nuclear medicine : official publication, Society of Nuclear Medicine. 2016 Sep:57(9):1478-85. doi: 10.2967/jnumed.116.172148. Epub 2016 Apr 7 [PubMed PMID: 27056617]
Level 3 (low-level) evidenceTreves ST, Lassmann M, EANM/SNMMI Pediatric Dosage Harmonization Working Group. International guidelines for pediatric radiopharmaceutical administered activities. Journal of nuclear medicine : official publication, Society of Nuclear Medicine. 2014 Jun:55(6):869-70. doi: 10.2967/jnumed.114.139980. Epub 2014 Apr 17 [PubMed PMID: 24744446]
Ferrari C, Niccoli Asabella A, Merenda N, Altini C, Fanelli M, Muggeo P, De Leonardis F, Perillo T, Santoro N, Rubini G. Pediatric Hodgkin Lymphoma: Predictive value of interim 18F-FDG PET/CT in therapy response assessment. Medicine. 2017 Feb:96(5):e5973. doi: 10.1097/MD.0000000000005973. Epub [PubMed PMID: 28151888]
Bakhshi S, Radhakrishnan V, Sharma P, Kumar R, Thulkar S, Vishnubhatla S, Dhawan D, Malhotra A. Pediatric nonlymphoblastic non-Hodgkin lymphoma: baseline, interim, and posttreatment PET/CT versus contrast-enhanced CT for evaluation--a prospective study. Radiology. 2012 Mar:262(3):956-68. doi: 10.1148/radiol.11110936. Epub [PubMed PMID: 22357895]
Kluge R, Wittig T, Georgi TW, Kurch L, Sabri O, Wallace WH, Klekawka T, Fernández-Teijeiro A, Ceppi F, Karlén J, Pears J, Cepelová M, Fosså A, Beishuizen A, Hjalgrim LL, Körholz D, Mauz-Körholz C, Hasenclever D. Comparison of Interim PET Response to Second-Line Versus First-Line Treatment in Classic Hodgkin Lymphoma: Contribution to the Development of Response Criteria for Relapsed or Progressive Disease. Journal of nuclear medicine : official publication, Society of Nuclear Medicine. 2021 Mar:62(3):338-341. doi: 10.2967/jnumed.120.247924. Epub 2020 Aug 6 [PubMed PMID: 32764122]
Verhagen MV, Menezes LJ, Neriman D, Watson TA, Punwani S, Taylor SA, Shankar A, Daw S, Humphries PD. (18)F-FDG PET/MRI for Staging and Interim Response Assessment in Pediatric and Adolescent Hodgkin Lymphoma: A Prospective Study with (18)F-FDG PET/CT as the Reference Standard. Journal of nuclear medicine : official publication, Society of Nuclear Medicine. 2021 Nov:62(11):1524-1530. doi: 10.2967/jnumed.120.260059. Epub 2021 Feb 19 [PubMed PMID: 33608429]
Ingley KM, Nadel HR, Potts JE, Wilson DC, Eftekhari A, Deyell RJ. The Utility of PET/CT in Guiding Radiotherapy Reduction for Children With Hodgkin Lymphoma Treated With ABVD. Journal of pediatric hematology/oncology. 2020 Mar:42(2):e87-e93. doi: 10.1097/MPH.0000000000001534. Epub [PubMed PMID: 31259825]
Rahman HA, El Semary SF, Ahmed G, Kenaai NE, Omar W, Zaky I, Nagy N. Can FDG-PET replace biopsy for the evaluation of residual tumor in pediatric mature B-cell non-Hodgkin lymphoma? Pediatric blood & cancer. 2020 Sep:67(9):e28310. doi: 10.1002/pbc.28310. Epub 2020 Jul 7 [PubMed PMID: 32634295]
Chen S, He K, Feng F, Wang S, Yin Y, Fu H, Wang H. Metabolic tumor burden on baseline (18)F-FDG PET/CT improves risk stratification in pediatric patients with mature B-cell lymphoma. European journal of nuclear medicine and molecular imaging. 2019 Aug:46(9):1830-1839. doi: 10.1007/s00259-019-04363-y. Epub 2019 Jun 11 [PubMed PMID: 31187163]
Chen S, Wang S, He K, Ma C, Fu H, Wang H. PET/CT predicts bone marrow involvement in paediatric non-Hodgkin lymphoma and may preclude the need for bone marrow biopsy in selected patients. European radiology. 2018 Jul:28(7):2942-2950. doi: 10.1007/s00330-018-5306-5. Epub 2018 Jan 30 [PubMed PMID: 29383519]
Bhojwani D, McCarville MB, Choi JK, Sawyer J, Metzger ML, Inaba H, Davidoff AM, Gold R, Shulkin BL, Sandlund JT. The role of FDG-PET/CT in the evaluation of residual disease in paediatric non-Hodgkin lymphoma. British journal of haematology. 2015 Mar:168(6):845-53. doi: 10.1111/bjh.13219. Epub 2014 Nov 10 [PubMed PMID: 25382494]
Level 2 (mid-level) evidencePolverari G, Ceci F, Passera R, Crane J, Du L, Li G, Fanti S, Bernthal N, Eilber FC, Allen-Auerbach M, Czernin J, Calais J, Federman N. [(18)F]FDG PET/CT for evaluating early response to neoadjuvant chemotherapy in pediatric patients with sarcoma: a prospective single-center trial. EJNMMI research. 2020 Oct 15:10(1):122. doi: 10.1186/s13550-020-00715-0. Epub 2020 Oct 15 [PubMed PMID: 33063147]
Donner D, Feraco P, Meneghello L, Rombi B, Picori L, Chierichetti F. Usefulness of 18f-FDG PET-CT in Staging, Restaging, and Response Assessment in Pediatric Rhabdomyosarcoma. Diagnostics (Basel, Switzerland). 2020 Dec 21:10(12):. doi: 10.3390/diagnostics10121112. Epub 2020 Dec 21 [PubMed PMID: 33371506]
Harrison DJ, Chi YY, Tian J, Hingorani P, Mascarenhas L, McCowage GB, Weigel BJ, Venkatramani R, Wolden SL, Yock TI, Rodeberg DA, Hayes-Jordan AA, Teot LA, Spunt SL, Meyer WH, Hawkins DS, Shulkin BL, Parisi MT. Metabolic response as assessed by (18) F-fluorodeoxyglucose positron emission tomography-computed tomography does not predict outcome in patients with intermediate- or high-risk rhabdomyosarcoma: A report from the Children's Oncology Group Soft Tissue Sarcoma Committee. Cancer medicine. 2021 Feb:10(3):857-866. doi: 10.1002/cam4.3667. Epub 2020 Dec 19 [PubMed PMID: 33340280]
El-Hennawy G, Moustafa H, Omar W, Elkinaai N, Kamel A, Zaki I, Farid N, El-Kholy E. Different (18) F-FDG PET parameters for the prediction of histological response to neoadjuvant chemotherapy in pediatric Ewing sarcoma family of tumors. Pediatric blood & cancer. 2020 Nov:67(11):e28605. doi: 10.1002/pbc.28605. Epub 2020 Jul 24 [PubMed PMID: 32706520]
Elmanzalawy A, Vali R, Chavhan GB, Gupta AA, Omarkhail Y, Amirabadi A, Shammas A. The impact of (18)F-FDG PET on initial staging and therapy planning of pediatric soft-tissue sarcoma patients. Pediatric radiology. 2020 Feb:50(2):252-260. doi: 10.1007/s00247-019-04530-1. Epub 2019 Oct 18 [PubMed PMID: 31628508]
Schmidkonz C, Krumbholz M, Atzinger A, Cordes M, Goetz TI, Prante O, Ritt P, Schaefer C, Agaimy A, Hartmann W, Rössig C, Fröhlich B, Bäuerle T, Dirksen U, Kuwert T, Metzler M. Assessment of treatment responses in children and adolescents with Ewing sarcoma with metabolic tumor parameters derived from (18)F-FDG-PET/CT and circulating tumor DNA. European journal of nuclear medicine and molecular imaging. 2020 Jun:47(6):1564-1575. doi: 10.1007/s00259-019-04649-1. Epub 2019 Dec 18 [PubMed PMID: 31853559]
