Percutaneous Transluminal Coronary Arteriography
Percutaneous Transluminal Coronary Arteriography
Introduction
Percutaneous transluminal coronary arteriography or invasive coronary angiogram is considered the goal standard investigation tool to diagnose coronary artery disease. Coronary disease is the leading cause of death in the United States of America. Around 20.1 million adults have coronary disease in the United States.[1] Over a million coronary angiograms are performed annually in the USA. Dr. Sones performed the first coronary angiogram in 1958.[2] The Interventional Cardiology field has evolved significantly since then. The fundamental goal of a coronary angiogram is to define the coronary anatomy and determine the severity of the stenosis in epicardial coronary arteries or coronary artery bypass grafts.
A coronary angiogram is relatively safe and carries prognostic value.[3] However, complications like pain, bleeding, radiation-associated injury, acute kidney injury, major heart attack, stroke, blood transfusions, access site infection, and symptoms from athero-embolism, arrhythmias, and death can occur. In general, most interventional cardiologists agree that hemodynamically significant coronary disease occurs if the angiographically estimated severity of the stenosis is more than 70% (see Graph. The Effect of Coronary Artery Stenosis on Coronary Flow Reserve). If the stenosis is between 50-70%, it is recommended to evaluate the lesion with physiological assessment, intravascular ultrasound (IVUS), or optical coherence tomography (OCT).[4] It will guide interventional cardiologists in determining the stenosis's severity and revascularization options.
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
Anatomy
The left main coronary artery arises from the left coronary sinus of the aorta and divides into a left anterior descending artery (LAD)and left circumflex artery (LCx). The left anterior descending artery gives off-diagonal branches, which supply arterial blood to the anterolateral myocardium, and anterior septal branches, which supply blood to the anterior interventricular septum and anterolateral papillary muscles. The terminal part of the LAD provides the left ventricular apex. The left circumflex artery divides into obtuse marginal branches. It supplies blood to the posterolateral side of the left ventricle (see Image. Left Coronary Angiogram, Various Orthogonal Views). [5]
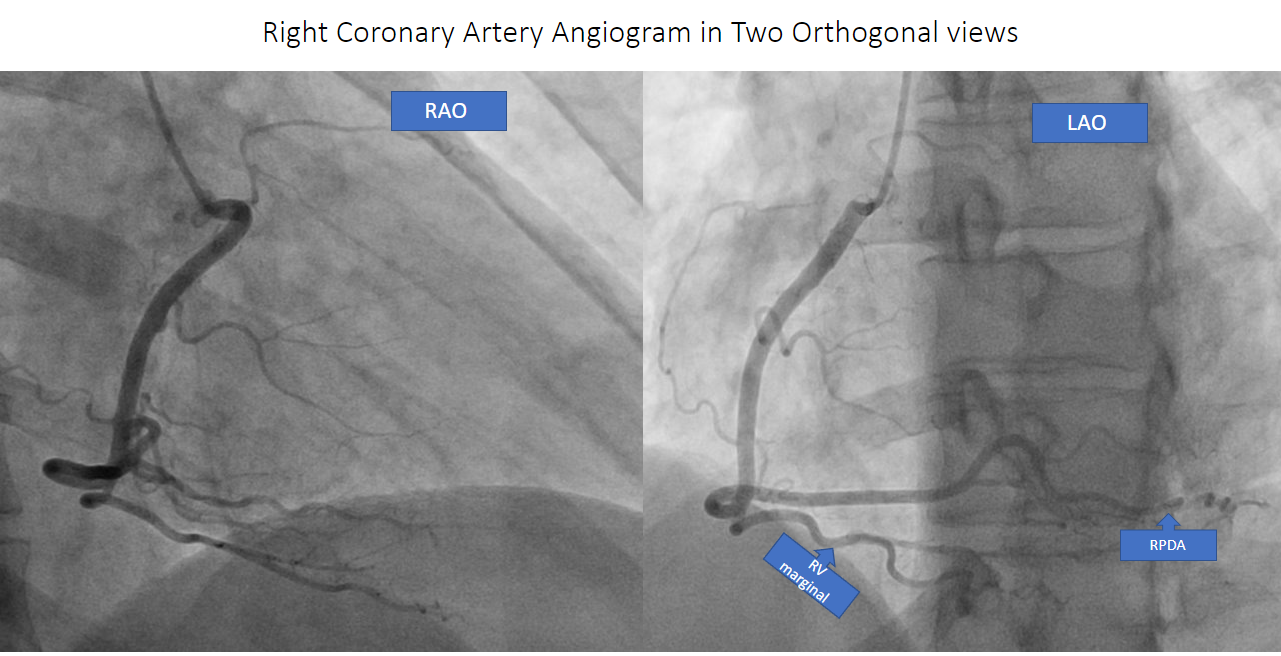
The right coronary artery originates from the right coronary sinus of the aorta. It travels along the right atrioventricular groove and divides into the posterolateral branch and posterior descending artery. It also gives off the sinoatrial nodal artery and right ventricular marginal artery. The dominance of coronary circulation depends on the posterior descending artery. The right dominant circulation is widespread because, 80-85%of the time, PDA comes from the right coronary artery (see Image. Right Coronary Angiogram, Two Orthogonal Views).[5]
Anomalous coronary arteries are relatively rare ( 1-2%). Among them, Anomalous circumflex arteries coming off the right coronary sinus or right coronary artery are common. It is considered a benign clinical course. Very rarely, anomalous coronary arteries traverse between the aorta and pulmonary artery, which can be associated with a malignant clinical course.[5]
Physiology
