Introduction
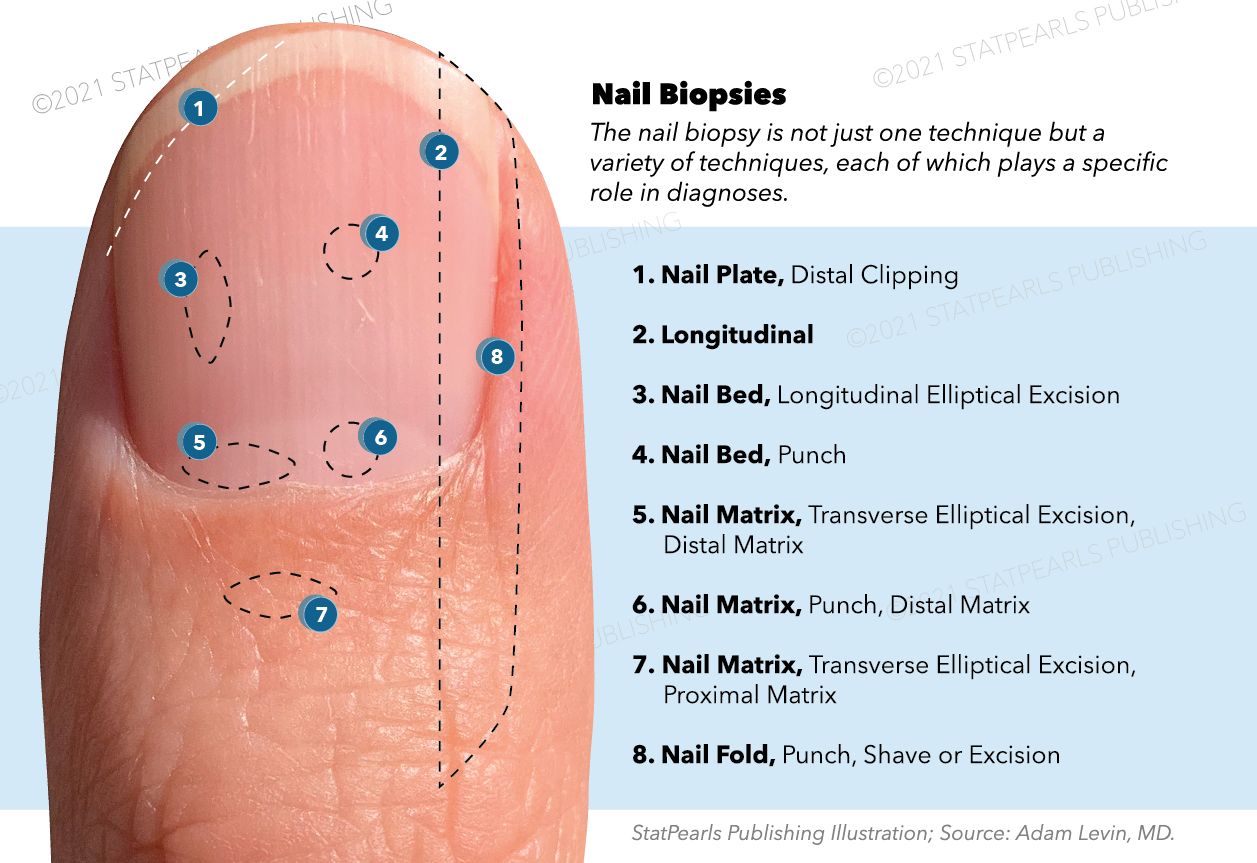
The nail biopsy is an essential procedure utilized by dermatologists to establish the diagnosis of a variety of skin and nail pathologies. The nail biopsy encompasses several biopsy techniques that include but are not limited to the nail plate, nail bed, nail fold, and nail matrix.[1][2]
The favored underlying diagnosis often determines the site of the biopsy and the techniques employed. The nail matrix is very delicate and carries its own biopsy risks and side effects. Even so, the majority of nail biopsies carry minimal to no risk of permanent nail dystrophy.[3]
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
The nail matrix is a crescent-shaped structure at the base of the nail, which produces the nail plate. Damage to the matrix may lead to scarring and dystrophy of the nail. The matrix is divided into proximal and distal; the proximal matrix is responsible for producing the superficial nail plate, while the distal matrix is responsible for the inferior nail plate. Biopsy of the distal matrix is less likely to produce scarring. The subcutaneous tissue inferior to the nail plate is quite thin, making it easy to reach the bone of the distal phalange. The extensor tendon of each digit is estimated to be approximately 12 mm proximal from the nail cuticle and, therefore, unlikely to be damaged during a routine biopsy.[2]
The nail unit receives its arterial supply from the proper digital arteries that run along with the digits on the medial and lateral aspects. The venous system predominately mirrors the course of the arterial supply. The 2nd, 3rd, and 4th nail digits are innervated by the volar proper digital nerves, while the 1st and 5th nail digits are innervated by the dorsal proper digital nerves.[4][5]
Indications
A nail biopsy is indicated in various pathologies, including infectious, inflammatory, autoimmune, traumatic, and oncologic. This is generally performed when the pathology is isolated to the nail unit.[1]
Common pathologic entities diagnosed via nail biopsy includes onychomycosis, psoriasis, lichen planus, twenty nail dystrophy, melanonychia, melanoma, and benign tumors of the nail unit.
