Introduction
Strings and animal tendons have been used to suture for thousands of years. Over time, innovations in suture materials and improved techniques decreased the complications associated with wound closure. The primary goal when suturing is to re-approximate wound edges under minimal tension enabling hemostasis and healing. This article outlines the various suture materials and needles while highlighting the techniques utilized by the oral surgeon when managing the closure of surgical wounds within the oral cavity.[1]
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
The ideal outcomes in any surgical setting are good closure and stabilization of re-approximated wound edges. However, dental surgeons are exposed to a unique challenge since they have to reapproximate and stabilize various types of soft tissue (delicate unattached mucosa vs. more substantial attached mucosa with keratinized tissue) onto varying types of hard tissue (compact and medullary bone, cementum, and titanium implant surfaces). Additional challenges include bacterial colonization, the tension created from the tongue, swallowing pattern, and masticatory function.[2]
Wound healing is a multifaceted process consisting of four sequential and overlapping phases: the hemostatic phase, inflammatory phase, proliferative phase, and maturation phase. The hemostatic phase is rapidly occurring, usually within minutes of wound closure. Exposed collagen and tissue factor initiate the hemostatic phase constricting vessels and formating the platelet plug. The platelets degranulate, releasing cytokines and growth factors originating the fibrin clot formation via the coagulation cascade. Simultaneously, the acute inflammatory phase drives the healing process, which usually lasts 72 hours. This phase is characterized by heat, pain, swelling, and redness. Increased vascularity facilitates the accumulation of cells consisting of macrophages, leukocytes, growth factors, and enzymes that rid the site of toxins, damaged cells, and bacteria.[3][4]
The proliferative phase varies in duration but generally continues for days to weeks, replacing the fibrin clot with granulation tissue and immature type III collagen. The granulation tissue comes from the extracellular matrix (ECM), consisting of collagen, elastin, hyaluronic acid, and proteoglycans. Cell types present in this phase are fibroblasts, keratinocytes, and endothelial cells. Growth factors and cytokines (TGF beta 1, 2, and 3; vascular epidermal growth factor and the interleukin family) are actively involved during this phase.[4]
The maturation and remodeling phase is the last step in wound healing. This phase consists of replacing the extracellular matrix and type III collagen with type I collagen (better organized), which can take months to years.[4]
Wounds heal by first, second, and third intention. Ideally, a wound heals by first intention whereby the wound edges are reapproximated, and the sutured is closed. The site will heal through the process mentioned above with minimal scar formation. Second intention healing is when the wound is too wide, deep, or jagged to re-approximate the tissue edges. These wounds are not closed, and the healing process begins at the wound base, migrating superficially to the epidermis. Finally, third intension healing is when a wound is infected or necrotic; therefore, it must be cleaned or drained until the infection has resolved to be definitively closed.[4][3]
Equipment
To provide consistent and repeatable wound closure, it is critical for the dental surgeon to understand the suturing armamentarium, including suture materials, needle types, and suturing instruments.[1]
A variety of suturing materials are available for use at the discretion of the dental surgeon. A key consideration when choosing the most appropriate material is tensile strength. Sutures vary in how they distribute tension across the wound after re-approximation. Tensile strength is directly related to the size of the thread material. Therefore, dental surgeons should select the smallest thread that achieves appropriate tension to minimize tissue damage. The suture material also needs to be easy to handle and provide secure knots. Thread materials utilized for suturing consist of resorbable materials and non-resorbable materials.[1]
Resorbable suture materials are most often the surgeon’s primary choice in modern dentoalveolar surgery. They eliminate the need for post-operative suture removal, reducing patient anxiety and usually result in less tissue inflammation. Resorbable suture materials consist of natural (gut and chromic gut) and synthetic materials (polyglycolic acid and polydioxanone).
Natural suture materials are composed of highly purified collagen derived from animals such as sheep and beef intestines. Surgical gut sutures are absorbed rapidly by enzymatic degradation. For this reason, surgical gut sutures are reserved for scenarios where the surgical flap is under minimal tension. The plain gut suture thread loses 50% of its tensile strength within 24 hours of exposure to the intraoral environment and completely resorbs in 3 to 5 days.