Epicardial coronary arteries (>400 micrometers) divide into small arteries (<400 micrometers)and eventually arterioles (<100 micrometers) which further divide into capillaries(<10 micrometers). Coronary blood flow is predominant during diastole compared to systole—the epicardial coronary artery transport blood to smaller arteries. Smaller arteries and arterioles control the coronary vascular blood flow by autoregulation. Small arteries, Arterioles, and capillaries determine the index of microcirculatory resistance. Coronary flow reserve (CFR) depends on blood transport, autoregulation, and metabolite exchange at the capillary level (see Graph. Coronary Macro and Microcirculation). Physiological assessment of epicardial coronary stenosis measured by fractional flow reserve (FFR) and microvascular resistance measured by the index of microcirculatory resistance. Instantaneous wave-free ratio (IFR) can be used in place of fractional flow reserve.[6]
Indications
Coronary angiogram's common indications:
- Stable angina(Canadian cardiology society class II, III, or IV) on maximally tolerated antianginal therapy (preferable > two different classes of antianginals).
- Unstable angina.
- Non-ST-elevation MI.
- High-risk noninvasive testing (more than 3% annual MI or death).
- Stress ischemia involves more than 10% of the myocardium or more than two coronary territories.
- Stress-induced left ventricular(LV) dysfunction (Ejection fraction less than 45% or >10% drop from the baseline).
- ST depressions more than 2 mm at low workload or persisting into recovery.
- Coronary artery calcium scores more than 400 Agaston.
- Stress-induced LV dilatation.
- Inducible wall motion abnormalities in more than two coronary artery territories.
- Inducible wall motion abnormality at low-dose dobutamine or low heart rate.
- Left-main more than 50% or multivessel disease with more than 70% stenosis.
- Exercise-induced ventricular tachycardia, ventricular fibrillation, or ST elevations.
- Successful resuscitation of sudden cardiac death ( if favorable resuscitation features are present).
- Sustained ventricular tachycardia with no clear etiology.
- Chest pain syndrome with unclear etiology and equivocal noninvasive test.
- ST-elevation MI.[7][8]
- Acute coronary syndrome with mechanical complications like mitral regurgitation and ventricular septal defect.Cardiac shock with hemodynamic instability (In selective cases).
- Before surgical intervention when symptomatic valvular heart disease or pericardial disease is suspected.
- Before surgical intervention to ascending aorta with coronary artery involvement.
- Preoperative and post-surgical evaluation for symptomatic cardiac transplant patients.
- Suspicion for symptomatic congenital coronary anomalies.
Contraindications
Absolute Contraindication
- Extremely limited life expectancy with no clinical benefit from coronary revascularization.
Relative Contraindications (Applicable for non-emergent coronary angiograms)
- Acute on chronic kidney injury; end-stage renal disease.
- Active bleeding; severe anemia with unknown etiology.
- Severe hemorrhagic disorder. Platelets less than 50,000.
- Recent direct oral anticoagulants (DOACs) or Coumadin use.
- Recent thrombotic or hemorrhagic stroke. [8][9]
- Severe sepsis and septic shock; Untreated bacteremia.
- Altered mental status/ Unable to follow commands.
- Acute pulmonary edema.
- A patient who refused pre-treatment for contrast allergy.
- Status post cardiac arrest with unfavorable resuscitation features present ( PH <7.2, elevated lactate >7, age more than 85, ESRD,> 30 min to ROSC, no bystander CPR, unwitnessed cardiac arrest).
Equipment
- Micro (25G) or macro (18G) puncture needles can be used for arterial access.
-
Vascular ultrasound for common femoral and radial artery vascular access is highly recommended.
-
Low osmolar contrast agents (Iohexol and Iopamidol) and Iso-osmolar contrast agents (Iodixanol) are associated with lower contrast-induced nephropathy.