El-Kholy E, El Nadi E, Hafez H, Ahmed S, Younes A, El-Kenanii N, Khalid E. Added predictive value of 18F-FDG PET/CT for pediatric rhabdomyosarcoma. Nuclear medicine communications. 2019 Sep:40(9):898-904. doi: 10.1097/MNM.0000000000001040. Epub [PubMed PMID: 31145205]
Albano D, Dondi F, Schumacher RF, D'Ippolito C, Porta F, Giubbini R, Bertagna F. Clinical and Prognostic Role of 18F-FDG PET/CT in Pediatric Ewing Sarcoma. Journal of pediatric hematology/oncology. 2020 Mar:42(2):e79-e86. doi: 10.1097/MPH.0000000000001518. Epub [PubMed PMID: 31135716]
Jiang M, Stanke J, Lahti JM. The connections between neural crest development and neuroblastoma. Current topics in developmental biology. 2011:94():77-127. doi: 10.1016/B978-0-12-380916-2.00004-8. Epub [PubMed PMID: 21295685]
Level 3 (low-level) evidenceVik TA, Pfluger T, Kadota R, Castel V, Tulchinsky M, Farto JC, Heiba S, Serafini A, Tumeh S, Khutoryansky N, Jacobson AF. (123)I-mIBG scintigraphy in patients with known or suspected neuroblastoma: Results from a prospective multicenter trial. Pediatric blood & cancer. 2009 Jul:52(7):784-90. doi: 10.1002/pbc.21932. Epub [PubMed PMID: 19185008]
Level 1 (high-level) evidenceKitamura Y, Baba S, Isoda T, Maruoka Y, Sasaki M, Kamitani T, Koga Y, Kawakubo N, Matsuura T, Ishigami K. (123)I metaiodobenzylguanidine (MIBG) uptake predicts early relapse of neuroblastoma using semi-quantitative SPECT/CT analysis. Annals of nuclear medicine. 2021 May:35(5):549-556. doi: 10.1007/s12149-021-01595-7. Epub 2021 Feb 14 [PubMed PMID: 33586098]
Piccardo A, Morana G, Puntoni M, Campora S, Sorrentino S, Zucchetta P, Ugolini M, Conte M, Cistaro A, Ferrarazzo G, Pescetto M, Lattuada M, Bottoni G, Garaventa A, Giovanella L, Lopci E. Diagnosis, Treatment Response, and Prognosis: The Role of (18)F-DOPA PET/CT in Children Affected by Neuroblastoma in Comparison with (123)I-mIBG Scan: The First Prospective Study. Journal of nuclear medicine : official publication, Society of Nuclear Medicine. 2020 Mar:61(3):367-374. doi: 10.2967/jnumed.119.232553. Epub 2019 Sep 20 [PubMed PMID: 31541036]
Aboian MS, Huang SY, Hernandez-Pampaloni M, Hawkins RA, VanBrocklin HF, Huh Y, Vo KT, Gustafson WC, Matthay KK, Seo Y. (124)I-MIBG PET/CT to Monitor Metastatic Disease in Children with Relapsed Neuroblastoma. Journal of nuclear medicine : official publication, Society of Nuclear Medicine. 2021 Jan:62(1):43-47. doi: 10.2967/jnumed.120.243139. Epub 2020 May 15 [PubMed PMID: 32414950]
Cistaro A, Quartuccio N, Caobelli F, Piccardo A, Paratore R, Coppolino P, Sperandeo A, Arnone G, Ficola U. 124I-MIBG: a new promising positron-emitting radiopharmaceutical for the evaluation of neuroblastoma. Nuclear medicine review. Central & Eastern Europe. 2015:18(2):102-6. doi: 10.5603/NMR.2015.0024. Epub [PubMed PMID: 26315872]
Maaz AUR, O'Doherty J, Djekidel M. (68)Ga-DOTATATE PET/CT for Neuroblastoma Staging: Utility for Clinical Use. Journal of nuclear medicine technology. 2021 Sep:49(3):265-268. doi: 10.2967/jnmt.120.258939. Epub 2021 Apr 5 [PubMed PMID: 33820858]
Telli T, Lay Ergün E, Volkan Salanci B, Özgen Kiratli P. The Complementary Role of 68Ga-DOTATATE PET/CT in Neuroblastoma. Clinical nuclear medicine. 2020 Apr:45(4):326-329. doi: 10.1097/RLU.0000000000002961. Epub [PubMed PMID: 31977455]
Marsh IR, Grudzinski J, Baiu DC, Besemer A, Hernandez R, Jeffery JJ, Weichert JP, Otto M, Bednarz BP. Preclinical Pharmacokinetics and Dosimetry Studies of (124)I/(131)I-CLR1404 for Treatment of Pediatric Solid Tumors in Murine Xenograft Models. Journal of nuclear medicine : official publication, Society of Nuclear Medicine. 2019 Oct:60(10):1414-1420. doi: 10.2967/jnumed.118.225409. Epub 2019 Mar 29 [PubMed PMID: 30926646]
Lee CL, Wahnishe H, Sayre GA, Cho HM, Kim HJ, Hernandez-Pampaloni M, Hawkins RA, Dannoon SF, VanBrocklin HF, Itsara M, Weiss WA, Yang X, Haas-Kogan DA, Matthay KK, Seo Y. Radiation dose estimation using preclinical imaging with 124I-metaiodobenzylguanidine (MIBG) PET. Medical physics. 2010 Sep:37(9):4861-7 [PubMed PMID: 20964203]
Level 3 (low-level) evidenceMan S, Yan J, Li J, Cao Y, Hu J, Ma W, Liu J, Zhao Q. Value of pretreatment 18F-FDG PET/CT in prognosis and the reflection of tumor burden: a study in pediatric patients with newly diagnosed neuroblastoma. International journal of medical sciences. 2021:18(8):1857-1865. doi: 10.7150/ijms.58263. Epub 2021 Feb 24 [PubMed PMID: 33746603]
Sung AJ, Weiss BD, Sharp SE, Zhang B, Trout AT. Prognostic significance of pretreatment (18)F-FDG positron emission tomography/computed tomography in pediatric neuroblastoma. Pediatric radiology. 2021 Jul:51(8):1400-1405. doi: 10.1007/s00247-021-05005-y. Epub 2021 Feb 25 [PubMed PMID: 33629142]
Dadgar H, Norouzbeigi N, Ahmadzadehfar H, Assadi M. 68Ga-DOTATATE and 18F-FDG PET/CT for the Management of Esthesioneuroblastoma of the Sphenoclival Region. Clinical nuclear medicine. 2020 Aug:45(8):e363-e364. doi: 10.1097/RLU.0000000000003133. Epub [PubMed PMID: 32558717]
Gains JE, Aldridge MD, Mattoli MV, Bomanji JB, Biassoni L, Shankar A, Gaze MN. 68Ga-DOTATATE and 123I-mIBG as imaging biomarkers of disease localisation in metastatic neuroblastoma: implications for molecular radiotherapy. Nuclear medicine communications. 2020 Nov:41(11):1169-1177. doi: 10.1097/MNM.0000000000001265. Epub [PubMed PMID: 32796449]
Pauwels E, Celen S, Vandamme M, Leysen W, Baete K, Bechter O, Bex M, Serdons K, Van Laere K, Bormans G, Deroose CM. Improved resolution and sensitivity of [(18)F]MFBG PET compared with [(123)I]MIBG SPECT in a patient with a norepinephrine transporter-expressing tumour. European journal of nuclear medicine and molecular imaging. 2021 Jan:48(1):313-315. doi: 10.1007/s00259-020-04830-x. Epub 2020 May 8 [PubMed PMID: 32385645]
Chen H, Sippel RS, O'Dorisio MS, Vinik AI, Lloyd RV, Pacak K, North American Neuroendocrine Tumor Society (NANETS). The North American Neuroendocrine Tumor Society consensus guideline for the diagnosis and management of neuroendocrine tumors: pheochromocytoma, paraganglioma, and medullary thyroid cancer. Pancreas. 2010 Aug:39(6):775-83. doi: 10.1097/MPA.0b013e3181ebb4f0. Epub [PubMed PMID: 20664475]
