Introduction
Conscious sedation is a technique whereby patients undergo a drug-induced depression of their consciousness but retain the ability to self-ventilate, maintain protective reflexes, and respond to verbal or light-pressure stimuli. It is a valuable tool often used in dentistry due to its anxiolytic effects. It makes treatment accessible to nervous patients or those with medical requirements, increasing their cooperation and enabling the practitioner to complete complex treatment without rendering the patient unconscious. Conversely, a general anesthetic is where the patient is unconscious and unresponsive. Respiratory support is, therefore, essential to maintain the airway.[1]
Local anesthetic (LA) controls loco-regional pain but does not affect consciousness. Conscious sedation is anxiolytic but does provide adequate analgesia, so LA must also be used.[2]
Benzodiazepines, nitrous oxide gas, opioids, ketamine, and propofol are drugs used to provide conscious sedation. Their routes of administration include intravenous, intranasal, oral, and inhalation.[3] Common combinations utilized by dentists are:
- Inhalation sedation using nitrous oxide/oxygen
- Oral sedation using diazepam
- Single-drug intravenous sedation using midazolam
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
Nitrous oxide is a colorless gas with a rapid onset and a wide safety margin. Many describe it as odorless or sweet swelling. As the technique suggests, it is inhaled and distributed from the lungs into the bloodstream via diffusion through the alveoli. It is removed from the system rapidly as levels are diminished during expiration.[4]
Unlike many drugs used in conscious sedation, nitrous oxide gives a slight analgesic effect and is both anxiolytic and analgesic. There are several theories as to why this is the case. Regarding analgesia, the most accepted is that the gas stimulates the release of enkephalins, which bind to opioid receptors, stimulating noradrenergic routes. For anxiolysis, nitrous oxide is suggested to utilize the benzodiazepine binding site to trigger the GABA (gamma-aminobutyric acid) receptor.[5]
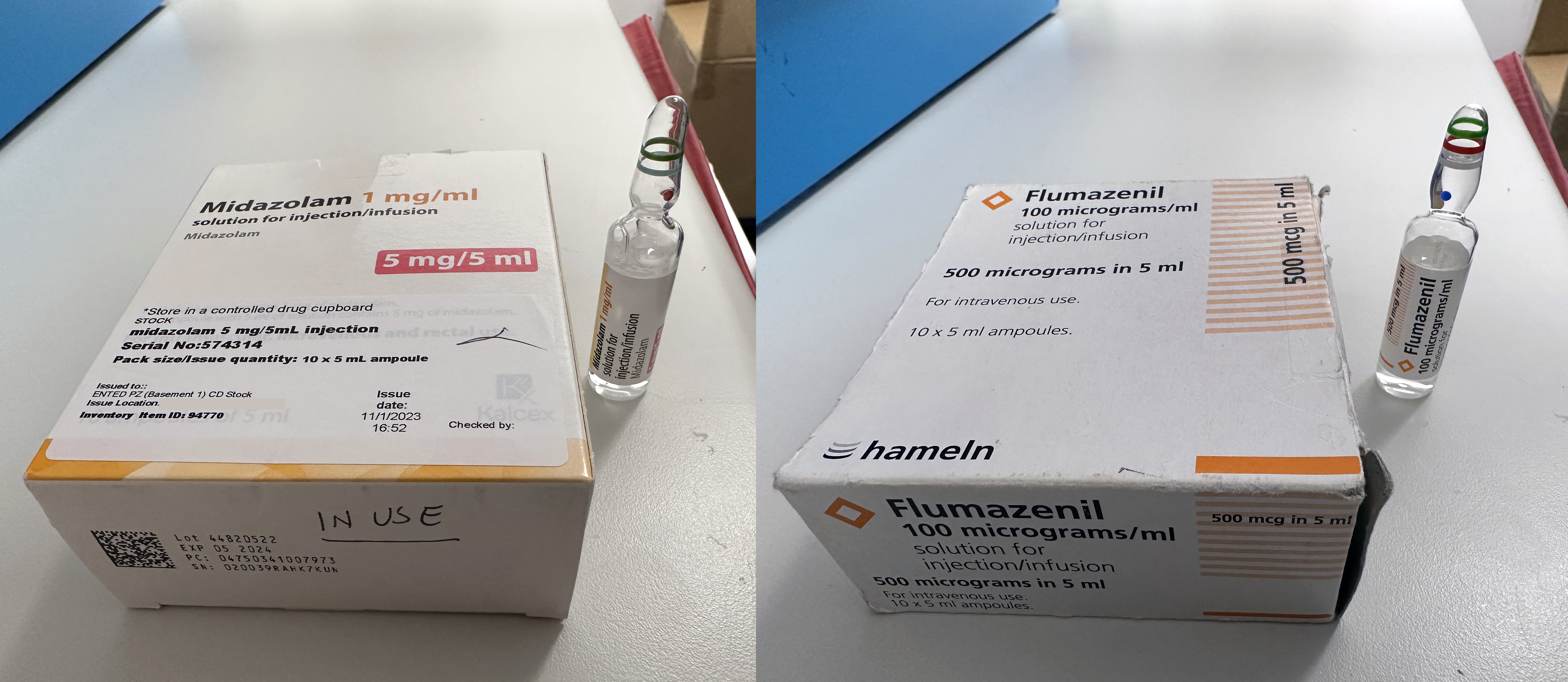
Benzodiazepines are a group of drugs with many uses within the medical field. They can treat insomnia, alcohol withdrawal, anxiety, and seizures and are used as sedative agents by dentists and in critical care or end-of-life units.[6] Benzodiazepines bind to and activate GABA receptors, suppressing the central nervous system and resulting in a sedative effect. The anxiolytic and anticonvulsant properties are also attributed to this mechanism of action. Midazolam is the most used for intravenous sedation; it has a rapid onset of action with a duration of approximately 1 to 2 hours and is relatively safe when used appropriately. It is important to note that it causes anterograde amnesia.