- Standard miscellaneous inventory for both femoral and radial approach: Band bag, 36 x 40 in., with tape; Bowl, guidewire, 2500cc; Bowl, sponge, 32oz., 1000cc; Clamps, towel, 41/2 in., plastic, blue, curved; Cover, setup, 54 x 90. drape, femoral angiography, 80 x 135 in. Forceps, Halstead mosquito, five in., curved. Gowns, X-Large. Labels, a sheet of 22 waterproofs. Marker, skin, dual-tip Medicine cup, two oz., 60 ccs, graduated. Needle holder, nest, foam block. Needle, 18G x 11/2 in. Needle, 25G x 11/2 in. Scalpel, #11, safety. Sponges, 4 x 4 in., 4-ply. Syringe, control, luer lock, 10mL.Syringes, luer lock, 10mL.Syringes, luer lock, 20mL. Table cover, 50 x 90 in. Towels, absorbent, white. Towels, OR, blue. Manifold. Pressure bag. Pressure transducer.
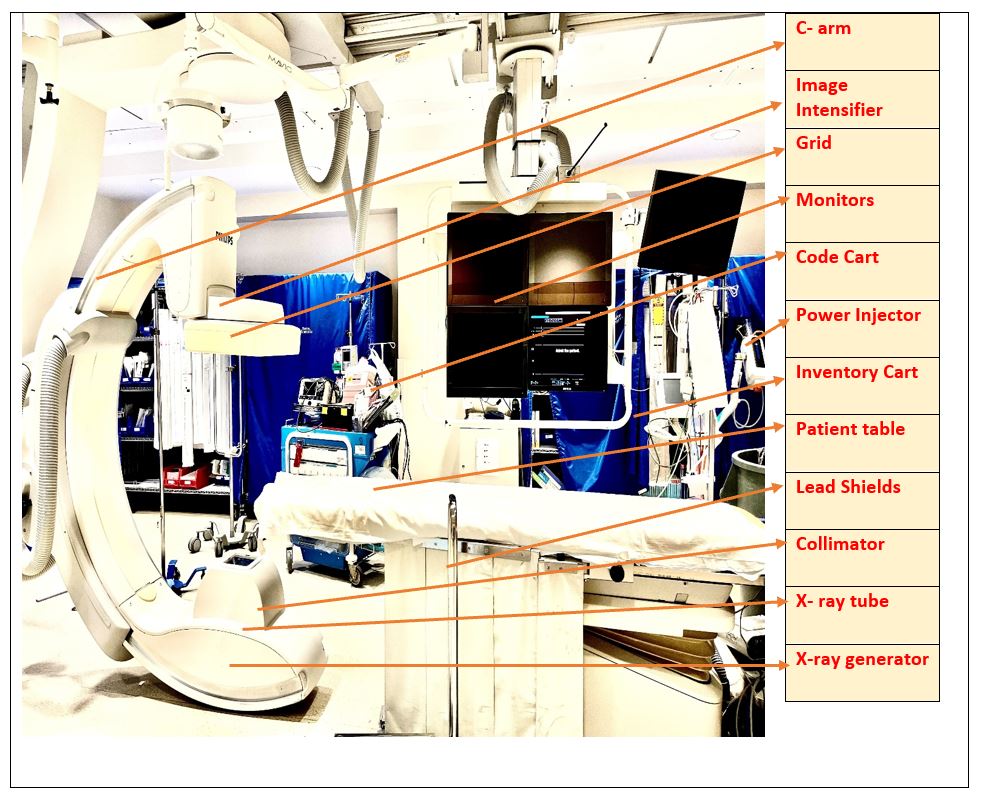
- Fluoroscopy is common for femoral and radial approaches (see Image. Cardiac Catheterization Lab).
| Medications | Access Sheaths | Diagnostic catheters | Wires | Guide catheters | Closure device | |
| Femoral Approach |
|
|
Various preshaped diagnostic catheters are available based on the manufacturing company. Available in 4 Fr, 5 Fr, 6 Fr, and 7 Fr diameters, short or long.Examples:
|
0.35" preshaped supporting wire ( hydrophilic on Hydrophobic) ( short (175- 190cm) or long (270-400cm)
Examples:
|
Various preshaped braided guiding catheters are available based on manufacturing companies. Available in 5 Fr, 6 Fr, 7 Fr, and 8 Fr diameters, short or long.
Examples:
|
Commonly used:
|
| Radial, Ulnar, and Brachial Approach |
|
|
As mentioned above, some dedicated radial catheters like
|
As mentioned above. Preferably long wires. |
As mentioned above, some dedicated radial guide catheters like
|
TR Band. |
Personnel
The cardiac catheterization laboratory team should include:
- Cath lab medical director
- Cath lab nurse manager
- Interventional /Invasive cardiologist
- Cath lab nurse
- Cath lab technician
- Janitor
- Chaplain
- Pharmacist
- Echo technician
- Transporter
Preparation
Step 1
The Cath lab charge nurse or scheduler will contact the patient regarding preoperative instructions.
- Nothing by mouth for 6-8 hours.
- Not to take anticoagulants.
- Discuss patient transportation options before and after the procedure.
- Review of home medications with a patient.
- Review of patient allergies.
- Review of the patient's labs, chest x-ray, urinalysis, and other preoperative testing.
