Introduction
Dental extractions are routine dental treatments offered by a range of practitioners with varying degrees of experience in oral surgery and various clinical settings. While modern dentistry focuses on patients maintaining their dentition for as long as possible, dental extractions are still commonly performed. Therefore, it is crucial that all practitioners performing dental extractions are aware of the basic principles of this treatment to perform these procedures safely and effectively.
This article focuses on non-surgical dental extractions to allow discussion of these basic principles. The non-surgical removal of a tooth relies on the progressive expansion of the bony socket within which a tooth sits, creating sufficient mobilization of the tooth, ultimately allowing for the tooth to be removed from the jaw. Dental extractions are not without risk, and all clinical and patient factors which impact this risk must be considered and discussed with the patient during the consent process.[1]
An overall understanding of relevant anatomy, extraction techniques, and perioperative factors is key to effective clinical care.
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
The relevant anatomy of a dental extraction will depend on the dental extraction site and is critical in considering appropriate anesthesia techniques and possible risks of a dental extraction.
Maxilla
The maxilla is the term given to the upper jaw. The maxilla makes up part of the mid-face, encasing the upper teeth at its inferior aspect and separating the oral cavity from the nasal floor and maxillary sinuses at its superior aspect. The cortical plates of the maxilla are thinner than those in the mandible, with the buccal cortices being thinner than the palatal cortices.[2] The thinner buccal cortex facilitates better penetration of local anesthesia via a supra-periosteal infiltration technique. The softer, thinner bone allows easier expansion of the dental socket, facilitating tooth removal usually with more ease than in the mandible.[3] The maxilla is more highly vascularised than the mandible, contributing to quicker and better post-extraction healing.
Mandible
The mandible refers to the lower jaw. The mandibular shape can often be simplified as a 'horseshoe' shape. The body of the mandible is the horizontally curved portion of bone that, with the symphyseal area anteriorly, holds the lower teeth. The body of the mandible ends posteriorly at the angle of the mandible, and the bone then continues vertically as the mandibular rami. The superior aspect of the mandible consists of the coronoid processes. The anterior aspect of the coronoids is a continuation of that of the ramus, and the posterior aspect of the coronoid makes up one side of the mandibular notch. Posterior to the coronoid processes, still on the superior aspect of the mandible, is the condylar heads that sit in the glenoid fossae of the temporal bones.[4] Between the condyle and the wall of the fossa sits an articular disc.[5] Together, these structures comprise the temporomandibular joint.
The mandibular bone has thicker cortices and trabecular bone and is less vascularised than the maxilla, tending towards more difficult extractions and slower healing response.[6] On the medial aspect of the mandibular rami sits the mandibular foramen. Adjacent to the mandibular foramen sits a bony protuberance called the lingula. The lingula is palpable in the oral cavity and provides an important anatomical landmark for administering an inferior alveolar nerve block.[7]
Nerves
Understanding the anatomy of the sensory network, which innervates the teeth, surrounding bone, and soft tissue is crucial in understanding how to make an extraction comfortable for a patient. The fifth cranial nerve (CN V), also known as the trigeminal nerve, divides into three main branches. The first branch (V1) is the ophthalmic nerve, which innervates the forehead, eyes, and nose. The second branch (V2) is the maxillary nerve, a sensory nerve that supplies sensation to much of the middle-third of the face and subdivides into the superior alveolar nerves, which provide sensation to the maxillary dentition.[8]
The posterior superior alveolar nerve branches directly off the maxillary nerve and innervates the maxillary molar teeth and adjacent buccal gingivae.[9] Another division of the maxillary nerve is the infraorbital nerve, which subdivides into the anterior superior alveolar nerve and the middle superior alveolar nerve, innervating the anterior teeth and the premolars along with their surrounding gingivae, respectively.[9]
The innervation of the hard palate is also supplied by branches of the maxillary nerve, specifically, the greater palatine and nasopalatine nerves, which branch further to supply sensation to the palatal bone. The anesthesia of these nerves and their subdivisions facilitates the extraction of an upper tooth. Common anesthesia techniques for maxillary teeth include buccal and palatal infiltrations and regional nerve blocks.
The mandibular nerve is the third branch of the trigeminal nerve (CN V3). The mandibular nerve gives sensory innervation to the lower face, including the mandible, the lower teeth, the oral mucosa, the anterior two-thirds of the tongue, the chin, and the lower lip. The mandibular nerve divides into an anterior and posterior trunk. The posterior trunk divides into the lingual and inferior alveolar nerves. The lingual nerve innervates the anterior two-thirds of the tongue but does not provide the sensation of taste. The inferior alveolar nerve innervates the mandibular teeth, their mucoperiosteum, and the lower lip and chin.[10]
The inferior alveolar nerve enters the mandible via the mandibular foramen and travels within the bone in the mandibular canal. It exits the bone again via the mental foramen as the mental nerve. The anesthesia of the inferior alveolar nerve before it enters the bone via the mandibular foramen constitutes a successful inferior alveolar nerve block.[11]
The lingual nerve enters the oral cavity separately from the inferior alveolar nerve, running anterior and inferior to the medial surface of the mandible and passing adjacent to the apices of the mandibular third molars.[12] This is relevant when considering the extraction of mandibular third molars and the associated risks.
Maxillary Sinus
Sinuses are air-filled spaces lined with mucosa. The maxillary sinuses (or antra) are one of four pairs of paranasal sinuses in the skull. The maxillary sinus communicates via its ostium with the middle meatus of the nasal cavity. The antral floor can lie adjacent to the apices of the upper posterior teeth, or the apices of the teeth can sit within the antrum itself. A possible sequela of the removal of upper posterior teeth is, therefore, the creation of an oro-antral communication (OAC), which, if left to epithelialize, can become an oro-antral fistula (OAF).[13] The risk of this must always be evaluated radiographically before the removal of upper posterior teeth, and an appropriate discussion must be had with the patient during the consent process.
Teeth
The anatomy of the teeth themselves is a crucial consideration when planning a dental extraction. The root morphology of each individual tooth must be considered - including the number of roots, divergence or convergence, root length, root shape, communication of roots with adjacent structures, dilaceration of the roots, and any existing root filling or treatment. The crown must also be considered, especially when assessing caries, as this will affect the feasibility of removing the tooth as a whole. Finally, the condition of the surrounding bone must be assessed, as any resorption of this bone due to apical pathology or periodontal disease will be key in determining the complexity of a dental extraction.
Indications
A dental extraction can be offered to patients for a multitude of reasons. While the emphasis is always placed on retaining as much of the dentition as possible, there are cases where this is no longer feasible or in the patient's best interest.
Dental Caries
When dental caries have progressed significantly, there is often not enough sound tooth tissue to allow for a restoration of any kind. This would render a tooth unrestorable, leaving extraction as the only viable treatment option. Caries are widely accepted as the primary reason for tooth removal.[14]
Pulpal/Apical Pathology
A common sequela of dental caries is pulpal and periapical pathology. A dental extraction would be indicated for a tooth with pulpal, or apical pathology that cannot be resolved with endodontic treatment or that would not be restorable following the endodontic treatment. In some cases, a dental extraction is indicated when the patient chooses not to have endodontic treatment but would still like the tooth to be treated.