Level 3 (low-level) evidenceRyder SJ, Love AJ, Duncan EL, Pattison DA. PET detectives: Molecular imaging for phaeochromocytomas and paragangliomas in the genomics era. Clinical endocrinology. 2021 Jul:95(1):13-28. doi: 10.1111/cen.14375. Epub 2020 Dec 9 [PubMed PMID: 33296100]
Taïeb D, Hicks RJ, Hindié E, Guillet BA, Avram A, Ghedini P, Timmers HJ, Scott AT, Elojeimy S, Rubello D, Virgolini IJ, Fanti S, Balogova S, Pandit-Taskar N, Pacak K. European Association of Nuclear Medicine Practice Guideline/Society of Nuclear Medicine and Molecular Imaging Procedure Standard 2019 for radionuclide imaging of phaeochromocytoma and paraganglioma. European journal of nuclear medicine and molecular imaging. 2019 Sep:46(10):2112-2137. doi: 10.1007/s00259-019-04398-1. Epub 2019 Jun 29 [PubMed PMID: 31254038]
Level 1 (high-level) evidenceJha A, Ling A, Millo C, Gupta G, Viana B, Lin FI, Herscovitch P, Adams KT, Taïeb D, Metwalli AR, Linehan WM, Brofferio A, Stratakis CA, Kebebew E, Lodish M, Civelek AC, Pacak K. Superiority of (68)Ga-DOTATATE over (18)F-FDG and anatomic imaging in the detection of succinate dehydrogenase mutation (SDHx )-related pheochromocytoma and paraganglioma in the pediatric population. European journal of nuclear medicine and molecular imaging. 2018 May:45(5):787-797. doi: 10.1007/s00259-017-3896-9. Epub 2017 Dec 4 [PubMed PMID: 29204718]
Timmers HJ, Chen CC, Carrasquillo JA, Whatley M, Ling A, Havekes B, Eisenhofer G, Martiniova L, Adams KT, Pacak K. Comparison of 18F-fluoro-L-DOPA, 18F-fluoro-deoxyglucose, and 18F-fluorodopamine PET and 123I-MIBG scintigraphy in the localization of pheochromocytoma and paraganglioma. The Journal of clinical endocrinology and metabolism. 2009 Dec:94(12):4757-67. doi: 10.1210/jc.2009-1248. Epub 2009 Oct 28 [PubMed PMID: 19864450]
Jaiswal SK, Sarathi V, Malhotra G, Hira P, Shah R, Patil VA, Dalvi A, Prakash G, Lila AR, Shah NS, Bandgar T. The utility of (68)Ga-DOTATATE PET/CT in localizing primary/metastatic pheochromocytoma and paraganglioma in children and adolescents - a single-center experience. Journal of pediatric endocrinology & metabolism : JPEM. 2021 Jan 27:34(1):109-119. doi: 10.1515/jpem-2020-0354. Epub 2020 Nov 12 [PubMed PMID: 33180042]
Jaiswal SK, Sarathi V, Memon SS, Garg R, Malhotra G, Verma P, Shah R, Sehemby MK, Patil VA, Jadhav S, Lila AR, Shah NS, Bandgar TR. 177Lu-DOTATATE therapy in metastatic/inoperable pheochromocytoma-paraganglioma. Endocrine connections. 2020 Oct:9(9):864-873. doi: 10.1530/EC-20-0292. Epub [PubMed PMID: 32784267]
Parghane RV, Talole S, Basu S. (131)I-MIBG negative progressive symptomatic metastatic paraganglioma: response and outcome with (177)Lu-DOTATATE peptide receptor radionuclide therapy. Annals of nuclear medicine. 2021 Jan:35(1):92-101. doi: 10.1007/s12149-020-01541-z. Epub 2020 Nov 1 [PubMed PMID: 33135123]
Patel M, Tena I, Jha A, Taieb D, Pacak K. Somatostatin Receptors and Analogs in Pheochromocytoma and Paraganglioma: Old Players in a New Precision Medicine World. Frontiers in endocrinology. 2021:12():625312. doi: 10.3389/fendo.2021.625312. Epub 2021 Mar 29 [PubMed PMID: 33854479]
Turnock S, Turton DR, Martins CD, Chesler L, Wilson TC, Gouverneur V, Smith G, Kramer-Marek G. (18)F-meta-fluorobenzylguanidine ((18)F-mFBG) to monitor changes in norepinephrine transporter expression in response to therapeutic intervention in neuroblastoma models. Scientific reports. 2020 Dec 1:10(1):20918. doi: 10.1038/s41598-020-77788-3. Epub 2020 Dec 1 [PubMed PMID: 33262374]
Pandit-Taskar N, Zanzonico P, Staton KD, Carrasquillo JA, Reidy-Lagunes D, Lyashchenko S, Burnazi E, Zhang H, Lewis JS, Blasberg R, Larson SM, Weber WA, Modak S. Biodistribution and Dosimetry of (18)F-Meta-Fluorobenzylguanidine: A First-in-Human PET/CT Imaging Study of Patients with Neuroendocrine Malignancies. Journal of nuclear medicine : official publication, Society of Nuclear Medicine. 2018 Jan:59(1):147-153. doi: 10.2967/jnumed.117.193169. Epub 2017 Jul 13 [PubMed PMID: 28705916]
Hassanzadeh-Rad A, Yousefifard M, Katal S, Asady H, Fard-Esfahani A, Moghadas Jafari A, Hosseini M. The value of (18) F-fluorodeoxyglucose positron emission tomography for prediction of treatment response in gastrointestinal stromal tumors: a systematic review and meta-analysis. Journal of gastroenterology and hepatology. 2016 May:31(5):929-35. doi: 10.1111/jgh.13247. Epub [PubMed PMID: 26642423]
Level 1 (high-level) evidenceRasheed R, Al-Kandari F, Ghanem M, Marafi F, Usmani S. Significance of 18F-FDG PET/CT in Characterization of Equivocal Lesions in High-Risk Testicular Carcinoma in Restaging Setting. Asian Pacific journal of cancer prevention : APJCP. 2020 Feb 1:21(2):511-515. doi: 10.31557/APJCP.2020.21.2.511. Epub 2020 Feb 1 [PubMed PMID: 32102532]
Cook GJ, Sohaib A, Huddart RA, Dearnaley DP, Horwich A, Chua S. The role of 18F-FDG PET/CT in the management of testicular cancers. Nuclear medicine communications. 2015 Jul:36(7):702-8. doi: 10.1097/MNM.0000000000000303. Epub [PubMed PMID: 25757201]
Level 2 (mid-level) evidenceSanchez D, Zudaire JJ, Fernandez JM, Lopez J, Arocena J, Sanz G, Gimenez M, Rosell D, Robles JE, Berian JM. 18F-fluoro-2-deoxyglucose-positron emission tomography in the evaluation of nonseminomatous germ cell tumours at relapse. BJU international. 2002 Jun:89(9):912-6 [PubMed PMID: 12010239]
Hain SF, O'Doherty MJ, Timothy AR, Leslie MD, Partridge SE, Huddart RA. Fluorodeoxyglucose PET in the initial staging of germ cell tumours. European journal of nuclear medicine. 2000 May:27(5):590-4 [PubMed PMID: 10853816]
Sharma P, Jain TK, Parida GK, Karunanithi S, Patel C, Sharma A, Thulkar S, Julka PK, Bal C, Kumar R. Diagnostic accuracy of integrated (18)F-FDG PET/CT for restaging patients with malignant germ cell tumours. The British journal of radiology. 2014 Aug:87(1040):20140263. doi: 10.1259/bjr.20140263. Epub 2014 Jun 4 [PubMed PMID: 24896199]
Level 2 (mid-level) evidenceHaddad T, Fard-Esfahani A, Vali R. A review of pediatric neuroendocrine tumors, their detection, and treatment by radioisotopes. Nuclear medicine communications. 2021 Jan:42(1):21-31. doi: 10.1097/MNM.0000000000001305. Epub [PubMed PMID: 33044400]