- Review of the indication for a coronary angiogram with the patient.
- Expected time of the procedure.
- Expected time to check in at the Cath lab.
Step 2
- The Cath lab nurse will accompany the patient from the check-in counter to the Cath lab.
- Safely lock the patient's items. The patient wears a surgical gown.
- The nurse records the patient's vital signs (heart rate, blood pressure, temperature, and respiratory rate).
- Insertion of IV access, preferably one on both arms.
- Connect the patient to telemetry and blood pressure monitor.
- Obtain Baseline EKG.
- Review of all the blood work and preoperative testing with the patient.
- Brief physical examination.
- IV hydration will be started based on the patient's clinical condition ( Normal saline is preferable to N acetylcysteine and bicarbonate solution).
Step 3
- Interventional/Invasive cardiologist explains the procedure limitations and benefits in detail to the patient and obtains written consent.
Step 4
- Brief physical examination by the physician. Modified Barbeau test for radial access. Routine groin check for femoral access. The physician finalizes the access route and the preferred catheters.
Step 5
- Cath lab technician connects pressure transducers and flushes all the diagnostic catheters. They will prepare the inventory based on the physician's preference.
Step 6
- The patient will be supine on the Cath lab table and covered under a sterile drape. The patient's groin or wrist will be prepped and sterilized for the procedure. The Cath lab technician organizes the inventory table and also helps with rotating C-arm.
Step 7
- The Cath lab nurse will organize medications like lidocaine and moderate sedation and help prep vascular ultrasound.
Step 8
- Cath lab technician or nurse will do a Pre-procedure time-out.
Step 9
- The second technician or nurse will be ready to enter all the hemodynamic data in the Cath lab reading room.
Technique or Treatment
The patient will receive moderate sedation and local anesthesia before arterial access.
Arterial Access
- Common femoral artery access:
- Under fluoroscopic and ultrasound guidance, obtain common femoral artery access with an 18 G large or 25 guide arch needle.
- Once blood flow pulsatility conformed, advance 0.35 in J-wire or 0.14 in microwire through the needle into the common femoral artery and iliac arteries under fluoroscopy guidance. Remove the needle
- Introduce 5 French or 6 French access sheaths over the wire into the common femoral artery in a retrograde fashion. Connect the access sheath side port to the IV pressure flush line.
- Inject 50: 50 through the side port into the sheet and perform a femoral artery angiogram.
- Flush the sheath frequently
- Radial or Ulnar artery access:
- Under ultrasound guidance, obtain radial /ulnar artery access with 25 gueuze microneedle.
- Once blood flow Pulsatility conformed, advance 0.14 in microwire through the needle into the radial/ulnar artery and remove the needle.
- Introducing 5 French or 6 French access sheath over the wire into the radial/ulnar artery in a retrograde fashion. Connect the access sheath side port to the IV pressure flush line.
- Inject radial cocktail ( nitroglycerin, nicardipine, or verapamil) and IV heparin through the side port.
- Flush the sheath frequently.
Left main coronary artery cannulation:
- Advance diagnostic catheters ( JL, AL, Jacky, or Tiger) over the wire under fluoroscopy guidance. Once a catheter tip is in the left coronary sinus, remove 0.35 in support wire. Obtain aortic pressure and waveform for baseline measurements. Engage the left main coronary artery with a slow, steady clock, counter clock, and push and pull maneuver. Left anterior oblique view preferred to engage the left main coronary artery. Obtain angiogram pictures by injecting IV contrast into the left main with steady pressure. It is crucial to review pressure tracing an EKG before the injection. Avoid injecting contrast if pressure is dampened. Obtain angiogram pictures in the right anterior oblique caudal, right anterior oblique cranial, left anterior oblique cranial, and left anterior oblique caudal. Exchange the catheter over the wire under fluoroscopic guidance. (Media Item 2)
Right coronary artery cannulation:
- Advance diagnostic catheters (JR, AR, Jacky, or Tiger) over the wire under fluoroscopy guidance. Once a catheter tip is in the right coronary sinus, remove 0.35 in support wire. Obtain aortic pressure and waveform for baseline measurements. Engage the right coronary artery with slow and steady clock, counter clock, and push and pull movements. Left anterior oblique view preferred to engage the right coronary artery. Obtain angiogram pictures by injecting IV contrast into the right coronary artery with steady pressure. It is vital to review pressure tracing and EKG before the injection. Avoid injecting contrast if the pressure is dampened. Obtain angiogram pictures in the right anterior oblique, left anterior oblique, and left anterior oblique cranial views. Exchange the catheter over the wire under fluoroscopic guidance. (Media Item 3)
Saphenous venous bypass graft (SVG) cannulation:
- Advance diagnostic catheters over the wire under fluoroscopy guidance. Preferably JR, AR, and AL catheters are for SVG to left-sided grafts and multipurpose catheters for SVG to RCA grafts. Once a catheter tip is in the SVG ostium or near the radiopaque marker, remove 0.35 in support wire. Obtain aortic pressure and waveform for baseline measurements. Engage SVG with slow and steady clock, counter clock, and push and pull movements. The right anterior oblique view is preferred to engage left-sided SVG grafts, and the Left anterior oblique is preferred to engage right-sided grafts. Obtain angiogram pictures by injecting IV contrast into the SVG with steady pressure. It is crucial to review pressure tracing an EKG before the injection. Avoid injecting contrast if the pressure is dampened. Obtain angiogram pictures in the right anterior oblique, left anterior oblique, and left anterior oblique cranial or caudal views. Exchange the catheter over the wire under fluoroscopic guidance.