Contraindications
Relative contraindications to nail biopsy include peripheral vascular disease and arterial compromise. As in any procedure, proper consent should be taken before the procedure being performed.[3]
Equipment
Antiseptic Agents
- Often alcohol or chlorhexidine, a variety of other antiseptics are suitable for nail biopsy.
Local Anesthetic
- The most commonly used local anesthetic is a 1% lidocaine solution.
- To decrease pain during the anesthetic application, 1 mL of sodium bicarbonate 8.5% solution may be added to 10 mL of 1% lidocaine.[6]
- To decrease excess bleeding during the procedure, epinephrine diluted to 1:100,000 – 200,000 is generally considered safe to use in healthy patients.
- While data is insufficient to suggest increased risk, caution should be used when using epinephrine in patients with peripheral arterial disease.
- The use of epinephrine for digital blocks can be performed but is less often utilized.[7]
Biopsy Instruments
- Tourniquet
- Punch or shave tool
- Nail clippers
- Scalpel
- Tissue scissors
- Needle driver
- Nail elevator[2]
Hemostatic Agents
- Aluminum chloride is the most commonly used hemostatic agent.
- Hyfrecators can be used but carry an increased risk of dystrophy near the nail matrix.
Sterile Gauze
Non-absorbable Suture
Non-stick Wound Dressing and Sterile Petroleum Ointment
- Data suggests that petroleum jelly is just as efficacious in preventing wound infection and promoting wound healing as antibiotic ointments while limiting allergic reactions[8]
Personnel
Nail biopsies are often performed solely by the practitioner. However, some practitioners find that being accompanied by a nurse or medical assistant may increase the efficiency of the procedure by cutting sutures, providing any additional materials that may be needed intraprocedurally, providing hemostasis and setting up the biopsy tray.
Preparation
Before any biopsy or anesthetic application, the biopsy site and the surrounding skin must be cleansed with an antiseptic. Local anesthesia is applied as a nerve block, which can either be a digital block or wing block. After anesthesia application, a 10-15 minute waiting period is sufficient for the full anesthetic effect. During the waiting period, the digit may be placed in a basin of water to soften the nail plate allowing for an easier biopsy. Once ready, a tourniquet is applied to the digit to decrease intraprocedural bleeding. The tourniquet should only be applied for a maximum of 15 minutes to reduce the risk of neurovascular compromise.[9] Many dermatologists err on the side of caution and attempt to apply and remove the tourniquet in under 5 minutes to further reduce risk.
For certain biopsy techniques, the nail must be avulsed before biopsy of the lesion in question. A common technique to avulse the nail is with the use of a nail elevator. The nail elevator is first inserted under the proximal nail fold to gently loosen the nail plate from the overlying nail fold. The elevator is then inserted under the distal nail plate and pushed proximally to detach the nail plate from the nail bed and nail matrix.[9]
Technique or Treatment
The two most common techniques for nail anesthesia consist of the proximal digital block and the distal digital (wing or paronychial) block. The nerves that supply the nail travel along the lateral aspects of the finger. The proximal digital block utilizes this neural anatomy by injecting a local anesthetic in the lateral aspects of the finger base, which creates a field block and requires 10 to 15 minutes to become fully effective. A tourniquet can be placed to decrease blood in the surgical field and to prevent circulatory loss of the anesthetic. Common tools used for the tourniquet include gauze, Penrose drain, foley catheter, and surgical gloves.[3][10][11] The tourniquet should not stay in place for greater than 15 minutes.[12] In the distal digital block, the injection site is found approximately 1 cm proximal and lateral to the angle of the proximal nail fold (PNF) and lateral nail folds (LNFs); this creates a localized block, requiring less anesthetic, and has a quicker effect. The preferred anesthetic is ropivacaine 1% due to its long duration, although any local anesthetic is a viable option.[13]
Nail plate biopsy: This biopsy technique is relatively limited in diagnostic information and is primarily used for fungal culture. It is considered the simplest form of a nail biopsy. A portion of the nail plate is removed with a scissor or nail clipper. In most cases, this biopsy technique does not require anesthesia or hemostatic efforts. However, when a more proximal portion of the nail is required, the nail may be partially avulsed before the biopsy, which requires a digital block and hemostasis. Scarring is rare.