Severe Periodontal Disease
Severe periodontal disease leads to the destruction of bone in the maxilla or mandible. Once a tooth has lost most of its bony support, it will become mobile and often an irritation to patients. As there are few options for bony regeneration, extraction is often indicated.
Fractured Teeth
Fractured teeth that cannot be appropriately restored or retained will require extraction.[15]
Retained Dental Roots
Retained dental roots can be present after crown fractures due to caries or trauma or following incomplete dental extraction. Some situations will allow for the retention of a dental root, such as for prosthetic reasons or due to the risk of damaging surrounding structures in an attempt to retrieve them.[16] However, they have the potential to cause infection and pain and are thus commonly advised for pre-emptive removal.
Impacted Teeth
Impacted teeth are those that cannot erupt due to a physical barrier.[17] Teeth that are impacted against other teeth or within the jaw are often considered for removal. If left impacted within the jaw, impacted teeth follicles have the potential for cystic change.[18]
A joint decision should be had with the patient as to whether prophylactic extraction or radiographic monitoring is preferable. Impaction of teeth is seen most commonly with teeth late in eruption chronology - namely mandibular third molars, upper canines, and lower premolars.[19] National clinical guidelines often govern the specific indications for mandibular third molar removal.
Supernumerary Teeth
A supernumerary tooth is defined as a tooth that is additional to the normal series. They present most commonly in the anterior maxilla. Supernumeraries can cause a range of clinical issues, including failure of eruption or displacement of a permanent tooth, dental crowding, and pathology.[20] If retention of a supernumerary tooth is not considered beneficial, then it is often planned for removal.
Orthodontic Extractions
Teeth are often considered for extraction for orthodontic reasons, often to create space in the dental arch to allow movement of the teeth into a more favorable position.[21] A plan for which teeth are to be removed should be formulated by an orthodontist.
Pre-prosthetic Extractions
Extraction of some teeth can be considered if it contributes to a better-fitting patient prosthesis or if teeth are considered to have a poor enough prognosis that they will later on adversely affect the suitability of a prosthesis.[22]
Tooth In a Fracture Line
When a patient sustains a mandibular fracture, the pattern of this fracture will be assessed clinically and radiographically. If the fracture line is seen to pass through a tooth considered a potential source of infection, a possible inhibitor to the fracture healing, or when the tooth itself is fractured, removing the tooth may be regarded as prudent.[23] This is usually done at the time of surgery for the fixation of the mandibular fracture.
Teeth with Associated Pathology
Teeth associated with pathologies, such as cysts of the jaws or malignancies, may be recommended for extraction.[24]
Prior to Radiotherapy
Patients undergoing radiotherapy, often for cancers of the head and neck, are usually required to have a dental assessment before commencing radiotherapy. This is to allow the identification of teeth with a poor prognosis or the potential to cause symptoms or infection in the near future. This is required as dental extractions in the irradiated patient carry a risk of osteoradionecrosis of the jaws, which should be avoided where possible.[25]
Contraindications
There are few absolute contraindications to dental extraction, especially when presented with an acutely symptomatic tooth. However, there are circumstances where a patient should be better optimized before extraction is performed. In all cases, a thorough risk vs. benefit discussion of tooth removal must be had with the patient. This discussion must encompass an understanding of the patient's medical background and the specific tooth or teeth being extracted.
Uncontrolled Medical Conditions Which Impact Dental Extractions
In all cases where a patient presents with an uncontrolled medical diagnosis, all reasonable efforts should be made to liaise with the patient's medical team or general medical practitioner to allow them to control the patient's condition. Once this has been achieved, it would be suitable to reassess the patient for their extraction.
Neurological Conditions
Conditions such as uncontrolled epilepsy put patients at an increased risk of aspiration or injury if a seizure occurs during an extraction.[26]
Patients with a history of hypertension or cerebrovascular disease are at a higher risk of stroke. It is important to clarify if they have had any previous transient ischaemic attacks (TIAs). If a patient is at an increased risk of stroke without any medical management, it is advisable to resolve this before dental extractions. It is important to note that while not a contraindication to dental extractions, many stroke-risk or post-stroke patients are on blood thinning medication, and appropriate hemostatic measures should be considered.
Respiratory Conditions
Respiratory conditions, such as chronic obstructive pulmonary disease (COPD), are not a total contraindication to dental extractions. However, many of these patients will prefer to be treated sitting up due to breathlessness experienced when lying flat.[27] Respiratory disorders can be a contraindication to dental treatment under sedation due to respiratory depression caused by the drugs used for dental sedation. This should be assessed with a thorough pre-sedation assessment of the patient.
Cardiovascular Conditions
Cardiovascular disease (CVD) is a term that covers a range of conditions, including ischaemic heart disease, infective endocarditis, hypertension, and dysrhythmias. Infective endocarditis (IE) is often discussed in the context of dental treatment. Prior to 2008, a range of clinical guidelines recommended antibiotic prophylaxis for certain cases where patients were at risk of developing IE.[28] This recommendation has broadly been dropped, as the risk of developing IE directly due to tooth extraction was thought to be overstated. However, patient-specific considerations should be discussed with the patient's cardiologist before extraction is performed.
Renal Impairment
Patients who have severe renal impairment can be complicated to manage. They are often at risk of increased bleeding and contracting infections. Where possible, it is appropriate to avoid surgical intervention for these patients. Due to their increased risk of infection, antibiotic prophylaxis is also often appropriate. Renal patients may also be immunosuppressed if they have received a transplant. A clear understanding of a patient's renal diagnoses and liaising with the patient's renal team is advisable before dental extraction.
Immunocompromised Patients
Immunocompromised patients are at risk of developing systemic infections following invasive dental treatment such as extractions. They must be carefully handled, and liaison with their medical teams is advised. Antibiotic prophylaxis in this group is not necessarily required as there is no clear evidence that prophylactic antibiotics reduce post-operative infection. Each case should be assessed individually, and appropriate advice should be sought.
Other conditions, such as hematological and hepatic conditions and diabetes, pose similar issues relating to dental extractions, as outlined above.
Medical Factors
Antiresorptive Agents
Antiresorptive agents, such as bisphosphonates and denosumab, are primarily used to treat osteoporosis, cases of hypercalcemia related to malignancy, multiple myeloma, Paget's disease, and other skeletal changes.[29] This group of drugs inhibits bone remodeling, which can reduce the healing of an extraction socket. The condition of a non-healing extraction socket - which may include exposed bone - is known as medication-related osteonecrosis of the jaws (MRONJ).[30]
A thorough dental assessment should be conducted before a patient begins a course of antiresorptive drugs. This allows any tooth with a poor prognosis to be removed before introducing MRONJ risk. However, it cannot always be avoided that a tooth requires extraction during or after antiresorptive treatment. Therefore, in these scenarios, a thorough risk vs. benefit discussion must be had with the patient prior to planning for an extraction.
Bisphosphonates can be administered in various ways, including orally and intravenously. A thorough history of bisphosphonate type, administration, and duration of use must be taken, as this will dictate the patient's risk of developing MRONJ. Higher risk factors have been identified, including over five years of use, concurrent steroid use, and advanced patient age.[31]
Drug holidays are not advised with these drugs, as omitting doses does not negate the cumulative effect of these drugs. If a tooth does need to be removed following bisphosphonate therapy has begun, a thorough history should be taken from the patient, liaising with their medical team should be done if appropriate and clear consent and follow-up should be conducted with the patient.