Foster JH, Sher A, Seghers V, Poston J, Wells D, Delpassand ES, Potter S, Mahajan P, Venkatramani R. Peptide receptor radionuclide therapy for treatment of metastatic neuroendocrine tumors in children. Pediatric blood & cancer. 2021 Jul:68(7):e29056. doi: 10.1002/pbc.29056. Epub 2021 Apr 12 [PubMed PMID: 33844446]
McElroy KM, Binkovitz LA, Trout AT, Czachowski MR, Seghers VJ, Lteif AN, States LJ. Pediatric applications of Dotatate: early diagnostic and therapeutic experience. Pediatric radiology. 2020 Jun:50(7):882-897. doi: 10.1007/s00247-020-04688-z. Epub 2020 Jun 3 [PubMed PMID: 32495176]
Goel R, Shukla J, Bansal D, Sodhi K, Bhattacharya A, Marwaha RK, Mittal BR. (68)Ga-DOTATATE positron emission tomography/computed tomography scan in the detection of bone metastases in pediatric neuroendocrine tumors. Indian journal of nuclear medicine : IJNM : the official journal of the Society of Nuclear Medicine, India. 2014 Jan:29(1):13-7. doi: 10.4103/0972-3919.125762. Epub [PubMed PMID: 24591776]
Bhavani N, Bhadran K, Nair V, Menon UV, Pavithran PV, Menon AS, Abraham N, Pankaj A, Kumar H. Treatment outcomes in pediatric differentiated thyroid carcinoma. Journal of pediatric endocrinology & metabolism : JPEM. 2018 Oct 25:31(10):1117-1122. doi: 10.1515/jpem-2018-0233. Epub [PubMed PMID: 30157034]
Pires BP, Alves PA Jr, Bordallo MA, Bulzico DA, Lopes FP, Farias T, Dias F, Lima RA, Santos Gisler IC, Coeli CM, Carvalhaes de Oliveira RV, Corbo R, Vaisman M, Vaisman F. Prognostic Factors for Early and Long-Term Remission in Pediatric Differentiated Thyroid Carcinoma: The Role of Sex, Age, Clinical Presentation, and the Newly Proposed American Thyroid Association Risk Stratification System. Thyroid : official journal of the American Thyroid Association. 2016 Oct:26(10):1480-1487 [PubMed PMID: 27540892]
Zanella AB, Scheffel RS, Nava CF, Golbert L, Laurini de Souza Meyer E, Punales M, Gonçalves I, Dora JM, Maia AL. Dynamic Risk Stratification in the Follow-Up of Children and Adolescents with Differentiated Thyroid Cancer. Thyroid : official journal of the American Thyroid Association. 2018 Oct:28(10):1285-1292. doi: 10.1089/thy.2018.0075. Epub [PubMed PMID: 30129889]
Lazar L, Lebenthal Y, Segal K, Steinmetz A, Strenov Y, Cohen M, Yaniv I, Yackobovitch-Gavan M, Phillip M. Pediatric Thyroid Cancer: Postoperative Classifications and Response to Initial Therapy as Prognostic Factors. The Journal of clinical endocrinology and metabolism. 2016 May:101(5):1970-9. doi: 10.1210/jc.2015-3960. Epub 2016 Mar 1 [PubMed PMID: 26930182]
Livhits MJ, Pasternak JD, Xiong M, Li N, Gosnell JE, Yeh MW, Chiu HK. PRE-ABLATION THYROGLOBULIN AND THYROGLOBULIN TO THYROID-STIMULATING HORMONE RATIO MAY BE ASSOCIATED WITH PULMONARY METASTASES IN CHILDREN WITH DIFFERENTIATED THYROID CANCER. Endocrine practice : official journal of the American College of Endocrinology and the American Association of Clinical Endocrinologists. 2016 Nov:22(11):1259-1266 [PubMed PMID: 27482611]
Quinn BM, Gao Y, Mahmood U, Pandit-Taskar N, Behr G, Zanzonico P, Dauer LT. Patient-adapted organ absorbed dose and effective dose estimates in pediatric 18F-FDG positron emission tomography/computed tomography studies. BMC medical imaging. 2020 Jan 29:20(1):9. doi: 10.1186/s12880-020-0415-4. Epub 2020 Jan 29 [PubMed PMID: 31996149]
Zampella E, Klain M, Pace L, Cuocolo A. PET/CT in the management of differentiated thyroid cancer. Diagnostic and interventional imaging. 2021 Sep:102(9):515-523. doi: 10.1016/j.diii.2021.04.004. Epub 2021 Apr 27 [PubMed PMID: 33926848]
Okuyucu K, Ince S, Alagoz E, Emer O, San H, Balkan E, Ayan A, Meric C, Haymana C, Acıkel C, Gunalp B, Karacalioglu AO, Arslan N. Risk factors and stratification for recurrence of patients with differentiated thyroid cancer, elevated thyroglobulin and negative I-131 whole-body scan, by restaging (18)F-FDG PET/CT. Hellenic journal of nuclear medicine. 2016 Sep-Dec:19(3):208-217. doi: 10.1967/s002449910402. Epub 2016 Nov 8 [PubMed PMID: 27824959]
Castinetti F, Taïeb D. Positron Emission Tomography Imaging in Medullary Thyroid Carcinoma: Time for Reappraisal? Thyroid : official journal of the American Thyroid Association. 2021 Feb:31(2):151-155. doi: 10.1089/thy.2020.0674. Epub 2020 Dec 23 [PubMed PMID: 33191866]
Sarikaya I, Sarikaya A. Current Status of Radionuclide Renal Cortical Imaging in Pyelonephritis. Journal of nuclear medicine technology. 2019 Dec:47(4):309-312. doi: 10.2967/jnmt.119.227942. Epub 2019 Jun 10 [PubMed PMID: 31182659]
Shaikh N, Shope TR, Hoberman A, Muniz GB, Bhatnagar S, Nowalk A, Hickey RW, Michaels MG, Kearney D, Rockette HE, Charron M, Lim R, Majd M, Shalaby-Rana E, Kurs-Lasky M, Cohen DM, Wald ER, Lockhart G, Pohl HG, Martin JM. Corticosteroids to prevent kidney scarring in children with a febrile urinary tract infection: a randomized trial. Pediatric nephrology (Berlin, Germany). 2020 Nov:35(11):2113-2120. doi: 10.1007/s00467-020-04622-3. Epub 2020 Jun 15 [PubMed PMID: 32556960]
Level 1 (high-level) evidenceEinarsdóttir HS, Berg RMG, Borgwardt L. Interrater Reliability of (99m)Tc-DMSA Scintigraphy Performed as Planar Scan vs. SPECT/Low Dose CT for Diagnosing Renal Scarring in Children. Diagnostics (Basel, Switzerland). 2020 Dec 17:10(12):. doi: 10.3390/diagnostics10121101. Epub 2020 Dec 17 [PubMed PMID: 33348530]
Ozen C, Ertan P, Aras F, Gumuser G, Ozkol M, Horasan Dinc G. Evaluation of abnormal radiological findings in children aged 2 to 36 months followed by recurrent urinary tract infection: a retrospective study. Renal failure. 2017 Nov:39(1):100-103. doi: 10.1080/0886022X.2016.1251460. Epub 2016 Nov 6 [PubMed PMID: 27819162]
Level 2 (mid-level) evidenceRoupakias S, Sinopidis X, Tsikopoulos G, Spyridakis I, Karatza A, Varvarigou A. Dimercaptosuccinic acid scan challenges in childhood urinary tract infection, vesicoureteral reflux and renal scarring investigation and management. Minerva urologica e nefrologica = The Italian journal of urology and nephrology. 2017 Apr:69(2):144-152. doi: 10.23736/S0393-2249.16.02509-1. Epub 2016 Jun 29 [PubMed PMID: 27355216]