Internal mammary artery (IMA) cannulation:
- Advance diagnostic catheters ( AR or IMA catheters) over the wire under fluoroscopy guidance. Once a catheter tip is in the IMA ostium, remove 0.35 in support wire. Obtain aortic pressure and waveform for baseline measurements. Engage IMA with slow and steady clock, counter clock, and push and pull movements. Anteroposterior or Right anterior oblique view is preferred to engage LIMA and Left anterior oblique is preferred to engage RIMA. Obtain angiogram pictures by injecting IV contrast into the IMA with steady pressure. It is essential to review pressure tracing an EKG before the injection. Avoid injecting contrast if the pressure is dampened. Obtain angiogram pictures in right anterior oblique cranial and left anterior oblique cranial views. Exchange the catheter over the wire under fluoroscopic guidance. Left radial access is preferred if the left internal mammary artery is present. Before engaging the internal mammary artery, one should engage the subclavian artery in the femoral access approach.
Post-angiogram steps:
- Review angiogram pictures once it is completed.
- Remove catheters over the wire under fluoroscopic guidance.
- Consider a closure device if the access site is optimal at the common femoral artery.
- Apply TR band for radial or ulnar access site.
- Transfer the patient to the postprocedure recovery area.
- Watch for blood pressure, oxygen saturation, and rhythm changes carefully.
- Once the patient recovers from sedation and vital signs are within normal limits, consider discharging the patient if inpatient care is unnecessary.
- Discussed the angiogram results with the patient and family in detail.
- Arrange outpatient follow-up.
- Review the medications before discharge.
Complications
Early Complications
- Access site hematoma.
- Acute Kidney Injury.
- Stroke ( Embolic or Hemorrhagic).
- Thromboembolic events.
- Acute blood anemia requiring blood transfusion.
- Access site pain.
- Myocardial infarction (Abrupt closure of coronary artery).
- Acute pulmonary edema.
- Emergency Coronary artery bypass surgery.
- VT/Vfib.
- Atheroemboli.
- Radiation-related injuries.[8][9]
- A-V fistula.
- Pseudoaneurysm.
- Death
Delayed Complications
- Access site infection.
- Acute Kidney Injury.
- Access site hematoma.
- Radiation-related injuries ( It is common in obese patients, prolonged procedure time, etc.)
- Acute on chronic pulmonary edema.
- Death
Clinical Significance
A coronary angiogram defines the coronary anatomy and determines the severity of the stenosis of coronary arteries. It would help interventional/invasive cardiologists to plan for appropriate revascularization strategy if indicated. Tools and techniques for coronary angiograms significantly evolved in the last two decades, and complication rates decreased significantly. A coronary angiogram is relatively safe and can be performed in a daycare setting. However, it is not entirely free of complications.
Enhancing Healthcare Team Outcomes
A coronary angiogram is a minimally invasive procedure and can be associated with severe complications. The heart team approach is essential to perform coronary angiograms effectively with minimal complications. The heart team approach consists of an interventional/invasive cardiologist, general cardiologist, cath lab nurse, cath lab technician, cardiothoracic surgeon, primary care physician, or referral physician. Close-loop communication between the heart team members can minimize unwanted complications. Meticulous patient selection is essential for coronary angiograms in stable angina patients. Always review the patient's allergies, home medications, renal function tests, hemoglobin and hematocrit, platelets, and PT INR before the procedure to avoid common complications. IV hydration prevents contrast-induced nephropathy. It is vital to watch for pressure tracing and rhythm strips before injecting contrast into the coronary artery ostium. Effective team communication is the key to better cath lab procedure outcomes.[8]
Nursing, Allied Health, and Interprofessional Team Interventions
The cath lab charge nurse or scheduler, or allied health care team member will contact the patient regarding preoperative instructions:
- Nothing by mouth for 6-8 hours.
- Not to take anticoagulants.
- Patient transportation options before and after the procedure.
- Review the home medications with a patient.
- Review of patient allergies.
- Review of the patient's labs, chest x-ray, urinalysis, and other preoperative testing.
- Review of the indication for a coronary angiogram with the patient.
- Expected time of the procedure.
- Expected time to check-in at the cath lab.
On the day of the procedure:
- The cath lab nurse or Allied health care member will accompany the patient from the check-in counter to the cath lab.