Steroid Use
Steroids are prescribed to patients for a variety of reasons. Over time, they impair healing, which must be considered with dental extractions. Additionally, some evidence suggests the benefit of doubling one dose of steroids prior to extraction to compensate for adrenal suppression. However, this depends on the type and dose of steroid a patient takes; if required, liaising with the patient's steroid prescriber can be advisable.
Anticoagulants and Antiplatelet Drugs
Anticoagulants and antiplatelets are widely prescribed, so familiarity with them and their impacts on dental treatment are imperative. A clear understanding of why a patient is on such a drug and their medical background is essential when considering omitting doses of such medication to allow for dental treatment. Evidence suggests that omitting doses of anticoagulants and antiplatelets is not routinely indicated, as the risk of missing doses on the patient's overall health must be balanced against the risk of oral bleeding, which can usually be locally controlled.[32] In all cases of a patient taking an anticoagulant or antiplatelet, local hemostatic measures should be taken following dental extractions.
Warfarin management is straightforward, as the international normalized ratio (INR) test is easily done in dental surgery and provides a quantitative measure of the patient's bleeding tendency. Evidence indicates that if a patient has an INR of under 4.0, they are suitable for dental extractions in the primary care setting and that over 4.0, they should be treated in secondary care.[32] The INR reading should be taken within 72 hours of dental treatment to be considered valid. Local hemostatic measures should be used routinely for patients on warfarin.
The introduction of novel oral anticoagulants (NOACs) has partially replaced warfarin usage. There is no INR-equivalent test for the NOACs; therefore, the management of these patients is a clinical judgment.
Local hemostatic measures include the use of oxidized cellulose materials in extraction sockets and the use of sutures to help minimize post-operative bleeding.
Radiotherapy
Patients undergoing or undergoing radiotherapy, especially in the head and neck region, are at risk of developing osteoradionecrosis (ORN).[33] Similarly to MRONJ, osteoradionecrosis presents as a non-healing area of bone that may be exposed to the oral cavity. A thorough dental assessment should be done before commencing radiotherapy. A thorough risk vs. benefit discussion with the patient is critical in this scenario, and specialist input or referral may be required.
Tooth-specific Factors
Proximity to Vital Structures
Proximity to the inferior dental nerve (IDN) is a common reason for deciding against dental extractions, primarily wisdom teeth. Radiographic signs of mandibular third molars close to the IDN include banding of the roots, loss of cortication of the IDN, and deviation of the IDN. Cone beam computerized tomography is useful in cases where the relationship between a mandibular molar and the IDN needs further investigation and visualization. The introduction of coronectomy techniques, where the coronal portion of the crown is removed to below the level of the cementoenamel junction, and the roots brought to at least 3 mm below the level of the surrounding bone, has provided an alternative treatment to total extraction of the tooth in scenarios where there is concern over IDN injury risk.[34]
Proximity to the antral sinuses can be a reason for caution when planning an extraction due to the potential to create an oroantral communication (OAC). However, if a tooth is acutely symptomatic, a high risk of an OAC may not be a sufficient reason to avoid extraction. Radiographic signs that a root apex sits in the sinus include deviation of the sinus floor, a lack of continuity of the sinus floor, and long roots visually invading the antral space. A clear consent process with the patient is key in these scenarios.
Equipment
Careful selection of the appropriate equipment for each extraction and patient scenario is key to successfully removing a tooth as efficiently, safely, and non-traumatically as possible. Therefore, it is crucial that any clinician undertaking dental extractions is aware of the various equipment options available to them and be able to choose from them appropriately. While the equipment detailed below is by no means an exhaustive list, it aims to describe some commonly known examples of each piece of equipment that may be required during a dental extraction and how they are best utilized.
Dental Anesthesia Equipment
Extractions are usually facilitated by the administration of appropriate anesthesia. The equipment required for local anesthesia delivery consists of a syringe, a needle, and a plunger. The syringe casing and plunger may be single-use or reusable. The needle is double-ended, with one end piercing the dental anesthesia cartridge and the other end being used to pierce the mucosa. Dental needles are commonly available in three lengths: extra-short, short and long. A short needle is usually approximately 21 mm, while a long needle is approximately 32 mm, this extra length facilitating block injections. The diameter of a dental needle is known as the gauge - the higher the gauge, the smaller the diameter. Dental needles are available in 25, 27, and 30 gauge. Studies show that patients cannot perceive a difference in pain with the different gauges, and a 30-gauge needle is no longer recommended for use.[35]
Dental local anesthesia is available in many drug formulations and concentrations, including lidocaine 2% with 1:80,000 parts adrenaline, articaine 4% with 1:100,000 parts adrenaline, and prilocaine 3% with felypressin. There are varying levels of evidence to support which formulations are more potent than the others.[36] The inclusion of adrenaline in local anesthesia primarily acts as a vasoconstrictor element, which prolongs the time period for which the anesthetic agent is in contact with the neural fibers.[37]
Elevators
Elevators are instruments used partly to sever the periodontal ligament from the tooth to be extracted. They are also used to lift the tooth coronally out of the socket, sometimes resulting in the avulsion of the tooth or facilitating the application of forceps on the tooth.[38] They can also be used to complete sectioned roots and elevate roots out of the dental socket. Elevators should be applied perpendicular to the long axis of the tooth, with both parts of the elevator placed on hard surfaces. The inner aspect of the elevator tip should be placed on tooth tissue. The outer aspect of the elevator tip should be placed on the alveolar bone and not on the neighboring tooth.[39] This is because the elevation of the tooth relies on using the application point of the elevator as a fulcrum or a leverage point, which could inadvertently result in the movement of the neighboring tooth.
Coupland Elevators
Coupland elevators come in three sequential widths: Couplands 1, 2, and 3. They all have a straight tip. They can be used sequentially, allowing for gradual dental socket expansion and increased tooth elevation. Alternatively, they can be used individually in relation to the space available between the tooth and the dental socket wall.
Warwick James Elevators
Warwick James elevators have three iterations: straight, left-curved, and right-curved. The straight Warwick James elevator can be used similarly to Coupland elevators, but due to the smaller width of the tip, it is suitable for smaller spaces. The right and left-curved elevators are applied in a similar fashion to the straight elevators but are used in a "scooping" motion. For example, when used for a maxillary third molar, the appropriate-sided elevator is chosen, and the inner aspect of the elevator is applied along the curve of the tooth's roots, with the curved tip placed as apically as possible. The elevator is then rotated to displace the tooth distally, usually facilitating its removal.
Cryers
Cryers are available in left- and right-curved, similar to Warwick James elevators. However, the tip of these elevators is much sharper with a wider base, making them triangular in shape. This makes Cryers especially useful for elevating root apices at the base of a socket when the adjacent root has been removed. For example, if a mesial root has been removed entirely, but a small portion of the distal root apex remains, a Cryer can be placed in the mesial space with the tip against the distal root apex. A rotating movement is then applied to elevate the apex.