Diazepam has an onset of between 15 to 60 minutes when given orally. This, coupled with its anxiolytic properties, means it can be a useful drug to give patients in the hours before a procedure, reducing their apprehension and increasing the likelihood of them attending or proceeding with their appointment.[7]
Benzodiazepines are widely regarded as safe to use. Firstly, this is due to the high toxic-to-therapeutic ratio. Secondly, one of the significant benefits is that they have a reversal agent, flumazenil, that can counter or reverse their pharmacological effects and is therefore indicated for use in over-sedation or respiratory depression.[8]
Flumazenil acts as a competitive antagonist of benzodiazepines due to its high affinity to the GABA receptor binding site, displacing the benzodiazepine and subsequently reversing the drug's sedative effects.[9] It is given intravenously and has an onset of 1 to 2 minutes. Flumazenil has a shorter duration of action than midazolam, so the patient must be monitored closely for up to 2 hours due to the potential for re-sedation. Certain practitioners use flumazenil to promote quick recovery and more efficient discharge; however, this practice is not broadly accepted or recommended.[8]
Indications
Dental anxiety is the most common reason patients opt for or undergo conscious sedation. This sedation can also be used to provide safe treatment for those with medical conditions exacerbated by stress, such as epilepsy or hypertension. Treatment for patients who suffer from conditions causing dyskinesia, such as Parkinson disease, can be challenging for both the operator and the patient. Sedation can be an effective way of controlling involuntary movements. Further indications are increased surgical complexity and the age of the patient.[10]
Contraindications
Absolute contraindications include pregnancy, allergy, or drug interaction. A cautious approach should be adopted when sedating patients taking psychotropics due to the synergist effect resulting in deeper sedation. Several patient groups require special consideration due to the increased risk of complications: those with significant systemic illnesses, e.g., chronic obstructive pulmonary disease, multiple co-morbidities, or conditions that cause upper airway obstruction. Common medical problems resulting in this obstruction are obesity and sleep apnea.[11] With a patient presenting like this, one can request a pre-assessment by an anesthesiologist, who can also perform the sedation in a general hospital.