- Safely lock the patient's items. Help the patient wears a surgical gown.
- Insertion of IV access, preferably one on both arms.
- Connect the patient to telemetry and blood pressure monitor.
- Obtain Baseline EKG.
- Review of all the blood work and preoperative testing with the patient.
- Brief physical examination.
- IV hydration based on the patient's clinical condition (Normal saline is preferable to N acetylcysteine and bicarbonate solution).
- Coordinate care and update it to the patient and the patient's family.
- Administering medications during the procedure.
Nursing, Allied Health, and Interprofessional Team Monitoring
- Before the procedure, the nurse obtains and monitors the patient's vital signs (heart rate, blood pressure, temperature, and respiratory rate).
- Reporting proceduralist if any pressure wave form dampening, blood pressure changes, or EKG rhythm changes.
Media
(Click Image to Enlarge)
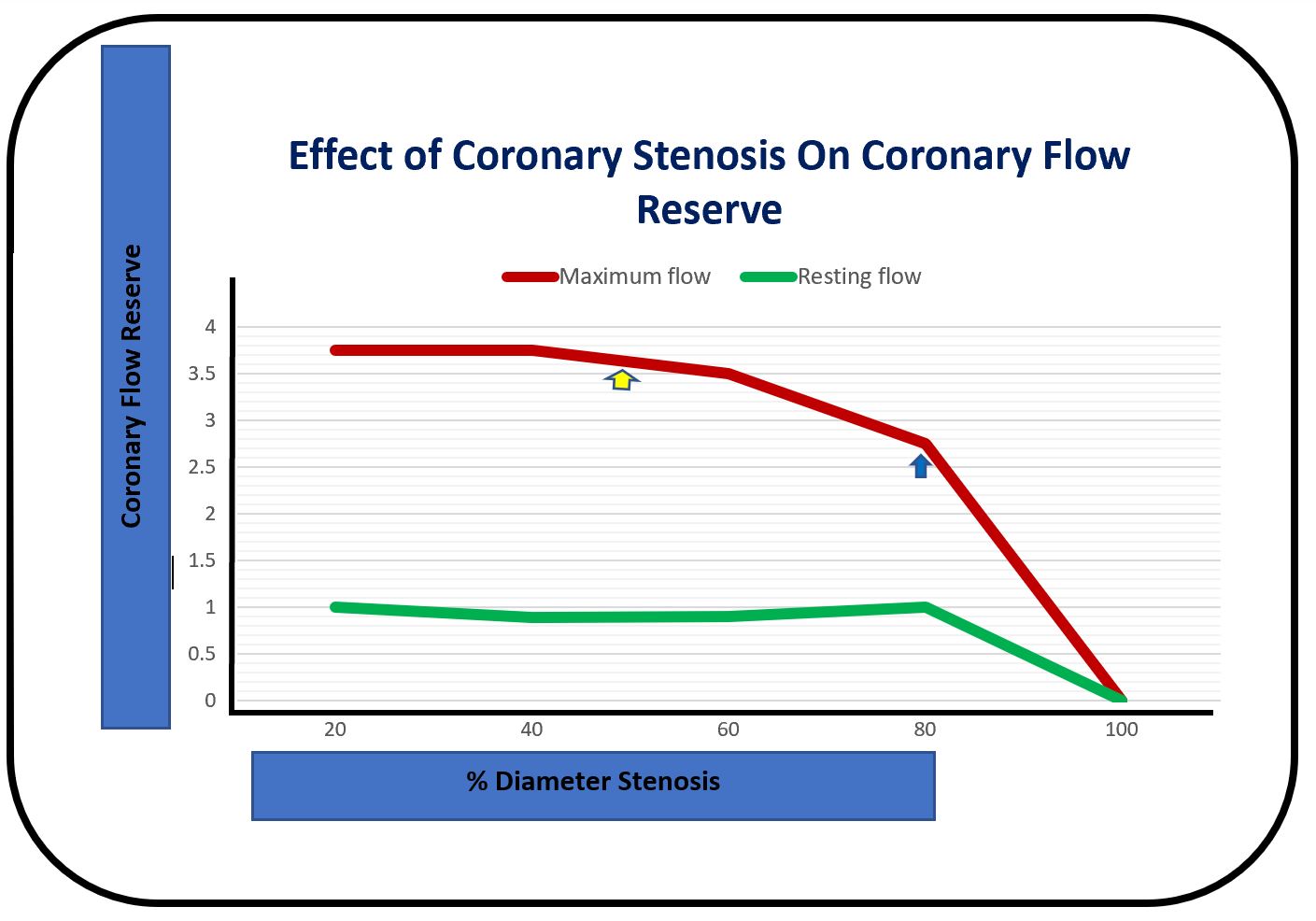
The Effect of Coronary Artery Stenosis on Coronary Flow Reserve. The maximal hyperemic coronary flow will start declining once coronary artery stenosis reaches approximately 50%, and resting coronary flow remains unchanged. However, resting coronary flow declines once coronary stenosis reaches 70% to 80%.