Luxators
Luxators look similar to elevators; however, they are used with different aims. They are sharp-tipped instruments that should be used along the long axis of a tooth. These instruments aim to sever the periodontal ligament attachment to the tooth and to gradually widen the alveolar socket.[40] A luxator should be gradually advanced apically along a tooth, rotating side-to-side as it advances, allowing for as much apical mobility as possible. This gradual widening of the alveolar socket creates space for the application of instruments such as forceps, allowing for a more atraumatic extraction, which is beneficial for preserving bone for possible future implant placement.[41]
Forceps
Dental extraction forceps consist of three main parts: the handle, the hinge, and the beaks. The beaks are parallel to the handle in maxillary forceps. The beaks are perpendicular to the handle in mandibular forceps. The shapes of the beaks are adapted depending on which tooth the forceps are intended to remove. The beaks are designed to grip onto the crown or root surface of teeth, but ideally, forceps should always be placed as apically as possible to avoid crown fracture.[42]
The beaks of forceps for use on multi-rooted teeth are pointed in order to engage the furcation areas of teeth. Cowhorn forceps have longer, pointed beaks, which allow them to engage deeper into the furcation of molars, making them especially useful for teeth that have lost large amounts of coronal tissue. The handle of forceps used on upper posterior teeth may have a curve at the end of the handle (known as 'Read pattern forceps'), which allows more axial force to be transmitted to the beaks.
Forceps are used to apply apical pressure onto a tooth with either a rotational or buccolingual movement or a combination of both. Correct selection of forceps for the tooth being removed is key to success in using them, and a practitioner should be aware of the variations between forceps for anterior teeth, premolars, molars, maxillary third molars, roots, and cowhorns.
Scalpel
The most commonly used scalpel in dentistry is the 15-blade. The 15-blades are commonly used for fine skin incisions and are therefore frequently used in dermatology. A 15-blade or a 15c-blade is useful for intra-oral and peri-oral use due to the fine and thin tip required to work in this relatively small area.[43]
Surgical Handpiece and Burs
Surgical handpieces are used with burs to remove bone during surgical extractions. While the scope of this article is routine extractions, it is important to know the equipment required should a routine extraction become more complex. Surgical handpieces should be used for bone removal over traditional high-speed air turbine dental handpieces as surgical handpieces do not expel air, which reduces the risk of the patient developing surgical emphysema.[44] Surgical burs should be used in conjunction with sterile saline to cool the bur.
The two main types of surgical burs are fissure burs and round burs. Round burs are often used for buccal bone removal as they do not create sharp edges. Fissure burs can also be used for bone removal and for sectioning of crowns and roots.
Additional Equipment Considerations
Additional equipment, such as personal protective equipment, suction, and appropriate lighting, must also be utilized for effective treatment.
Personnel
Pre-operative assessment of a patient for extraction should be done by dentists, ideally by the same dentist who is due to perform the extraction. However, this is not always possible in a secondary care environment. The dental extraction itself is always performed by the dental surgeon. The dental assistant's role centers on ensuring the required equipment are available and given to the operator at the appropriate points.
The dental assistant is also highly valuable during the extraction process by ensuring good surgical site visibility through a combination of suction and soft-tissue retraction. The dental assistant can also provide post-operative instructions to patients after the extraction if they are appropriately trained. The surgeon must remove their sharp instruments from the tray and dispose of them correctly. The dental assistant or a decontamination team should properly sterilize or dispose of the remaining equipment.
Preparation
A thorough consultation should be conducted with a patient before a dental extraction is performed. Ideally, the consultation and the treatment should be performed on separate occasions to allow the patient time to confirm that they are happy to proceed with the treatment.
During this consultation appointment, a thorough medical history should be taken. This should include any medical diagnoses and conditions, all medications the patient regularly takes - both prescription and non-prescription - along with any allergies. Any subsequent considerations based on this medical history should be explored. These diagnoses can have medical impacts, as described in previous sections, and also may impact the ideal timing of treatment. A patient's weight may also be prudent to take to allow for a maximum safe dosage of local anesthesia to be calculated.
A clear diagnosis should be in place before considering extraction. The patient's symptoms should be explored, and a causative tooth should be identified prior to presenting dental extraction as a treatment option. This will avoid unnecessary dental extractions, for example, in cases where facial pain mimics dental pain.[45] Once a diagnosis has been made, all relevant treatment options should be presented to the patient.
If a patient does choose to proceed with the extraction of the causative tooth, then a consent discussion must be had. This should cover all the commonly occurring risks of dental extraction - pain, bleeding, bruising, swelling, infection - and less frequently occurring risks. Clinicians may wish to discuss potential damage to adjacent teeth as this can happen during treatment, especially if neighboring teeth are heavily restored.
Site-specific risks should also be discussed, such as IDN injury causing a temporary or permanent altered sensation in the lip, cheek, tongue, and teeth, an altered sense of taste, or OAC formation. It should be emphasized to the patient that these site-specific risks are rarer. However, the clinician should ensure they have conducted enough investigations to understand each patient's specific level of risk for these site-specific complications. The patient's consent should be recorded in written format and re-confirmed on the day of treatment.
If required, further investigations should be performed. Clinicians should always have a radiograph of the tooth they intend to take out. This radiograph should include the apex of the tooth. Based on this radiograph, further investigations, such as cone beam CT imaging, may require a complete consent discussion with the patient.
Patients may have medical-specific factors that should be handled before treatment is conducted. For example, if liaising with a patient's medical team is required, this should be done prior to treatment to ensure that any pre or post-operative instructions are given to the patient in good time. If a medication is to be suspended or dosage changed, then the patient should also be informed of this in good time to allow them to do so before their extraction.
At the treatment appointment, the clinician should indicate to their assistant what equipment they think they should need based on which tooth they are extracting and other factors such as loss of coronal tissue of the tooth. The assistant should then have this equipment ready for when treatment starts. Consent should be re-confirmed with the patient prior to treatment starting. The clinician should have thoroughly reviewed previous notes and radiographs of the relevant tooth to be prepared for the upcoming treatment.
Technique or Treatment
This section aims to provide an overview of techniques for each sequential step of performing a routine dental extraction. This assumes that the steps outlined in the previous 'preparation' section have all been carried out.
Anesthesia
An appropriate anesthesia technique should be chosen according to which tooth is anesthetized. For maxillary teeth, a buccal and palatal infiltration is usually sufficient. This is ideally delivered using a short needle with a local anesthetic agent appropriate to the patient; usually, lidocaine or articaine is used. An inferior dental nerve block is usually used and supplemented with a buccal infiltration for mandibular teeth, administered with a long needle. Initial anesthesia can be supplemented with intraligamentary infiltrations for all teeth, where a short or extra-short needle is inserted into the PDL space, and the anesthetic agent administered.[46]
For nerve blocks, lidocaine is usually the anesthetic agent of choice due to concern over the neurotoxic potential of articaine. However, no clear evidence supports this concern.[47]
Initial anesthesia should be administered, and an appropriate time should be given for the anesthesia to take effect. For IDN blocks, this can be up to five minutes. The patient's pain perception should first be tested by placing a dental probe into the PDL space on all tooth surfaces and applying pressure. The patient should be warned that a pressure sensation is expected, but any sharp pain should not be present. Based on the outcome of this test, the clinician will know whether further anesthesia is required. If it is, supplementary anesthesia should be given. Further doses of anesthesia may be required during the procedure.