Nail bed biopsy: This is performed to diagnose skin lesions and rashes isolated under the nail plate. To perform a nail bed biopsy, the nail is commonly avulsed. Alternatively, a punch biopsy may be taken directly through the nail plate. After avulsion, the specimen is removed with an excisional biopsy taken longitudinally or via a punch biopsy tool. Biopsies larger than 3 mm in size often require a suture. Onycholysis may occur after the nail has regrown.
Nail fold biopsy: This is performed on the lateral nail folds to diagnose periungual lesions or rashes. The lesion is removed via a shave/punch tool or is excised with a scalpel. A nail elevator tool may be inserted below the surrounding nail fold to assist in easier removal of the lesion while also decreasing the nail matrix's risk of damage. Scarring is rare, and the biopsy site can be left to heal via secondary intention.
Nail matrix biopsy: The nail matrix biopsy is often employed to diagnose or rule out melanoma in patients with longitudinal melanonychia originating from the matrix. The nail may be partially or entirely avulsed, and the lesion is either biopsied via a punch tool or excised with a scalpel. It is important to note that it is best to excise the lesion horizontally rather than longitudinally, unlike nail bed biopsies. The biopsy site is often sutured for better cosmesis and regrowth of the nail. The site may be scarred, and the nail may regrow with a split nail deformity. Staining of the biopsy specimen before send-out can be helpful for orientation and histological interpretation by the pathologist.[2][3]
Longitudinal nail biopsy: The longitudinal nail biopsy is often used for large and laterally located lesions or when a sample of the entire nail unit may be required to diagnose the underlying pathology. One such example is longitudinal melanonychia, which may be a sign of melanoma. With this technique, the nail matrix, bed, fold, and hyponychium are all sampled simultaneously and give the most diagnostic information. To perform the biopsy, an incision is made in-line with the lateral nail fold starting midway between the cuticle and distal interphalangeal joint crease and followed distally to the nail tip. Another incision is placed up to 3 mm medial or lateral to the initial incision within the nail plate to connect each incision's proximal and distal apices. The tissue is then lifted with a skin hook or forceps and removed with tissue scissors to bone depth. The biopsy site is then sutured for optimal healing and cosmesis. This technique is the most invasive nail biopsy technique and has the highest risk for scarring and nail dystrophy.[2][14]
Hemostasis can be obtained via chemical coagulation with aluminum chloride, Monsel’s solution, or less common hyfrecation. A popular technique is holding pressure over the biopsy site. Alternatively, pressure can be applied over the digital arteries after the biopsy is complete. After waiting at least 5 minutes and ensuring there is hemostasis, cleaning and dressing application can commence.[2] The site can be cleaned with alcohol or normal saline and covered in sterile petroleum. The non-stick dressing should be applied.[9]
Complications
Before the procedure, the practitioner should set patient expectations. Potential risks of the procedure include bleeding, infection, permanent nail dystrophy, the possibility that the biopsy does not yield a diagnosis, post-operative pain, and temporary functional handicap of the digit. A strict sterile technique is essential to avoid osteomyelitis because most biopsies are taken down to the periosteum of the underlying phalanx.[5] Complications may include:
- Bleeding
- Postoperative pain
- Infection
- Nail regrowth defects (split nail deformity, erythronychia, dystrophic nail plates)
- Hypersensitivity reaction to lidocaine
- Vasovagal response (due to anesthetic injection)
The patient should receive instruction to elevate the digit for 48 hours post-surgery to prevent edema that can create a tourniquet from the bandage compromising digital perfusion.[3]
Clinical Significance
Nail biopsies are used in conjunction with clinical findings to confirm the diagnosis. The biopsy specimen is processed and histologically evaluated, providing additional information that allows the clinician to make a clinicopathologic diagnosis. With a proper diagnosis, planning and treatment can commence.