Contributed and adapted by G Maheswara, MD. Modified from Gould et al. 1974.
(Click Image to Enlarge)
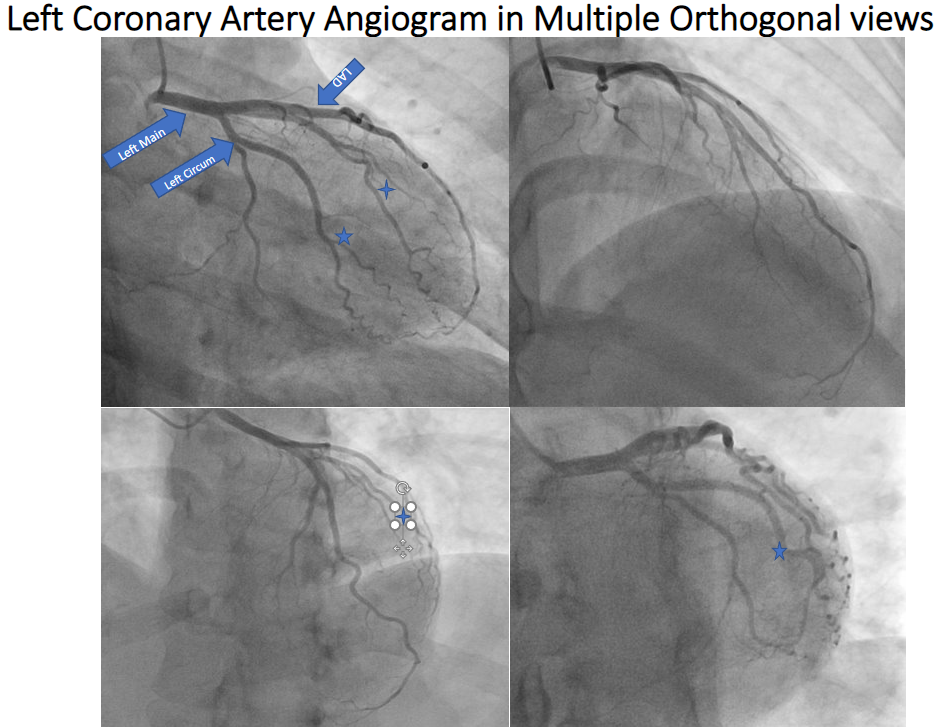
Left Coronary Angiogram, Various Orthogonal Views. The angiogram showed the left main coronary artery bifurcating into a left circumflex artery and a left anterior descending artery. Left top, right anterior oblique caudal view. Right top, right anterior oblique cranial view. Left bottom, left anterior oblique cranial view. Right bottom, left anterior oblique caudal view. Blue star: Obtuse marginal branches of left circumflex; two-spike star, diagonal branches of LAD.
Contributed by G Maheswara, MD
(Click Image to Enlarge)
(Click Image to Enlarge)
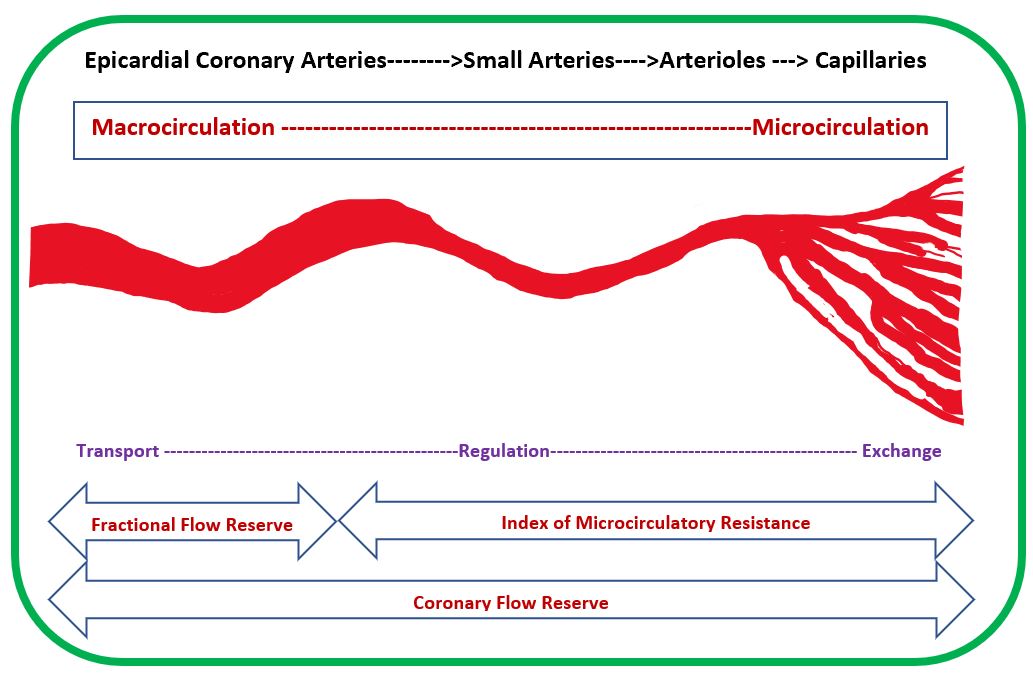
Coronary Macro and Microcirculation. The epicardial coronary artery transports blood to smaller arteries. Smaller arteries and arterioles control blood flow by autoregulation. Small arteries, arterioles, and capillaries determine the index of microcirculatory resistance (IMR). Coronary flow reserve depends on blood transport, autoregulation, and exchange of blood at the capillary level.