Luxation/Elevation
Each tooth will require a different approach. However, many teeth will require some elevation or luxation. This elevation or luxation may be prior to applying forceps or sufficient to avulse the tooth. Luxators should be used in an apical motion along the long axis of the tooth, as previously described. Elevators are used perpendicular to the tooth as a lever to elevate the tooth coronally out of the socket. Appropriate types of elevators and luxators should be chosen based on the clinical and radiographic appearance of the tooth. The aim of luxation and elevation is to achieve sufficient mobility and widening of the PDL space either to avulse the tooth or apply forceps.
Should a crown fracture occur, elevators and luxators may also be used to remove the remaining root from the socket.
Forceps
Forceps should be chosen based on which tooth is being removed. Forceps should be applied as apically as possible to avoid placing undue stress on the coronal portion of the tooth, which often results in a crown fracture. Once the forceps have been placed on the tooth, a rotational movement, often combined with a buccolingual movement, should be used to increase the PDL space further and slowly remove the tooth.
Achieving Hemostasis
Following the removal of a tooth, a roll of gauze or bite pack should be placed over the socket, and the patient should be asked to bite together or hold down on the pack firmly. This pressure should be placed for a minimum of five minutes, and hemostasis should be checked before the patient can leave the chair. If hemostasis has not been achieved after a prolonged period of pressure, then local hemostatic agents should be used.
The above steps outline the usual sequence of simple removal of a tooth. Should these steps not be successful in removing a tooth, then a surgical approach may be required.
Complications
Dental extractions, much like any surgical procedure, are not without risk. These risks must be discussed with the patient before the procedure. Frequently occurring risks after dental extraction includes pain, bleeding, bruising, swelling, and infection. Damage to the adjacent structures, like neighboring teeth, should always be mentioned, especially when adjacent teeth have restorations. Site-specific risks such as oroantral communication and inferior dental nerve injury must be mentioned if appropriate.
Pain
Pain after a dental extraction is a commonly occurring postoperative risk. This is usually managed sufficiently with over-the-counter analgesics such as paracetamol and ibuprofen.[48][49] These two medications can be taken in combination to good effect.[48] However, some patients may not find these medications sufficient and may return with a primary complaint of post-operative pain. A thorough pain history and clinical examination should be taken in this scenario.
If the clinician is satisfied that there is no other diagnosis for the patient's pain, then conservative management would be advisable. Reassurance should be given to the patient that post-operative pain can take 3 to 7 days to settle.[50] Additional analgesia can be prescribed in this circumstance, such as opioids or corticosteroids.[51]
Another common reason for patients returning with post-operative pain is alveolar osteitis, known as dry socket. Alveolar osteitis occurs due to the breakdown of the blood clot in a socket before wound organization has occurred.[52] Patients with alveolar osteitis present with post-operative pain initially resolving and then increasing 1 to 3 days following the extraction. The patient may report they saw a clot being lost when spitting out, or on clinical examination, the loss of the clot will be evident. The patient may also report noticing a bad taste in their mouth or halitosis.[53]
Alveolar osteitis is usually treated with irrigation with saline along with the placement of a medicated dressing in the socket. Alvogyl is a commonly used dressing that acts as a local analgesic, an antibacterial, and an obtundent.[54]
Patients may also complain of pain associated with the temporomandibular joint following an extraction. This pain is usually myofascial in nature and can be resolved with conservative management advice and time.
Bleeding
Post-operative bleeding is a normal occurrence after tooth extraction. Any medical factors in the patient's history predisposing them to prolonged post-operative bleeding should be identified early and managed according to the relevant guidelines. If a patient does continue to bleed after a prolonged period of pressure is placed on the area, then local hemostatic agents should be used to arrest bleeding. If these are unsuccessful, localized use of tranexamic acid can also be considered.[55]
Clear safety net instructions should be provided to the patient that should they experience prolonged bleeding at home that cannot be stopped with pressure; they should seek urgent attention from a dental or medical professional.
Bruising
Some patients can experience bruising following dental extraction. However, this is more common with surgical extractions than simple ones.[56] Post-operative bruising usually resolves several days following the extraction, and patients should be warned of the possibility of bruising developing to avoid concern.
Swelling
Swelling, similar to bruising, is more common with surgical exodontia. However, a patient can experience swelling after a simple extraction. Swelling should resolve in 3 to 7 days post-extraction. However, it is possible to develop a post-operative infection, which can present as facial swelling. Therefore, examining a patient who presents with post-operative swelling for all signs of systemic infection and airway patency is crucial. Clear post-operative advice surrounding facial swellings is key. Patients should be reassured that some degree of facial swelling is normal, but also be aware of signs that a post-operative infection has developed and should seek review with a healthcare professional.
Infection
As discussed, patients must be warned about post-operative infection. Despite the risk of this developing, the evidence does not suggest there is a role for routine post-operative antibiotics.[57] Post-operative infections can be severe and are one of the more dangerous complications of exodontia.
Damage to Adjacent Teeth
The risk of damage to adjacent teeth should be minimized as much as possible through thorough pre-operative preparation and avoiding luxation or elevation adjacent to a heavily restored tooth.
Inferior Dental Nerve Injury
This risk usually pertains to mandibular third molars, although mandibular second molars can occasionally present close to the IDN. The patient should always be warned of the risk of temporary or permanent altered sensation to the lip, cheek, tongue, and teeth on the relevant side. The incidence of IDN injury is between 0.35% to 8.4%, with a permanent injury to the nerve being rare.[58]
Should a patient suffer an IDN injury, they should be followed up closely in the initial period. In most cases, recovery is seen in 6 to 8 weeks, which can take up to two years. Ideally, complete recovery should be seen within two months, as the chance of permanent deficit increases after this period.[59]
Oroantral Communication
Oroantral communication (OAC) most commonly occurs with maxillary molars. The primary reason for the formation of an OAC or oroantral fistula (OAF) is the proximity of a tooth's apices to the antral floor or the projection of the roots into the sinus. OAC can also occur following the displacement of a root or apex into the sinus during extraction by the operator. Most defects less than 2 mm can close spontaneously and be managed conservatively. However, defects that are larger than this are likely to epithelialize if left and form an OAF. This can lead to the patient developing sinusitis. These defects require surgical closure, ideally within 24 hours.[13]
Wrong-site Tooth Extraction
Removal of the wrong tooth is one of dentistry's most regrettable complications. Poor communication, referrals, and operator exhaustion are common reasons for wrong-site surgery.[60]
This does not represent an exhaustive list of all possible complications following a tooth extraction, but the above described are the most commonly experienced complications and make up the bulk of a routine consent discussion with patients.
Clinical Significance
Understanding the principles outlined is imperative to perform routine oral surgery procedures. Routine dental extractions are part of the basic treatments that all qualified dentists should be able to provide; therefore, understanding the indications and contraindications of extractions, along with appropriate medical considerations, is imperative. Additionally, the ability to appropriately prepare for dental extraction and select the correct equipment and knowledge of how to use that equipment will contribute to successful treatment. The theoretical knowledge provided in this article should complement the ongoing practical experience.