Inhalational sedation should be avoided in patients with upper respiratory tract infections, chronic obstructive pulmonary disease, and recent middle ear surgery or current infection.[4][10] History of illicit drug use can impact the efficacy of conscious sedation.[12] If a patient is not fit for conscious sedation, local anesthetic or general anesthetic should be explored further. The decision will be based on patient anxiety, age, and complexity of treatment.
Equipment
Several factors should be checked and available before any procedure.[13][14] These include the following:
- Monitoring equipment, eg, pulse oximeter and blood pressure cuff
- Intravenous cannulas or masks to deliver nitrous oxygen/oxygen
- Suction tubing
- Oxygen delivering equipment
- Stocked medical emergency trolley
- Access to automated external defibrillators
- Reversal drugs
Personnel
The correct number of sedation-trained healthcare professionals must be acquired before starting treatment. Typically, this is the dental surgeon and one dental nurse. This allows the dentist and their dental assistant to focus on the therapy while the remaining sedation nurse monitors the patient. These team members will have completed further training providing them with an additional qualification. They should also be trained in basic and immediate life support, eg, managing medical emergencies or using airway adjuncts.[14]
Preparation
Patient Selection
A thorough history, clinical examination, and pre-assessment are imperative to ensure appropriate patient selection. This combination evaluates whether patients are medically or psychologically suitable for a specific technique and determines the appropriate procedure. This is fundamental for patient safety but can also benefit the clinician, as procedures will be more challenging without adequate patient cooperation.[15]
A pre-assessment should record the patient's baseline vital signs, such as oxygen saturation, blood pressure, heart rate, height, and weight. The latter allows a body mass index score to be calculated.[16]
The American Society of Anesthesiologists (ASA) classification of the physical status of a patient is a widely used method to establish if a patient is fit for conscious sedation and general anesthetic:[17]
- ASA 1: A normal healthy patient
- ASA 2: A patient with mild systemic disease
- ASA 3: A patient with a severe systemic disease that is not life-threatening