Contributed and adapted by G Maheswara, MD. Modified from Pijls N, et al.
(Click Image to Enlarge)
References
Wilson PW, Culleton BF. Epidemiology of cardiovascular disease in the United States. American journal of kidney diseases : the official journal of the National Kidney Foundation. 1998 Nov:32(5 Suppl 3):S56-65 [PubMed PMID: 9820465]
Ryan TJ. The coronary angiogram and its seminal contributions to cardiovascular medicine over five decades. Transactions of the American Clinical and Climatological Association. 2002:113():261-71 [PubMed PMID: 12053714]
Rao Golla MS, Paul T, Rao S, Wiesen C, Yeung M, Stouffer GA. Risk of developing coronary artery disease following a normal coronary angiogram in middle-aged adults. The Journal of invasive cardiology. 2014 Dec:26(12):624-8 [PubMed PMID: 25480990]
Sharma SK, Vengrenyuk Y, Kini AS. IVUS, OCT, and Coronary Artery Calcification: Is There a Bone of Contention? JACC. Cardiovascular imaging. 2017 Aug:10(8):880-882. doi: 10.1016/j.jcmg.2017.06.008. Epub [PubMed PMID: 28797409]
Mori S, Tretter JT, Spicer DE, Bolender DL, Anderson RH. What is the real cardiac anatomy? Clinical anatomy (New York, N.Y.). 2019 Apr:32(3):288-309. doi: 10.1002/ca.23340. Epub 2019 Feb 13 [PubMed PMID: 30675928]
Del Buono MG, Montone RA, Camilli M, Carbone S, Narula J, Lavie CJ, Niccoli G, Crea F. Coronary Microvascular Dysfunction Across the Spectrum of Cardiovascular Diseases: JACC State-of-the-Art Review. Journal of the American College of Cardiology. 2021 Sep 28:78(13):1352-1371. doi: 10.1016/j.jacc.2021.07.042. Epub [PubMed PMID: 34556322]
Ryan TJ, Antman EM, Brooks NH, Califf RM, Hillis LD, Hiratzka LF, Rapaport E, Riegel B, Russell RO, Smith EE 3rd, Weaver WD, Gibbons RJ, Alpert JS, Eagle KA, Gardner TJ, Garson A Jr, Gregoratos G, Smith SC Jr. 1999 update: ACC/AHA Guidelines for the Management of Patients With Acute Myocardial Infarction: Executive Summary and Recommendations: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Acute Myocardial Infarction). Circulation. 1999 Aug 31:100(9):1016-30 [PubMed PMID: 10468535]
Level 1 (high-level) evidenceWriting Committee Members, Lawton JS, Tamis-Holland JE, Bangalore S, Bates ER, Beckie TM, Bischoff JM, Bittl JA, Cohen MG, DiMaio JM, Don CW, Fremes SE, Gaudino MF, Goldberger ZD, Grant MC, Jaswal JB, Kurlansky PA, Mehran R, Metkus TS Jr, Nnacheta LC, Rao SV, Sellke FW, Sharma G, Yong CM, Zwischenberger BA. 2021 ACC/AHA/SCAI Guideline for Coronary Artery Revascularization: Executive Summary: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Journal of the American College of Cardiology. 2022 Jan 18:79(2):197-215. doi: 10.1016/j.jacc.2021.09.005. Epub 2021 Dec 9 [PubMed PMID: 34895951]
Level 1 (high-level) evidenceScanlon PJ, Faxon DP, Audet AM, Carabello B, Dehmer GJ, Eagle KA, Legako RD, Leon DF, Murray JA, Nissen SE, Pepine CJ, Watson RM, Ritchie JL, Gibbons RJ, Cheitlin MD, Gardner TJ, Garson A Jr, Russell RO Jr, Ryan TJ, Smith SC Jr. ACC/AHA guidelines for coronary angiography: executive summary and recommendations. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Coronary Angiography) developed in collaboration with the Society for Cardiac Angiography and Interventions. Circulation. 1999 May 4:99(17):2345-57 [PubMed PMID: 10226103]
Level 1 (high-level) evidence