Enhancing Healthcare Team Outcomes
All members of the dental team contribute towards successful exodontia and management of the patient. The operator is responsible for thorough preparation, patient consent, and performing the required treatment. The dental assistant plays a vital role throughout this process, including retraction and suction during the treatment and provision of post-operative instructions.
The dental assistant is also crucial in being vigilant and stopping the operator should it appear that there is a risk of wrong-site surgery being performed. The whole team is important in providing reassurance to a patient throughout their treatment and making the environment feel comfortable to the patient. Overall, the entire team is crucial to a successful patient outcome.
Nursing, Allied Health, and Interprofessional Team Interventions
Dental nurses play a vital role in all extractions, such as providing a second check of the patient's details and allergies and confirming the tooth to be extracted. Techniques such as counting teeth aloud and confirming that the dentist is about to work on the same tooth as specified on the consent form rely on dental nurses being involved in providing confirmation.
Dental nurses may also be responsible for the decontamination of instruments following a procedure. All dental team members should be aware of cross-infection protocols to ensure the safety of the patient and the team.
It is the operator's responsibility to remove their sharp instruments, and the dental nurse should feel able to prompt the dentist to do so.
Dental nurses can also check for hemostasis following the extraction and provide post-operative instructions should they feel comfortable doing so.
Nursing, Allied Health, and Interprofessional Team Monitoring
Four-handed dentistry is key to making dental extractions as simple as possible. The dental nurse should be aware of the instruments required to perform an extraction and be able to provide the next appropriate instrument to the dentist.[61] They should also be able to provide appropriate soft tissue retraction, good lighting, and suction to aid with the process of tooth removal. Nurses may also check for hemostasis, although it is advisable for operators to also confirm hemostasis in cases where the patient may be predisposed to prolonged bleeding. Post-operative instructions can also be provided by nursing staff.
The administrative team should be aware of why patients may require certain times of day for their booking, such as morning appointments for patients on anticoagulants or with memory impairment.
The wider team should also be aware of the possible complications of dental extractions so they can appropriately triage phone calls or walk-ins from patients and highlight these to the clinician appropriately.
Media
(Click Image to Enlarge)
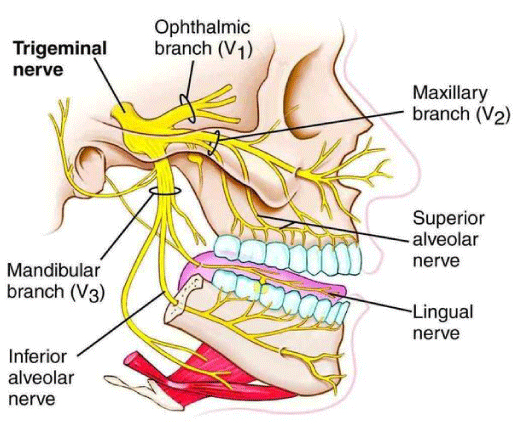
Diagram showing the innervation of the dentition by the maxillary and mandibular nerves and their subdivisions. Cited from Al-Rawee RY, Abdalfattah MM (2020) Anatomy Respect in Implant Dentistry. Assortment, Location, Clinical Importance (Review Article). J Dent Probl Solut 7(2): 068-078. DOI: 10.17352/2394-8418.000088
References
Arya R, Jadun S, Shah A. An evaluation of patient informed consent for dental extractions. Primary dental journal. 2022 Sep:11(3):98-103. doi: 10.1177/20501684221112527. Epub [PubMed PMID: 36073049]
Porto OCL, Silva BSF, Silva JA, Estrela CRA, Alencar AHG, Bueno MDR, Estrela C. CBCT assessment of bone thickness in maxillary and mandibular teeth: an anatomic study. Journal of applied oral science : revista FOB. 2020:28():e20190148. doi: 10.1590/1678-7757-2019-0148. Epub 2020 Feb 7 [PubMed PMID: 32049133]
Devlin H, Horner K, Ledgerton D. A comparison of maxillary and mandibular bone mineral densities. The Journal of prosthetic dentistry. 1998 Mar:79(3):323-7 [PubMed PMID: 9553887]
Breeland G, Aktar A, Patel BC. Anatomy, Head and Neck, Mandible. StatPearls. 2023 Jan:(): [PubMed PMID: 30335325]
Chang CL, Wang DH, Yang MC, Hsu WE, Hsu ML. Functional disorders of the temporomandibular joints: Internal derangement of the temporomandibular joint. The Kaohsiung journal of medical sciences. 2018 Apr:34(4):223-230. doi: 10.1016/j.kjms.2018.01.004. Epub 2018 Feb 7 [PubMed PMID: 29655411]
Saka B, Wree A, Henkel KO, Anders L, Gundlach KK. Blood supply of the mandibular cortex: an experimental study in Göttingen minipigs with special reference to the condyle. Journal of cranio-maxillo-facial surgery : official publication of the European Association for Cranio-Maxillo-Facial Surgery. 2002 Feb:30(1):41-5 [PubMed PMID: 12064882]
Level 3 (low-level) evidenceChoi DY, Hur MS. Anatomical review of the mandibular lingula for inferior alveolar nerve block. Folia morphologica. 2021:80(4):786-791. doi: 10.5603/FM.a2020.0135. Epub 2020 Nov 10 [PubMed PMID: 33169354]
Somayaji KS, Rao MK. Anatomy and clinical applications of the maxillary nerve in dentistry: a literature review. Dental update. 2012 Dec:39(10):727-30, 733-5 [PubMed PMID: 23367639]
Shafique S, M Das J. Anatomy, Head and Neck, Maxillary Nerve. StatPearls. 2023 Jan:(): [PubMed PMID: 31194417]
Ghatak RN, Helwany M, Ginglen JG. Anatomy, Head and Neck, Mandibular Nerve. StatPearls. 2023 Jan:(): [PubMed PMID: 29939597]
Kim C, Hwang KG, Park CJ. Local anesthesia for mandibular third molar extraction. Journal of dental anesthesia and pain medicine. 2018 Oct:18(5):287-294. doi: 10.17245/jdapm.2018.18.5.287. Epub 2018 Oct 31 [PubMed PMID: 30402548]
Fagan SE, Roy W. Anatomy, Head and Neck, Lingual Nerve. StatPearls. 2023 Jan:(): [PubMed PMID: 31536258]
Khandelwal P, Hajira N. Management of Oro-antral Communication and Fistula: Various Surgical Options. World journal of plastic surgery. 2017 Jan:6(1):3-8 [PubMed PMID: 28289607]