- ASA 4: A patient with a severe systemic disease that is a constant threat to life
Airway assessment is essential in case of a serious complication during the procedure requiring airway support. The modified Mallampati score is a common example:[18]
- Class 0: Any part of the epiglottis is visible
- Class I: Soft palate, uvula, and pillars are visible
- Class II: Soft palate and uvula are visible
- Class III: Only the soft palate and base of the uvula are visible
- Class IV: Only the hard palate is visible
All options must be considered for each patient to avoid a blanket approach. Every effort should be made to adopt the least invasive technique, and desensitization methods should be at the forefront of the mind. This enables practitioners to formulate a specific indication (or contraindication), ensuring actions are justified and in the patient's best interests.[15]
Technique or Treatment
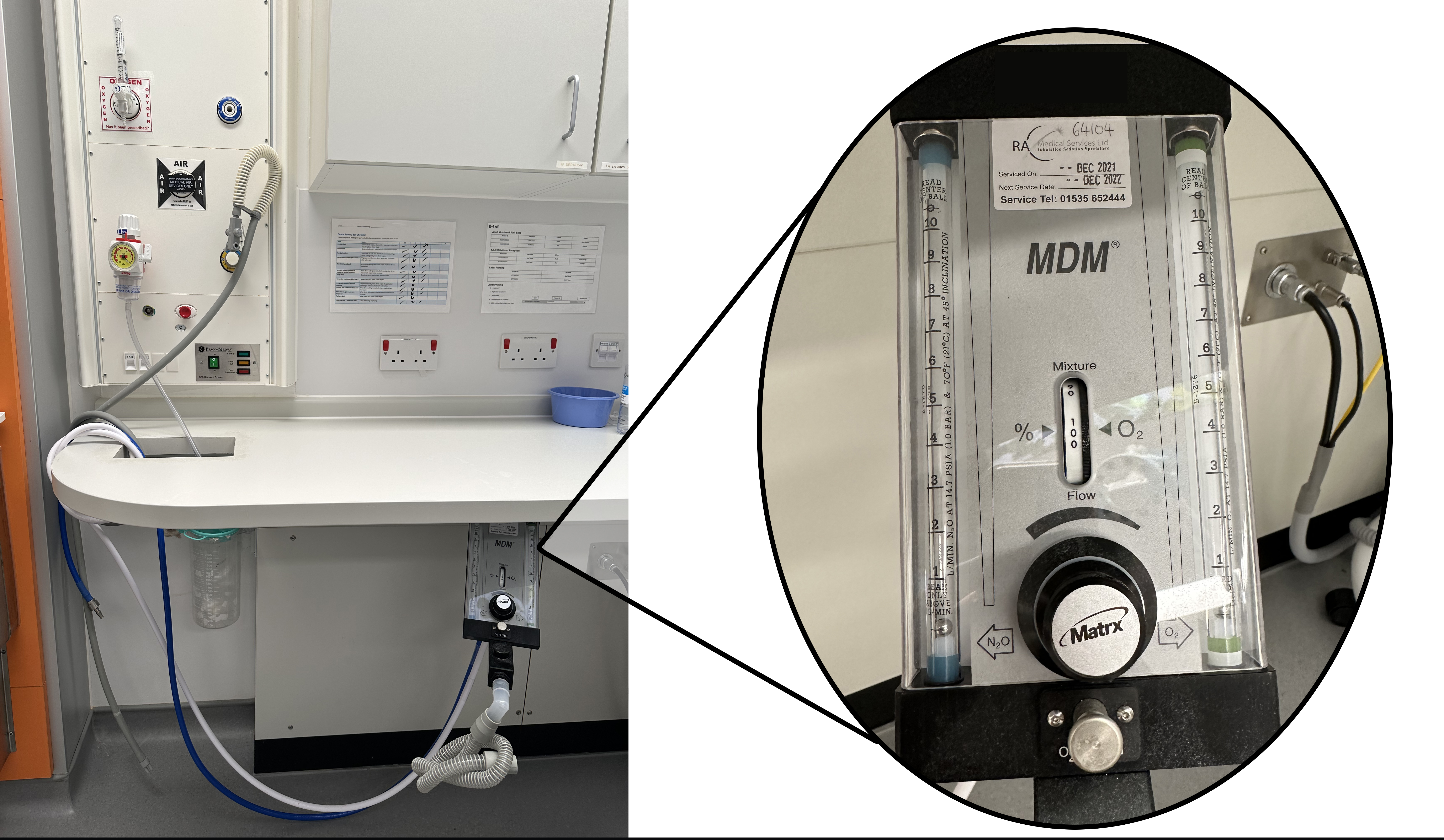
Inhalation Sedation with Nitrous Oxide/Oxygen
This technique is prominently used for children with anxiety toward dental procedures, thus making them uncooperative. Dental caries (decay) is one of the most common diseases, and if left untreated, it can lead to pain, local or systemic infection, and early loss of teeth. Utilizing this tool allows the patient to receive this essential dental treatment, preventing the abovementioned consequences. Providing therapy in a more comfortable environment lets patients overcome this barrier for future appointments. Having a cooperative patient enables dentists to provide safer and more effective treatment.[19]
The procedure begins with inhaling 100% oxygen for 2 to 5 minutes. Nitrous oxide is introduced and gradually increased every second minute. The maximum that can be given is 70%, and many machines will not physically allow any more than this. A common operational concentration is 30 to 40%. Once the procedure is finished, 100% oxygen should be given for 5 minutes. The operator must visually monitor the patient to know when an appropriate level of sedation has been reached, and behavioral management is still essential to success.[13]
Intravenous Sedation with Midazolam
Patients must attend their appointment with a designated escort available to take them patient home and be with them for the remainder of the day and overnight. The patient should be the escort's sole focus; therefore, if children are at home, they must be looked after by a different responsible adult.