Breinbjerg A, Jørgensen CS, Frøkiær J, Tullus K, Kamperis K, Rittig S. Risk factors for kidney scarring and vesicoureteral reflux in 421 children after their first acute pyelonephritis, and appraisal of international guidelines. Pediatric nephrology (Berlin, Germany). 2021 Sep:36(9):2777-2787. doi: 10.1007/s00467-021-05042-7. Epub 2021 Mar 23 [PubMed PMID: 33754234]
Arapović A, Punda A, Brdar D, Čapkun V, Bajo D, Veljačić D, Punda H, Simičić-Majce A, Saraga-Babić M, Vukojević K, Saraga M. Types of Parenchymal Changes Diagnosed on DMSA Scans of Kidneys Affected by Different Grades of Vesicoureteral Reflux. Medical science monitor : international medical journal of experimental and clinical research. 2021 Mar 1:27():e929617. doi: 10.12659/MSM.929617. Epub 2021 Mar 1 [PubMed PMID: 33647007]
Lee JN, Kang JK, Jeong SY, Lee SM, Cho MH, Ha YS, Kim HT, Kim TH, Yoo ES, Kwon TG, Chung SK. Predictive value of cortical transit time on MAG3 for surgery in antenatally detected unilateral hydronephrosis caused by ureteropelvic junction stenosis. Journal of pediatric urology. 2018 Feb:14(1):55.e1-55.e6. doi: 10.1016/j.jpurol.2017.08.009. Epub 2017 Sep 19 [PubMed PMID: 28988673]
Faure A, London K, Smith GH. Early mercaptoacetyltriglycine(MAG-3) diuretic renography results after pyeloplasty. BJU international. 2016 Nov:118(5):790-796. doi: 10.1111/bju.13512. Epub 2016 May 25 [PubMed PMID: 27105017]
Pui MH, Yueh TC. Lymphoscintigraphy in chyluria, chyloperitoneum and chylothorax. Journal of nuclear medicine : official publication, Society of Nuclear Medicine. 1998 Jul:39(7):1292-6 [PubMed PMID: 9669413]
Level 2 (mid-level) evidenceTurpin S, Lambert R. Lymphoscintigraphy of Chylous Anomalies: Chylothorax, Chyloperitoneum, Chyluria, and Lymphangiomatosis-15-Year Experience in a Pediatric Setting and Review of the Literature. Journal of nuclear medicine technology. 2018 Jun:46(2):123-128. doi: 10.2967/jnmt.117.203281. Epub 2018 Feb 2 [PubMed PMID: 29438003]
Bellini C, Villa G, Sambuceti G, Traggiai C, Campisi C, Bellini T, Morcaldi G, Massocco D, Bonioli E, Boccardo F. Lymphoscintigraphy patterns in newborns and children with congenital lymphatic dysplasia. Lymphology. 2014 Mar:47(1):28-39 [PubMed PMID: 25109167]
Watt H, Singh-Grewal D, Wargon O, Adams S. Paediatric lymphoedema: A retrospective chart review of 86 cases. Journal of paediatrics and child health. 2017 Jan:53(1):38-42. doi: 10.1111/jpc.13305. Epub 2016 Oct 4 [PubMed PMID: 27701785]
Level 2 (mid-level) evidenceKuo PH, Barber BJ, Kylat RI, Klewer SE, Behan S, Lau-Braunhut S, Bernas MJ, Moedano L, Bedrick AD, Mustacich DJ, Witte MH. Whole-body lymphangioscintigraphy and SPECT/CT in children with lymphatic complications after surgery for complex congenital heart disease. Lymphology. 2019:52(4):157-165 [PubMed PMID: 32171182]
Hou G, Jiang Y, Jing H, Xu W, Xu KF, Chen L, Li F, Cheng W. Usefulness of 99mTc-ASC lymphoscintigraphy and SPECT/CT in the evaluation of rare lymphatic disorders: Gorham-Stout disease, lymphangioma, and lymphangioleiomyomatosis. Medicine. 2020 Sep 25:99(39):e22414. doi: 10.1097/MD.0000000000022414. Epub [PubMed PMID: 32991473]
Law ST, Ma KM, Li KK. The clinical characteristics of lupus related protein-losing enteropathy in Hong Kong Chinese population: 10 years of experience from a regional hospital. Lupus. 2012 Jul:21(8):840-7. doi: 10.1177/0961203312438113. Epub 2012 Feb 17 [PubMed PMID: 22343095]
Level 2 (mid-level) evidenceChau TN, Mok MY, Chan EY, Luk WH, Lai KB, Li FT, Leung VK, Wong R. Evaluation of performance of measurement of faecal α(1)-antitrypsin clearance and technetium-99m human serum albumin scintigraphy in protein-losing enteropathy. Digestion. 2011:84(3):199-206. doi: 10.1159/000327914. Epub 2011 Jul 8 [PubMed PMID: 21757911]
Level 2 (mid-level) evidenceHalaby H, Bakheet SM, Shabib S, Powe JE, Al Mehaidib A, Nazer H. 99mTc-human serum albumin scans in children with protein-losing enteropathy. Journal of nuclear medicine : official publication, Society of Nuclear Medicine. 2000 Feb:41(2):215-9 [PubMed PMID: 10688102]
Level 2 (mid-level) evidenceChiu NT, Lee BF, Hwang SJ, Chang JM, Liu GC, Yu HS. Protein-losing enteropathy: diagnosis with (99m)Tc-labeled human serum albumin scintigraphy. Radiology. 2001 Apr:219(1):86-90 [PubMed PMID: 11274540]
Snyder E, Kashyap S, Lopez PP. Hepatobiliary Iminodiacetic Acid Scan. StatPearls. 2023 Jan:(): [PubMed PMID: 30969603]
Stagg H, Cameron BH, Ahmed N, Butler A, Jimenez-Rivera C, Yanchar NL, Martin SR, Emil S, Anthopoulos G, Schreiber RA, Laberge JM, Canadian Biliary Atresia Registry. Variability of diagnostic approach, surgical technique, and medical management for children with biliary atresia in Canada - Is it time for standardization? Journal of pediatric surgery. 2017 May:52(5):802-806. doi: 10.1016/j.jpedsurg.2017.01.041. Epub 2017 Jan 30 [PubMed PMID: 28189446]
Shah I, Bhatnagar S, Rangarajan V, Patankar N. Utility of Tc99m-Mebrofenin hepato-biliary scintigraphy (HIDA scan) for the diagnosis of biliary atresia. Tropical gastroenterology : official journal of the Digestive Diseases Foundation. 2012 Jan-Mar:33(1):62-4 [PubMed PMID: 22803298]
Level 2 (mid-level) evidenceRobie DK, Overfelt SR, Xie L. Differentiating biliary atresia from other causes of cholestatic jaundice. The American surgeon. 2014 Sep:80(9):827-31 [PubMed PMID: 25197861]
Level 2 (mid-level) evidenceJancelewicz T, Barmherzig R, Chung CT, Ling SC, Kamath BM, Ng VL, Amaral J, O'Connor C, Fecteau A, Langer JC. A screening algorithm for the efficient exclusion of biliary atresia in infants with cholestatic jaundice. Journal of pediatric surgery. 2015 Mar:50(3):363-70. doi: 10.1016/j.jpedsurg.2014.08.014. Epub [PubMed PMID: 25746690]
Level 2 (mid-level) evidenceFares M, Critser PJ, Arruda MJ, Wilhelm CM, Rattan MS, Lang SM, Alsaied T. Pharmacologic stress cardiovascular magnetic resonance in the pediatric population: A review of the literature, proposed protocol, and two examples in patients with Kawasaki disease. Congenital heart disease. 2019 Nov:14(6):1166-1175. doi: 10.1111/chd.12840. Epub 2019 Sep 9 [PubMed PMID: 31498562]
Doan TT, Wilkinson JC, Loar RW, Pednekar AS, Masand PM, Noel CV. Regadenoson Stress Perfusion Cardiac Magnetic Resonance Imaging in Children With Kawasaki Disease and Coronary Artery Disease. The American journal of cardiology. 2019 Oct 1:124(7):1125-1132. doi: 10.1016/j.amjcard.2019.06.033. Epub 2019 Jul 16 [PubMed PMID: 31371063]