Broers DLM, Dubois L, de Lange J, Su N, de Jongh A. Reasons for Tooth Removal in Adults: A Systematic Review. International dental journal. 2022 Feb:72(1):52-57. doi: 10.1016/j.identj.2021.01.011. Epub 2021 Feb 26 [PubMed PMID: 33648772]
Level 1 (high-level) evidenceAida J, Ando Y, Akhter R, Aoyama H, Masui M, Morita M. Reasons for permanent tooth extractions in Japan. Journal of epidemiology. 2006 Sep:16(5):214-9 [PubMed PMID: 16951541]
Nayyar J, Clarke M, O'Sullivan M, Stassen LF. Fractured root tips during dental extractions and retained root fragments. A clinical dilemma? British dental journal. 2015 Mar 13:218(5):285-90. doi: 10.1038/sj.bdj.2015.147. Epub [PubMed PMID: 25766165]
Suri L, Gagari E, Vastardis H. Delayed tooth eruption: pathogenesis, diagnosis, and treatment. A literature review. American journal of orthodontics and dentofacial orthopedics : official publication of the American Association of Orthodontists, its constituent societies, and the American Board of Orthodontics. 2004 Oct:126(4):432-45 [PubMed PMID: 15470346]
Wali GG, Sridhar V, Shyla HN. A study on dentigerous cystic changes with radiographically normal impacted mandibular third molars. Journal of maxillofacial and oral surgery. 2012 Dec:11(4):458-65. doi: 10.1007/s12663-011-0252-7. Epub 2011 Jul 6 [PubMed PMID: 24293941]
Sarica I, Derindag G, Kurtuldu E, Naralan ME, Caglayan F. A retrospective study: Do all impacted teeth cause pathology? Nigerian journal of clinical practice. 2019 Apr:22(4):527-533. doi: 10.4103/njcp.njcp_563_18. Epub [PubMed PMID: 30975958]
Level 2 (mid-level) evidenceGarvey MT, Barry HJ, Blake M. Supernumerary teeth--an overview of classification, diagnosis and management. Journal (Canadian Dental Association). 1999 Dec:65(11):612-6 [PubMed PMID: 10658390]
Level 3 (low-level) evidenceAraújo TM, Caldas LD. Tooth extractions in Orthodontics: first or second premolars? Dental press journal of orthodontics. 2019 Aug 1:24(3):88-98. doi: 10.1590/2177-6709.24.3.088-098.bbo. Epub 2019 Aug 1 [PubMed PMID: 31390455]
Fernández-Barrera MÁ, Medina-Solís CE, Casanova-Rosado JF, Mendoza-Rodríguez M, Escoffié-Ramírez M, Casanova-Rosado AJ, Navarrete-Hernández Jde J, Maupomé G. Contribution of prosthetic treatment considerations for dental extractions of permanent teeth. PeerJ. 2016:4():e2015. doi: 10.7717/peerj.2015. Epub 2016 Jul 7 [PubMed PMID: 27441103]
Taysi M, Yildirim S. Should the teeth in the line of jaw fractures be extracted? Journal of Istanbul University Faculty of Dentistry. 2015:49(1):61-65. doi: 10.17096/jiufd.98462. Epub 2015 Jan 31 [PubMed PMID: 28955528]
Nyimi BF, Yifang Z, Liu B. The Changing Landscape in Treatment of Cystic Lesions of the Jaws. Journal of International Society of Preventive & Community Dentistry. 2019 Jul-Aug:9(4):328-337. doi: 10.4103/jispcd.JISPCD_180_19. Epub 2019 Aug 6 [PubMed PMID: 31516866]
Thorn JJ,Hansen HS,Specht L,Bastholt L, Osteoradionecrosis of the jaws: clinical characteristics and relation to the field of irradiation. Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons. 2000 Oct; [PubMed PMID: 11021701]
Pick L, Bauer J. [Dentistry and epilepsy]. Der Nervenarzt. 2001 Dec:72(12):946-9 [PubMed PMID: 11789440]
Devlin J. Patients with chronic obstructive pulmonary disease: management considerations for the dental team. British dental journal. 2014 Sep:217(5):235-7. doi: 10.1038/sj.bdj.2014.756. Epub [PubMed PMID: 25213520]
Thornhill MH, Gibson TB, Yoon F, Dayer MJ, Prendergast BD, Lockhart PB, O'Gara PT, Baddour LM. Antibiotic Prophylaxis Against Infective Endocarditis Before Invasive Dental Procedures. Journal of the American College of Cardiology. 2022 Sep 13:80(11):1029-1041. doi: 10.1016/j.jacc.2022.06.030. Epub 2022 Aug 17 [PubMed PMID: 35987887]
Landesberg R, Eisig S, Fennoy I, Siris E. Alternative indications for bisphosphonate therapy. Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons. 2009 May:67(5 Suppl):27-34. doi: 10.1016/j.joms.2008.12.006. Epub [PubMed PMID: 19371812]
Level 3 (low-level) evidenceNicolatou-Galitis O, Schiødt M, Mendes RA, Ripamonti C, Hope S, Drudge-Coates L, Niepel D, Van den Wyngaert T. Medication-related osteonecrosis of the jaw: definition and best practice for prevention, diagnosis, and treatment. Oral surgery, oral medicine, oral pathology and oral radiology. 2019 Feb:127(2):117-135. doi: 10.1016/j.oooo.2018.09.008. Epub 2018 Oct 9 [PubMed PMID: 30393090]
Bansal H. Medication-related osteonecrosis of the jaw: An update. National journal of maxillofacial surgery. 2022 Jan-Apr:13(1):5-10. doi: 10.4103/njms.NJMS_236_20. Epub 2022 Apr 20 [PubMed PMID: 35911799]
Carter G, Goss AN, Lloyd J, Tocchetti R. Current concepts of the management of dental extractions for patients taking warfarin. Australian dental journal. 2003 Jun:48(2):89-96; quiz 138 [PubMed PMID: 14649397]
Chronopoulos A, Zarra T, Ehrenfeld M, Otto S. Osteoradionecrosis of the jaws: definition, epidemiology, staging and clinical and radiological findings. A concise review. International dental journal. 2018 Feb:68(1):22-30. doi: 10.1111/idj.12318. Epub 2017 Jun 25 [PubMed PMID: 28649774]
Martin A, Perinetti G, Costantinides F, Maglione M. Coronectomy as a surgical approach to impacted mandibular third molars: a systematic review. Head & face medicine. 2015 Apr 10:11():9. doi: 10.1186/s13005-015-0068-7. Epub 2015 Apr 10 [PubMed PMID: 25890111]
Level 1 (high-level) evidenceAl-Moraissi EA, Al-Selwi AM, Al-Zendani EA. Do length and gauge of dental needle affect success in performing an inferior alveolar nerve block during extraction of adult mandibular molars? A prospective, randomized observer-blind, clinical trial. Clinical oral investigations. 2021 Aug:25(8):4887-4893. doi: 10.1007/s00784-021-03796-w. Epub 2021 Jan 19 [PubMed PMID: 33469717]
Level 1 (high-level) evidenceSt George G, Morgan A, Meechan J, Moles DR, Needleman I, Ng YL, Petrie A. Injectable local anaesthetic agents for dental anaesthesia. The Cochrane database of systematic reviews. 2018 Jul 10:7(7):CD006487. doi: 10.1002/14651858.CD006487.pub2. Epub 2018 Jul 10 [PubMed PMID: 29990391]