When the patient enters the surgery, their blood pressure, pulse rate, and oxygen saturation will be re-checked. This monitoring will remain on the patient during the procedure and is particularly important encase of respiratory depression or over-sedation. Monitoring with equipment does not replace visual monitoring; therefore, it is imperative to use both. An intravenous cannula is then inserted; common sites are the dorsum of the hand or the anterior cubital fossa.[20]
Midazolam is commonly stored in a 5-mg vial drawn up with a needle. The drug is titrated, ensuring it is given in a controlled manner so that the patient can be monitored closely to mitigate further the risk of respiratory depression, over-sedation, or other complications. An accepted titration method is the slow injection of 2 mg of midazolam, a 90-second pause. Then further 1 mg doses at 1-minute intervals until a safe and satisfactory level of sedation is achieved.[21]
Once the treatment is complete, the patient should be monitored in recovery until they are deemed safe to leave. This decision should be based on their vital signs and a sedation-trained clinician's behavior assessment. Reminding the escort of their duty to look after the patient once they are discharged is imperative. The patient cannot drive, sign legal documents, or operate machinery for 24 hours.
If there are complications or changes to the treatment plan during intravenous sedation, arranging follow-up with the patient is good practice. Due to its amnesic effects, patients may not remember what they are told, even in recovery.
Oral Sedation with Diazepam
Typically, either 5 or 10 mg of diazepam is given one to two hours before the appointment. Patients must still attend with an escort and can't drive after the procedure. Vital signs should be recorded pre- and post-treatment, and clinicians should monitor the level of sedation to ensure the patient can still respond to verbal commands. This method is straightforward, less expensive, and requires less equipment than those above. Conversely, the drug's effect is less predictable, and it achieves a milder level of sedation compared to midazolam.[22]
Complications
Inhalation Sedation with Nitrous Oxide/Oxygen
In general, adverse effects or serious complications are rare. Examples are:
- Vomiting or nausea
- Laryngospasm
- Diffusion hypoxia
- Nitrous-oxide-induced vitamin B12 inactivation[19]
Intravenous sedation with midazolam:
Potential Complications
- Nausea and vomiting
- Transient desaturations
- Paradoxical reactions
- Dizziness
- Drowsiness
- Hiccough
- Hallucinations
- Respiratory depression[20]
Oral Sedation with Diazepam
As diazepam and midazolam are the same drug class, their potential complications are similar. They would be less likely in oral sedation due to the route of administration.
Clinical Significance
Dental anxiety affects children and adults, and its prevalence has been reported in the literature as approximately 20% in various population-based studies. As a result, patients can develop avoidance tendencies, potentially leading to poor dental health. This severe form of dental anxiety has been found to affect approximately 5% of the general population. When non-pharmacological anxiety management methods are insufficient, conscious sedation becomes extremely useful.[21]
Drugs used in conscious sedation can be titrated to achieve the desired balance between the procedure's safety, the operator's ability to facilitate the required treatment, and the patient's anxiolysis needs[4].