Abe T, Tsuda E, Sugiyama H, Kiso K, Yamada O. Risk factors of non-sustained ventricular tachycardia by technetium-perfusion imaging in patients with coronary artery lesions caused by Kawasaki disease. Journal of cardiology. 2019 May:73(5):358-362. doi: 10.1016/j.jjcc.2018.12.007. Epub 2018 Dec 31 [PubMed PMID: 30606680]
Vijarnsorn C, Noga M, Schantz D, Pepelassis D, Tham EB. Stress perfusion magnetic resonance imaging to detect coronary artery lesions in children. The international journal of cardiovascular imaging. 2017 May:33(5):699-709. doi: 10.1007/s10554-016-1041-7. Epub 2016 Dec 20 [PubMed PMID: 28000002]
Kamiyama H, Karasawa K. [Cardiac scintigraphy-Pharmacological stress and appropriate management of pediatric radiopharmaceutical administration in patients after Kawasaki disease]. Nihon rinsho. Japanese journal of clinical medicine. 2014 Sep:72(9):1595-600 [PubMed PMID: 25518408]
Abe M, Fukazawa R, Ogawa S, Watanabe M, Fukushima Y, Kiriyama T, Hayashi H, Itoh Y. Usefulness of Single Photon Emission Computed Tomography/Computed Tomography Fusion-Hybrid Imaging to Evaluate Coronary Artery Disorders in Patients with a History of Kawasaki Disease. Journal of Nippon Medical School = Nippon Ika Daigaku zasshi. 2016:83(2):71-80. doi: 10.1272/jnms.83.71. Epub [PubMed PMID: 27180792]
Doan TT, Molossi S, Sachdeva S, Wilkinson JC, Loar RW, Weigand JD, Schlingmann TR, Reaves-O'Neal DL, Pednekar AS, Masand P, Noel CV. Dobutamine stress cardiac MRI is safe and feasible in pediatric patients with anomalous aortic origin of a coronary artery (AAOCA). International journal of cardiology. 2021 Jul 1:334():42-48. doi: 10.1016/j.ijcard.2021.04.031. Epub 2021 Apr 20 [PubMed PMID: 33892043]
Doan TT, Zea-Vera R, Agrawal H, Mery CM, Masand P, Reaves-O'Neal DL, Noel CV, Qureshi AM, Sexson-Tejtel SK, Fraser CD Jr, Molossi S. Myocardial Ischemia in Children With Anomalous Aortic Origin of a Coronary Artery With Intraseptal Course. Circulation. Cardiovascular interventions. 2020 Mar:13(3):e008375. doi: 10.1161/CIRCINTERVENTIONS.119.008375. Epub 2020 Feb 27 [PubMed PMID: 32102565]
Sinha CK, Pallewatte A, Easty M, De Coppi P, Pierro A, Misra D, Biassoni L. Meckel's scan in children: a review of 183 cases referred to two paediatric surgery specialist centres over 18 years. Pediatric surgery international. 2013 May:29(5):511-7. doi: 10.1007/s00383-013-3270-3. Epub 2013 Feb 16 [PubMed PMID: 23417523]
Level 2 (mid-level) evidenceVali R, Daneman A, McQuattie S, Shammas A. The value of repeat scintigraphy in patients with a high clinical suspicion for Meckel diverticulum after a negative or equivocal first Meckel scan. Pediatric radiology. 2015 Sep:45(10):1506-14. doi: 10.1007/s00247-015-3340-x. Epub 2015 Apr 7 [PubMed PMID: 25846077]
Dillman JR, Wong KK, Brown RK, Frey KA, Strouse PJ. Utility of SPECT/CT with Meckel's scintigraphy. Annals of nuclear medicine. 2009 Nov:23(9):813-5. doi: 10.1007/s12149-009-0301-1. Epub 2009 Sep 29 [PubMed PMID: 19784878]
Level 3 (low-level) evidenceMorbelli S, Djekidel M, Hesse S, Pagani M, Barthel H, Neuroimaging Committee of the European Association of Nuclear Medicine (EANM), Brain Imaging Council of the Society of Nuclear Medicine and Molecular Imaging (SNMMI). Role of (18)F-FDG-PET imaging in the diagnosis of autoimmune encephalitis. The Lancet. Neurology. 2016 Sep:15(10):1009-10. doi: 10.1016/S1474-4422(16)30140-5. Epub 2016 Aug 8 [PubMed PMID: 27571149]
Morbelli S, Arbizu J, Booij J, Chen MK, Chetelat G, Cross DJ, Djekidel M, Drzezga A, Ekmekcioglu O, Garibotto V, Hesse S, Ishii K, Jafari L, Lammertsma AA, Law I, Mathews D, Minoshima S, Mosci K, Pagani M, Pappata S, Silverman DH, Signore A, Van De Giessen E, Villemagne V, Barthel H, European Association of Nuclear Medicine (EANM) and of the Society of Nuclear Medicine and Molecular Imaging (SNMMI). The need of standardization and of large clinical studies in an emerging indication of [(18)F]FDG PET: the autoimmune encephalitis. European journal of nuclear medicine and molecular imaging. 2017 Mar:44(3):353-357. doi: 10.1007/s00259-016-3589-9. Epub 2016 Dec 6 [PubMed PMID: 27924371]
Djekidel M. (18)F-FDG PET Imaging Predicts the Epileptogenic Zone Prospectively in Recurrent Cryptogenic Meningoencephalitis with Subsequent Simple Partial Visual Seizures. Journal of nuclear medicine technology. 2021 Mar:49(1):92-94. doi: 10.2967/jnmt.120.252866. Epub 2020 Nov 20 [PubMed PMID: 33219155]
Grosse F, Wedel F, Thomale UW, Steffen I, Koch A, Brenner W, Plotkin M, Driever PH. Benefit of Static FET PET in Pretreated Pediatric Brain Tumor Patients with Equivocal Conventional MRI Results. Klinische Padiatrie. 2021 May:233(3):127-134. doi: 10.1055/a-1335-4844. Epub 2021 Feb 17 [PubMed PMID: 33598897]
Somme F, Bender L, Namer IJ, Noël G, Bund C. Usefulness of (18)F-FDOPA PET for the management of primary brain tumors: a systematic review of the literature. Cancer imaging : the official publication of the International Cancer Imaging Society. 2020 Oct 6:20(1):70. doi: 10.1186/s40644-020-00348-5. Epub 2020 Oct 6 [PubMed PMID: 33023662]
Level 1 (high-level) evidenceTatekawa H, Yao J, Oughourlian TC, Hagiwara A, Wang C, Raymond C, Lai A, Cloughesy TF, Nghiemphu PL, Liau LM, Salamon N, Ellingson BM. Maximum Uptake and Hypermetabolic Volume of 18F-FDOPA PET Estimate Molecular Status and Overall Survival in Low-Grade Gliomas: A PET and MRI Study. Clinical nuclear medicine. 2020 Dec:45(12):e505-e511. doi: 10.1097/RLU.0000000000003318. Epub [PubMed PMID: 33031233]
Tatekawa H, Hagiwara A, Yao J, Oughourlian TC, Ueda I, Uetani H, Raymond C, Lai A, Cloughesy TF, Nghiemphu PL, Liau LM, Pope WB, Salamon N, Ellingson BM. Voxelwise and Patientwise Correlation of (18)F-FDOPA PET, Relative Cerebral Blood Volume, and Apparent Diffusion Coefficient in Treatment-Naïve Diffuse Gliomas with Different Molecular Subtypes. Journal of nuclear medicine : official publication, Society of Nuclear Medicine. 2021 Mar:62(3):319-325. doi: 10.2967/jnumed.120.247411. Epub 2020 Jul 9 [PubMed PMID: 32646876]