Enhancing Healthcare Team Outcomes
The importance of consent, both orally and written, is imperative before any dermatologic procedure. Nail biopsies are of special consideration given the potential complications arising from the disruption of the nail matrix.
Coordination and preparation between healthcare team members provide the opportunity for an optimal procedure outcome. The practicing physician who performs the nail biopsy, the dermatopathologist, processes, and examines the specimen. All of the medical staff who assist are all of great importance to ensure the ultimate goal of the biopsy: diagnosing, treating, and helping patients. [Level V]
Nursing, Allied Health, and Interprofessional Team Interventions
The role of the nurse or medical assistant may vary depending on how the practitioner performs the biopsy. They may help with suturing, provide the physician with additional biopsy materials, set up the biopsy tray or they may help with hemostasis.
Nursing, Allied Health, and Interprofessional Team Monitoring
In addition to monitoring the digit for signs of ischemia, the patient’s comfort should be monitored throughout the procedure. Nail biopsies are precise procedures and even small movements from an uncomfortable patient can decrease the practitioners ability to biopsy the intended area and repair the site for best aesthetic outcomes.
Media
(Click Image to Enlarge)
References
Grover C, Chaturvedi UK, Reddy BS. Role of nail biopsy as a diagnostic tool. Indian journal of dermatology, venereology and leprology. 2012 May-Jun:78(3):290-8. doi: 10.4103/0378-6323.95443. Epub [PubMed PMID: 22565428]
Rich P. Nail biopsy. Indications and methods. The Journal of dermatologic surgery and oncology. 1992 Aug:18(8):673-82 [PubMed PMID: 1307222]
Grover C, Bansal S. Nail Biopsy: A User's Manual. Indian dermatology online journal. 2018 Jan-Feb:9(1):3-15. doi: 10.4103/idoj.IDOJ_268_17. Epub [PubMed PMID: 29441291]
Haneke E. Surgical anatomy of the nail apparatus. Dermatologic clinics. 2006 Jul:24(3):291-6 [PubMed PMID: 16798426]
Fleckman P, Allan C. Surgical anatomy of the nail unit. Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al.]. 2001 Mar:27(3):257-60 [PubMed PMID: 11277893]
McKay W, Morris R, Mushlin P. Sodium bicarbonate attenuates pain on skin infiltration with lidocaine, with or without epinephrine. Anesthesia and analgesia. 1987 Jun:66(6):572-4 [PubMed PMID: 3034106]
Ilicki J. Safety of Epinephrine in Digital Nerve Blocks: A Literature Review. The Journal of emergency medicine. 2015 Nov:49(5):799-809. doi: 10.1016/j.jemermed.2015.05.038. Epub 2015 Aug 4 [PubMed PMID: 26254284]
Draelos ZD, Rizer RL, Trookman NS. A comparison of postprocedural wound care treatments: do antibiotic-based ointments improve outcomes? Journal of the American Academy of Dermatology. 2011 Mar:64(3 Suppl):S23-9. doi: 10.1016/j.jaad.2010.11.010. Epub 2011 Jan 17 [PubMed PMID: 21247662]
Haneke E. Nail surgery. Journal of cutaneous and aesthetic surgery. 2011 Sep:4(3):163-4. doi: 10.4103/0974-2077.91245. Epub [PubMed PMID: 22279379]
McGinness JL, Parlette HL 3rd. Versatile sterile field for nail surgery using a sterile glove. Dermatology online journal. 2005 Dec 1:11(3):10 [PubMed PMID: 16409906]
Grover C, Nanda S, Nagi Reddy BS. Gauze strip tourniquet for nail surgery. Journal of cutaneous and aesthetic surgery. 2014 Jul:7(3):164-6. doi: 10.4103/0974-2077.146673. Epub [PubMed PMID: 25538439]
Rich P. Nail biopsy: indications and methods. Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al.]. 2001 Mar:27(3):229-34 [PubMed PMID: 11277887]
Haneke E. Nail surgery. Clinics in dermatology. 2013 Sep-Oct:31(5):516-25. doi: 10.1016/j.clindermatol.2013.06.012. Epub [PubMed PMID: 24079580]
de Berker DA. Lateral longitudinal nail biopsy. The Australasian journal of dermatology. 2001 May:42(2):142-4 [PubMed PMID: 11309042]