It is important to remember that adequate local anesthesia must be administered with sedative drugs. The clinician must not compensate for poor insufficient local anesthesia by deepening levels of sedation due to the potential complications associated with deep sedation, including increased morbidity and mortality. When a trained operator delivers conscious sedation effectively, it is a safe alternative to general anesthesia, which helps to reduce waiting list times and eliminate the complications associated with having a general anesthetic.[22]
Enhancing Healthcare Team Outcomes
Conscious sedation often requires an interprofessional approach to achieve the best outcome for the patient. It is less expensive than general anesthesia, which is very costly as it requires a hospital setting, specialist nurses and theatre staff, etc. In some countries, such as the United Kingdom, it is against the law to perform general anesthesia within a dental practice setting. Therefore, providing treatment under sedation in an outpatient setting can reduce the financial burden on healthcare organizations. Anesthesia or dentists trained in advanced techniques can provide poly-pharmaceutical sedation, allowing the treating dentist to focus on the required procedure.[23]
The dentist can prescribe oral anxiolytics at their initial consultation appointment for the patient to collect from a local pharmacy and take on the day of their procedure. A pharmacist may therefore be involved in the patient’s journey and ensure that they are given the correct and safe dose. Dental practitioners must thoroughly understand the proper dosing regimens, interactions, indications, and contraindications of the drugs prescribed.[24]
Sedation-trained nurses not only support the dentist by assisting with the required equipment, but they can also monitor the patient throughout the treatment and raise concerns where necessary. Following treatment, nurses can also recover the patient in a separate area, allowing the clinic to be utilized more efficiently as the dental practitioner can proceed to the next patient. All team members must be sedation trained, correctly indemnified, and competent to carry out treatment under sedation. A logbook detailing each treatment should be recorded for patient safety reasons and as a resource for audits to improve current practice.[25]
Media
References
Pollock H, Forman S, Pollock T, Raccasi M. Conscious sedation/local anesthesia in the office-based surgical and procedural facility. Clinics in plastic surgery. 2013 Jul:40(3):383-8. doi: 10.1016/j.cps.2013.04.014. Epub 2013 May 23 [PubMed PMID: 23830746]
Bahar E, Yoon H. Lidocaine: A Local Anesthetic, Its Adverse Effects and Management. Medicina (Kaunas, Lithuania). 2021 Jul 30:57(8):. doi: 10.3390/medicina57080782. Epub 2021 Jul 30 [PubMed PMID: 34440986]
Craig DC, Wildsmith JA, Royal College of Anaesthetists, Royal College of Surgeons of England. Conscious sedation for dentistry: an update. British dental journal. 2007 Dec 8:203(11):629-31 [PubMed PMID: 18065980]
Becker DE, Rosenberg M. Nitrous oxide and the inhalation anesthetics. Anesthesia progress. 2008 Winter:55(4):124-30; quiz 131-2. doi: 10.2344/0003-3006-55.4.124. Epub [PubMed PMID: 19108597]
Emmanouil DE, Quock RM. Advances in understanding the actions of nitrous oxide. Anesthesia progress. 2007 Spring:54(1):9-18 [PubMed PMID: 17352529]
Level 3 (low-level) evidenceBounds CG, Nelson VL. Benzodiazepines. StatPearls. 2023 Jan:(): [PubMed PMID: 29261973]
Dhaliwal JS, Rosani A, Saadabadi A. Diazepam. StatPearls. 2023 Jan:(): [PubMed PMID: 30725707]
Wong M. Reversal Agents in Sedation and Anesthesia Practice for Dentistry. Anesthesia progress. 2022 Apr 1:69(1):49-58. doi: 10.2344/anpr-69-01-09. Epub [PubMed PMID: 35377935]