Qian J, Herman MG, Brinkmann DH, Laack NN, Kemp BJ, Hunt CH, Lowe V, Pafundi DH. Prediction of MGMT Status for Glioblastoma Patients Using Radiomics Feature Extraction From (18)F-DOPA-PET Imaging. International journal of radiation oncology, biology, physics. 2020 Dec 1:108(5):1339-1346. doi: 10.1016/j.ijrobp.2020.06.073. Epub 2020 Jul 4 [PubMed PMID: 32634544]
Level 2 (mid-level) evidenceCastello A, Riva M, Fernandes B, Bello L, Lopci E. The role of 11C-methionine PET in patients with negative diffusion-weighted magnetic resonance imaging: correlation with histology and molecular biomarkers in operated gliomas. Nuclear medicine communications. 2020 Jul:41(7):696-705. doi: 10.1097/MNM.0000000000001202. Epub [PubMed PMID: 32371671]
Spies AJ, Steyn M, Bussy E, Brits D. Forensic imaging: The sensitivities of various imaging modalities in detecting skeletal trauma in simulated cases of child abuse using a pig model. Journal of forensic and legal medicine. 2020 Nov:76():102034. doi: 10.1016/j.jflm.2020.102034. Epub 2020 Aug 6 [PubMed PMID: 33208232]
Level 3 (low-level) evidenceChuang YW, Hsu CC, Chang CC, Lin CY, Chu HL, Huang YF, Tyan YC. Multiple Bony Injuries on Bone Scan in a Case of Unsuspected Child Abuse. Case reports in medicine. 2017:2017():3015941. doi: 10.1155/2017/3015941. Epub 2017 Jun 27 [PubMed PMID: 28740509]
Level 3 (low-level) evidenceBorn M, Schwier F, Stoever B, Mentzel HJ, Freiberg J. The German Evidence-Based Child Protection Guideline - Imaging in Suspected Child Abuse. RoFo : Fortschritte auf dem Gebiete der Rontgenstrahlen und der Nuklearmedizin. 2020 Apr:192(4):343-348. doi: 10.1055/a-1019-8018. Epub 2019 Nov 20 [PubMed PMID: 31747703]
Bainbridge JK, Huey BM, Harrison SK. Should bone scintigraphy be used as a routine adjunct to skeletal survey in the imaging of non-accidental injury? A 10 year review of reports in a single centre. Clinical radiology. 2015 Aug:70(8):e83-9. doi: 10.1016/j.crad.2015.04.012. Epub 2015 Jun 6 [PubMed PMID: 26055408]
Level 3 (low-level) evidenceDrubach LA. Nuclear Medicine Techniques in Pediatric Bone Imaging. Seminars in nuclear medicine. 2017 May:47(3):190-203. doi: 10.1053/j.semnuclmed.2016.12.006. Epub 2017 Jan 12 [PubMed PMID: 28417851]
Valanne L, Föhr A. [Radiological examinations in suspected physical abuse of a child]. Duodecim; laaketieteellinen aikakauskirja. 2015:131(10):1000-7 [PubMed PMID: 26237881]
Grant FD. ¹⁸F-fluoride PET and PET/CT in children and young adults. PET clinics. 2014 Jul:9(3):287-97. doi: 10.1016/j.cpet.2014.03.004. Epub [PubMed PMID: 25030392]
Niccoli Asabella A, Stabile Ianora AA, Di Palo A, Rubini D, Pisani AR, Ferrari C, Notaristefano A, Rubini G. [Lung perfusion scintigraphy in pediatric patients with congenital malformations]. Recenti progressi in medicina. 2013 Jul-Aug:104(7-8):442-5. doi: 10.1701/1315.14593. Epub [PubMed PMID: 24042425]
Level 3 (low-level) evidenceWise-Faberowski L, Irvin M, Lennig M, Long J, Nadel HR, Bauser-Heaton H, Asija R, Hanley FL, McElhinney DB. Assessment of the Reconstructed Pulmonary Circulation With Lung Perfusion Scintigraphy After Unifocalization and Repair of Tetralogy of Fallot With Major Aortopulmonary Collaterals. World journal for pediatric & congenital heart surgery. 2019 May:10(3):313-320. doi: 10.1177/2150135119836735. Epub [PubMed PMID: 31084304]
Asabella AN, Cimino A, Altini C, Lavelli V, Rubini G. Lung Perfusion Imaging in Tetralogy of Fallot: A Case Report. Molecular imaging and radionuclide therapy. 2018 Oct 9:27(3):146-148. doi: 10.4274/mirt.04909. Epub [PubMed PMID: 30317856]
Level 3 (low-level) evidenceChien KJ, Huang HW, Huang TC, Lee CL, Weng KP, Lin CC, Shieh PC, Wu MT, Hsieh KS. Assessment of branch pulmonary artery stenosis in children after repair of tetralogy of Fallot using lung perfusion scintigraphy comparison with echocardiography. Annals of nuclear medicine. 2016 Jan:30(1):49-59 [PubMed PMID: 26493388]
Rubió Rodríguez A, Ferran Sureda N, Balliu Collgròs E, Uriel Prat S, Galofré Mora P. [Unilateral ventilation/perfusión (V/Q) mismatch in a child with corrected congenital heart disease]. Revista espanola de medicina nuclear. 2009 Jan-Feb:28(1):30-1 [PubMed PMID: 19232176]
Level 3 (low-level) evidenceKamal A, Sarvepalli S, Selvakumar P, Lopez R, Radhakrishnan K, Gabbard S. Assessment of Gastric Emptying Times Between Pediatrics and Adults With Cyclic Vomiting Syndrome. Journal of clinical gastroenterology. 2020 Oct:54(9):e89-e92. doi: 10.1097/MCG.0000000000001352. Epub [PubMed PMID: 32569030]
Kwatra NS, Shalaby-Rana E, Andrich MP, Tsai J, Rice AL, Ghelani SJ, Spottswood SE, Majd M. Gastric emptying of milk in infants and children up to 5 years of age: normative data and influencing factors. Pediatric radiology. 2020 May:50(5):689-697. doi: 10.1007/s00247-020-04614-3. Epub 2020 Jan 28 [PubMed PMID: 31993707]
Edwards ST, Cocjin J, Theut SB, Rivard D, Sherman AK, Friesen CA. A comparison of the diagnosis of gastroparesis in 4 h pediatric gastric emptying studies versus 2 h studies. BMC gastroenterology. 2019 Feb 11:19(1):26. doi: 10.1186/s12876-019-0948-6. Epub 2019 Feb 11 [PubMed PMID: 30744574]
Du T, Hill L, Ding L, Towbin AJ, DeJonckheere M, Bennett P, Hagerman N, Varughese AM, Pratap JN. Gastric emptying for liquids of different compositions in children. British journal of anaesthesia. 2017 Nov 1:119(5):948-955. doi: 10.1093/bja/aex340. Epub [PubMed PMID: 29077812]
Wu H, Zhao R. Image characteristics and classification of salivagram in the diagnosis of pulmonary aspiration in children. Nuclear medicine communications. 2017 Jul:38(7):617-622. doi: 10.1097/MNM.0000000000000688. Epub [PubMed PMID: 28471844]
Shao F, Zhao X, Toyama H, Ichihara T, Zhuang H, Zhao R, Kung BT, Ng KS, Zhang Z, Wu H. Semi-quantitative assessment optimized the grading of pulmonary aspiration on salivagram in children. Annals of nuclear medicine. 2021 Mar:35(3):321-327. doi: 10.1007/s12149-020-01564-6. Epub 2021 Feb 8 [PubMed PMID: 33555558]
Kim GE, Sung IY, Ko EJ, Choi KH, Kim JS. Comparison of Videofluoroscopic Swallowing Study and Radionuclide Salivagram for Aspiration Pneumonia in Children With Swallowing Difficulty. Annals of rehabilitation medicine. 2018 Feb:42(1):52-58. doi: 10.5535/arm.2018.42.1.52. Epub 2018 Feb 28 [PubMed PMID: 29560324]