Level 1 (high-level) evidenceBecker DE, Reed KL. Local anesthetics: review of pharmacological considerations. Anesthesia progress. 2012 Summer:59(2):90-101; quiz 102-3. doi: 10.2344/0003-3006-59.2.90. Epub [PubMed PMID: 22822998]
Bussell MA, Graham RM. The history of commonly used dental elevators. British dental journal. 2008 Nov 8:205(9):505-8. doi: 10.1038/sj.bdj.2008.933. Epub [PubMed PMID: 18997710]
Mamoun J. Use of elevator instruments when luxating and extracting teeth in dentistry: clinical techniques. Journal of the Korean Association of Oral and Maxillofacial Surgeons. 2017 Jun:43(3):204-211. doi: 10.5125/jkaoms.2017.43.3.204. Epub 2017 Jun 28 [PubMed PMID: 28770164]
Sambrook PJ, Goss AN. Contemporary exodontia. Australian dental journal. 2018 Mar:63 Suppl 1():S11-S18. doi: 10.1111/adj.12586. Epub [PubMed PMID: 29574811]
Sharma SD, Vidya B, Alexander M, Deshmukh S. Periotome as an Aid to Atraumatic Extraction: A Comparative Double Blind Randomized Controlled Trial. Journal of maxillofacial and oral surgery. 2015 Sep:14(3):611-5. doi: 10.1007/s12663-014-0723-8. Epub 2014 Nov 8 [PubMed PMID: 26225052]
Level 2 (mid-level) evidenceMcKenzie WS. Principles of Exodontia. Oral and maxillofacial surgery clinics of North America. 2020 Nov:32(4):511-517. doi: 10.1016/j.coms.2020.06.001. Epub 2020 Aug 21 [PubMed PMID: 32839095]
Chandra S, Podder I, Chatterjee M, Field L. Anatomy and Applications of the #15 Scalpel Blade and Its Variations. Journal of cutaneous and aesthetic surgery. 2018 Apr-Jun:11(2):79-82. doi: 10.4103/JCAS.JCAS_70_16. Epub [PubMed PMID: 30210210]
Gowans K, Patel M, Lewis K. Surgical Emphysema: A Rare Complication of a Simple Surgical Dental Extraction Without the Use of an Air-Driven Rotor. Dental update. 2017 Mar:44(3):217-8, 220 [PubMed PMID: 29172328]
Renton T. Tooth-Related Pain or Not? Headache. 2020 Jan:60(1):235-246. doi: 10.1111/head.13689. Epub 2019 Nov 1 [PubMed PMID: 31675112]
Meechan JG. Intraligamentary anaesthesia. Journal of dentistry. 1992 Dec:20(6):325-32 [PubMed PMID: 1452871]
Aps J, Badr N. Narrative review: the evidence for neurotoxicity of dental local anesthetics. Journal of dental anesthesia and pain medicine. 2020 Apr:20(2):63-72. doi: 10.17245/jdapm.2020.20.2.63. Epub 2020 Apr 27 [PubMed PMID: 32395611]
Level 3 (low-level) evidenceWeil K, Hooper L, Afzal Z, Esposito M, Worthington HV, van Wijk AJ, Coulthard P. Paracetamol for pain relief after surgical removal of lower wisdom teeth. The Cochrane database of systematic reviews. 2007 Jul 18:2007(3):CD004487 [PubMed PMID: 17636762]
Level 1 (high-level) evidenceGazal G, Al-Samadani KH. Comparison of paracetamol, ibuprofen, and diclofenac potassium for pain relief following dental extractions and deep cavity preparations. Saudi medical journal. 2017 Mar:38(3):284-291. doi: 10.15537/smj.2017.3.16023. Epub [PubMed PMID: 28251224]
Seymour RA, Blair GS, Wyatt FA. Post-operative dental pain and analgesic efficacy. Part I. The British journal of oral surgery. 1983 Dec:21(4):290-7 [PubMed PMID: 6580915]
Cho H, Lynham AJ, Hsu E. Postoperative interventions to reduce inflammatory complications after third molar surgery: review of the current evidence. Australian dental journal. 2017 Dec:62(4):412-419. doi: 10.1111/adj.12526. Epub 2017 Jun 14 [PubMed PMID: 28498604]
Houston JP, McCollum J, Pietz D, Schneck D. Alveolar osteitis: a review of its etiology, prevention, and treatment modalities. General dentistry. 2002 Sep-Oct:50(5):457-63; quiz 464-5 [PubMed PMID: 12448899]
Garola F, Gilligan G, Panico R, Leonardi N, Piemonte E. Clinical management of alveolar osteitis. A systematic review. Medicina oral, patologia oral y cirugia bucal. 2021 Nov 1:26(6):e691-e702. doi: 10.4317/medoral.24256. Epub 2021 Nov 1 [PubMed PMID: 34704976]
Level 1 (high-level) evidenceSupe NB, Choudhary SH, Yamyar SM, Patil KS, Choudhary AK, Kadam VD. Efficacy of Alvogyl (Combination of Iodoform + Butylparaminobenzoate) and Zinc Oxide Eugenol for Dry Socket. Annals of maxillofacial surgery. 2018 Jul-Dec:8(2):193-199. doi: 10.4103/ams.ams_167_18. Epub [PubMed PMID: 30693231]
Jaiswal P, Agrawal R, Gandhi A, Jain A, Kumar A, Rela R. Managing Anticoagulant Patients Undergoing Dental Extraction by using Hemostatic Agent: Tranexamic Acid Mouthrinse. Journal of pharmacy & bioallied sciences. 2021 Jun:13(Suppl 1):S469-S472. doi: 10.4103/jpbs.JPBS_639_20. Epub 2021 Jun 5 [PubMed PMID: 34447136]
Yao J, Lee KK, McGrath C, Wu YN, Li KY, Mattheos N. Comparison of patient-centered outcomes after routine implant placement, teeth extraction, and periodontal surgical procedures. Clinical oral implants research. 2017 Apr:28(4):373-380. doi: 10.1111/clr.12794. Epub 2016 Mar 11 [PubMed PMID: 26970296]
Singh Gill A, Morrissey H, Rahman A. A Systematic Review and Meta-Analysis Evaluating Antibiotic Prophylaxis in Dental Implants and Extraction Procedures. Medicina (Kaunas, Lithuania). 2018 Dec 1:54(6):. doi: 10.3390/medicina54060095. Epub 2018 Dec 1 [PubMed PMID: 30513764]
Level 1 (high-level) evidenceSarikov R, Juodzbalys G. Inferior alveolar nerve injury after mandibular third molar extraction: a literature review. Journal of oral & maxillofacial research. 2014 Oct-Dec:5(4):e1. doi: 10.5037/jomr.2014.5401. Epub 2014 Dec 29 [PubMed PMID: 25635208]
Bhat P, Cariappa KM. Inferior alveolar nerve deficits and recovery following surgical removal of impacted mandibular third molars. Journal of maxillofacial and oral surgery. 2012 Sep:11(3):304-8. doi: 10.1007/s12663-012-0335-0. Epub 2012 Feb 19 [PubMed PMID: 23997481]
Jan AM, Albenayan R, Alsharkawi D, Jadu FM. The prevalence and causes of wrong tooth extraction. Nigerian journal of clinical practice. 2019 Dec:22(12):1706-1714. doi: 10.4103/njcp.njcp_206_19. Epub [PubMed PMID: 31793478]
Bhatia K, Aruede G. Oral Surgery, Instruments. StatPearls. 2023 Jan:(): [PubMed PMID: 36251846]