Maeda S, Miyawaki T, Higuchi H, Shimada M. Effect of flumazenil on disturbance of equilibrium function induced by midazolam. Anesthesia progress. 2008 Fall:55(3):73-7. doi: 10.2344/0003-3006-55.3.73. Epub [PubMed PMID: 18788841]
Level 1 (high-level) evidenceKapur A, Kapur V. Conscious Sedation in Dentistry. Annals of maxillofacial surgery. 2018 Jul-Dec:8(2):320-323. doi: 10.4103/ams.ams_191_18. Epub [PubMed PMID: 30693254]
Working Group on Guidelines Development for Intravenous Sedation in Dentistry, the Japanese Dental Society of Anesthesiology. Practice Guidelines for Intravenous Conscious Sedation in Dentistry (Second Edition, 2017). Anesthesia progress. 2018 Winter:65(4):e1-e18. doi: 10.2344/anpr-65-04-15w. Epub [PubMed PMID: 30702348]
Level 1 (high-level) evidenceHasan A, Sharma V. Substance abuse and conscious sedation: theoretical and practical considerations. British dental journal. 2019 Nov:227(10):923-927. doi: 10.1038/s41415-019-0897-z. Epub [PubMed PMID: 31758135]
Ashley P, Anand P, Andersson K. Best clinical practice guidance for conscious sedation of children undergoing dental treatment: an EAPD policy document. European archives of paediatric dentistry : official journal of the European Academy of Paediatric Dentistry. 2021 Dec:22(6):989-1002. doi: 10.1007/s40368-021-00660-z. Epub 2021 Aug 28 [PubMed PMID: 34453697]
Benzoni T, Cascella M. Procedural Sedation. StatPearls. 2023 Jan:(): [PubMed PMID: 31869149]
O'Halloran M. The use of anaesthetic agents to provide anxiolysis and sedation in dentistry and oral surgery. The Australasian medical journal. 2013 Dec 31:6(12):713-8. doi: 10.4066/AMJ.2013.1836. Epub 2013 Dec 31 [PubMed PMID: 24391684]
Liew J, Winston M. Retrospective audit of midazolam dose and intravenous sedation record keeping in a primary care oral surgery service. Primary dental journal. 2022 Mar:11(1):50-57. doi: 10.1177/20501684221085846. Epub [PubMed PMID: 35383494]
Level 2 (mid-level) evidenceDoyle DJ, Hendrix JM, Garmon EH. American Society of Anesthesiologists Classification. StatPearls. 2023 Jan:(): [PubMed PMID: 28722969]
Stutz EW, Rondeau B. Mallampati Score. StatPearls. 2023 Jan:(): [PubMed PMID: 36256766]
Chi SI. Complications caused by nitrous oxide in dental sedation. Journal of dental anesthesia and pain medicine. 2018 Apr:18(2):71-78. doi: 10.17245/jdapm.2018.18.2.71. Epub 2018 Apr 27 [PubMed PMID: 29744381]
Papineni A, Lourenço-Matharu L, Ashley PF. Safety of oral midazolam sedation use in paediatric dentistry: a review. International journal of paediatric dentistry. 2014 Jan:24(1):2-13. doi: 10.1111/ipd.12017. Epub 2012 Dec 13 [PubMed PMID: 23240863]
Wide Boman U, Carlsson V, Westin M, Hakeberg M. Psychological treatment of dental anxiety among adults: a systematic review. European journal of oral sciences. 2013 Jun:121(3 Pt 2):225-34. doi: 10.1111/eos.12032. Epub 2013 Mar 28 [PubMed PMID: 23659254]
Level 1 (high-level) evidenceHarbuz DK, O'Halloran M. Techniques to administer oral, inhalational, and IV sedation in dentistry. The Australasian medical journal. 2016:9(2):25-32. doi: 10.4066/AMJ.2015.2543. Epub 2016 Feb 29 [PubMed PMID: 26989448]
Ashley PF, Parry J, Parekh S, Al-Chihabi M, Ryan D. Sedation for dental treatment of children in the primary care sector (UK). British dental journal. 2010 Jun:208(11):E21; discussion 522-3. doi: 10.1038/sj.bdj.2010.542. Epub [PubMed PMID: 20543774]
Level 2 (mid-level) evidenceFinn K, Kwasnicki A, Field EA, Randall C. UK Dental Medicines Advisory Service - questions asked by dentists: part 3 - prescribing of anxiolytic medications in dental practice. British dental journal. 2021 Nov:231(9):556-561. doi: 10.1038/s41415-021-3568-9. Epub 2021 Nov 12 [PubMed PMID: 34773018]
Jones N, Long L, Zeitz K. The role of the nurse sedationist. Collegian (Royal College of Nursing, Australia). 2011:18(3):115-23 [PubMed PMID: 21957664]
Level 3 (low-level) evidence