Wu H, Zhao X, Ting Kung B, Sing Ng K. Effect of nasogastric tube on salivagram result in paediatric patients. Nuclear medicine communications. 2019 Sep:40(9):894-897. doi: 10.1097/MNM.0000000000001052. Epub [PubMed PMID: 31343616]
Li Q, Tian R, Sun X. More Evidence Is Warranted to Establish the Role of 18FDG-PET/CT in Fever of Unknown Origin (FUO) Investigations Among Children. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 2021 Nov 2:73(9):e2842-e2844. doi: 10.1093/cid/ciaa1574. Epub [PubMed PMID: 33064795]
Pijl JP, Kwee TC, Legger GE, Peters HJH, Armbrust W, Schölvinck EH, Glaudemans AWJM. Role of FDG-PET/CT in children with fever of unknown origin. European journal of nuclear medicine and molecular imaging. 2020 Jun:47(6):1596-1604. doi: 10.1007/s00259-020-04707-z. Epub 2020 Feb 7 [PubMed PMID: 32030452]
Shimizu M, Ikawa Y, Mizuta M, Takakura M, Inoue N, Nishimura R, Yachie A. FDG-PET in macrophage activation syndrome associated with systemic juvenile idiopathic arthritis. Pediatrics international : official journal of the Japan Pediatric Society. 2017 Apr:59(4):509-511. doi: 10.1111/ped.13238. Epub [PubMed PMID: 28401744]
Shimizu M, Saikawa Y, Yachie A. Role of 18-fluoro-2-deoxyglucose positron emission tomography in detecting acute inflammatory lesions of non-bacterial osteitis in patients with a fever of unknown origin: A comparative study of 18-fluoro-2-deoxyglucose positron emission tomography, bone scan, and magnetic resonance imaging. Modern rheumatology. 2018 Nov:28(6):1058-1062. doi: 10.1080/14397595.2016.1193112. Epub 2016 Jun 20 [PubMed PMID: 27321232]
Level 2 (mid-level) evidenceGarg G, DaSilva R, Bhalakia A, Milstein DM. Utility of fluorine-18-fluorodeoxyglucose positron emission tomography/computed tomography in a child with chronic granulomatous disease. Indian journal of nuclear medicine : IJNM : the official journal of the Society of Nuclear Medicine, India. 2016 Jan-Mar:31(1):62-4. doi: 10.4103/0972-3919.172366. Epub [PubMed PMID: 26917900]
Chang L, Cheng MF, Jou ST, Ko CL, Huang JY, Tzen KY, Yen RF. Search of Unknown Fever Focus Using PET in Critically Ill Children With Complicated Underlying Diseases. Pediatric critical care medicine : a journal of the Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies. 2016 Feb:17(2):e58-65. doi: 10.1097/PCC.0000000000000601. Epub [PubMed PMID: 26649939]
Jiménez D, Soto ME, Martínez-Martínez LA, Hernández-López D, Lerma C, Barragán-Garfias JA, Pérez-Torres I, Hernández-Lemus E, Guarner-Lans V. Assessment of inflammatory activity in Takayasu's arteritis: performance of clinical scores and common biomarkers versus 18F-FDG PET/CT. Clinical and experimental rheumatology. 2021 Sep-Oct:39(5):1011-1020. doi: 10.55563/clinexprheumatol/a71bzh. Epub 2020 Oct 29 [PubMed PMID: 33124558]
Kawamura J, Ueno K, Taimura E, Matsuba T, Imoto Y, Jinguji M, Kawano Y. Case Report: (18)F-FDG PET-CT for Diagnosing Prosthetic Device-Related Infection in an Infant With CHD. Frontiers in pediatrics. 2021:9():584741. doi: 10.3389/fped.2021.584741. Epub 2021 Mar 8 [PubMed PMID: 33763393]
Level 3 (low-level) evidenceAslanidis IP, Pursanova DM, Mukhortova OV, Shurupova IV, Ekaeva IV, Arakelyan VS, Golukhova EZ, Mironenko VA, Garmanov SV, Popov DA. [18F-fluorodeoxyglucose PET/CT in the diagnosis of vascular graft infection]. Khirurgiia. 2021:(2):58-66. doi: 10.17116/hirurgia202102158. Epub [PubMed PMID: 33570356]
Cremer PC. Diagnostic Uncertainty in Prosthetic Valve Endocarditis: Value of (18)F-FDG PET/CT and the Need for Standardization. JACC. Cardiovascular imaging. 2020 Dec:13(12):2616-2618. doi: 10.1016/j.jcmg.2020.06.023. Epub 2020 Aug 19 [PubMed PMID: 32828768]
Jerónimo A, Olmos C, Vilacosta I, Ortega-Candil A, Rodríguez-Rey C, Pérez-Castejón MJ, Fernández-Pérez C, Pérez-García CN, García-Arribas D, Ferrera C, Carreras JL. Accuracy of (18)F-FDG PET/CT in patients with the suspicion of cardiac implantable electronic device infections. Journal of nuclear cardiology : official publication of the American Society of Nuclear Cardiology. 2022 Apr:29(2):594-608. doi: 10.1007/s12350-020-02285-z. Epub 2020 Aug 3 [PubMed PMID: 32748277]
Gobbo MY, Meretta AH, Rosa D, Corneli M, Daquarti GJ, Masoli OH, Grymberg L, Pérez Baliño N, Nacinovich F, Ronderos R. [Positron emission tomography in infective endocarditis associated with intracardiac devices and prosthetic valves]. Medicina. 2020:80(1):17-22 [PubMed PMID: 32044737]
Treglia G. Diagnostic Performance of (18)F-FDG PET/CT in Infectious and Inflammatory Diseases according to Published Meta-Analyses. Contrast media & molecular imaging. 2019:2019():3018349. doi: 10.1155/2019/3018349. Epub 2019 Jul 25 [PubMed PMID: 31427907]
Chen W, Sajadi MM, Dilsizian V. Merits of FDG PET/CT and Functional Molecular Imaging Over Anatomic Imaging With Echocardiography and CT Angiography for the Diagnosis of Cardiac Device Infections. JACC. Cardiovascular imaging. 2018 Nov:11(11):1679-1691. doi: 10.1016/j.jcmg.2018.08.026. Epub [PubMed PMID: 30409329]
Diemberger I, Bonfiglioli R, Martignani C, Graziosi M, Biffi M, Lorenzetti S, Ziacchi M, Nanni C, Fanti S, Boriani G. Contribution of PET imaging to mortality risk stratification in candidates to lead extraction for pacemaker or defibrillator infection: a prospective single center study. European journal of nuclear medicine and molecular imaging. 2019 Jan:46(1):194-205. doi: 10.1007/s00259-018-4142-9. Epub 2018 Sep 8 [PubMed PMID: 30196365]
Blanc P, Bonnet E, Giordano G, Monteil J, Salabert AS, Payoux P. The use of labelled leucocyte scintigraphy to evaluate chronic periprosthetic joint infections: a retrospective multicentre study on 168 patients. European journal of clinical microbiology & infectious diseases : official publication of the European Society of Clinical Microbiology. 2019 Sep:38(9):1625-1631. doi: 10.1007/s10096-019-03587-y. Epub 2019 Jun 20 [PubMed PMID: 31218592]
Level 2 (mid-level) evidenceDjekidel M, Brown RK, Piert M. Benefits of hybrid SPECT/CT for (111)In-oxine- and Tc-99m-hexamethylpropylene amine oxime-labeled leukocyte imaging. Clinical nuclear medicine. 2011 Jul:36(7):e50-6. doi: 10.1097/RLU.0b013e31821738a0. Epub [PubMed PMID: 21637042]