Chromic gut sutures are treated with chromium salts to extend their absorption time to approximately 7 to 10 days. These sutures maintain tensile strength for up to 5 days. As discussed before, surgical gut sutures are the most common suture material utilized in dentoalveolar surgery. Still, they are contraindicated in scenarios where the intraoral pH is decreased—for example, gastroesophageal reflux disease (GERD), antipsychotic drug therapy, and Sjogren’s Syndrome. If the surgical gut suture is used in these scenarios, it may rapidly dissolve, resulting in surgical flap dehiscence.[5][6][7][1]
The most common synthetic resorbable suture material used is made from polyglycolic acid (PGA). PGA is digested by hydrolysis, which takes 21 to 28 days in the intraoral environment. In addition to the extended absorption profile that PGA suture materials possess, it also maintains high tensile strength for approximately three weeks. PGA is the resorbable suture material of choice when placing mattress sutures to keep tension against the muscles of mastication. Its braided structure tends to improve handling characteristics and maintain knot integrity. This suture also comes coated with an antimicrobial agent. Another synthetic resorbable material commonly used to close the dermis is polydioxanone. This is a monofilament that holds 70% of its tensile strength for two weeks.[5][6][7][1]
Silk and polyester are the primary non-resorbable materials used today. Silk is inexpensive and readily available, primarily manufactured with fibers in a braided configuration. The braid allows for elasticity and the material to adhere to itself, maintaining tension within the knot allowing for secure knots. However, silk sutures are more likely to cause infection, and removal is recommended one week after placement. The braided arrangement of fibers increases surface area, which wicks fluid and bacteria into the composition of the thread. As a result, the bacteria distributes into the wound, increasing the likelihood of infection. Silk is contraindicated when used at sites where permanent structures are present such as implants or particulate grafts.[5][6]
Polyester sutures are another widely used non-resorbable material. Polypropylene, black monofilament, and polytetrafluoroethylene are the primary polyester sutures used in dentoalveolar surgery. It is critical to use a surgeon's knot versus a slipknot when closing with a polyester suture because of the material memory. The surgeon's knot will prevent the knot from coming untied. The non-absorbent polyester fibers decrease the likelihood of facilitating bacterial growth.[5]
A myriad of surgical suture needles exists on the market today. Reverse-cutting suture needles are the primary choice for dentoalveolar surgeons. The reverse-cutting needle is triangular in cross-section, where the triangle's base faces the inner part of the circle created by the needle. This shape prevents tearing oral mucosa as tension is applied during the knot tying. The 3/8-circle needle is most often used in dentoalveolar settings. However, the 1/2-circle needle is sometimes preferred where working space is restricted, such as the maxillary posterior region.[8][9]
Technique or Treatment
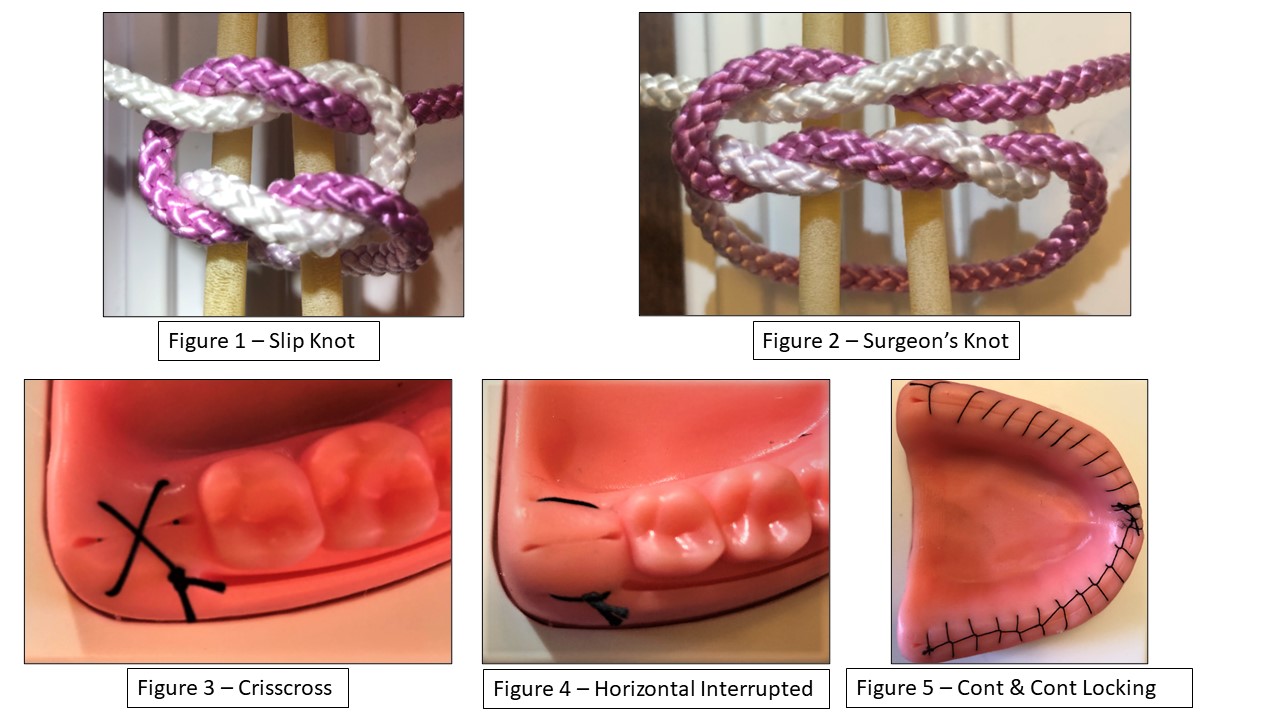
Equally important as the selection of suturing materials is the appropriately selected knot and technique. Two primary knots are utilized in dentoalveolar circumstances: the slip knot (Figure 1) and the surgeon’s knot (Figure 2).
The primary factor when selecting one or the other is the suture material utilized. A surgeon’s knot must be selected when using synthetic suture materials to prevent loosening of the knot. Synthetic sutures like polyester maintain memory (they will unravel to return to a straight position). First, a surgeon’s knot is done by tying a double overhand throw; then, an additional single overhand throw is placed in the opposite direction to lock the knot. The granny or surgical slip knot enables the surgeon to tighten the suture toward the tissue and pull the flap edges together. The slip knot may be used with gut and chromic gut suture materials. This knot is not recommended when using resorbable or non-resorbable synthetic materials. The surgical slip knot is executed by making two separate overhand knots in the same direction, pulling taught and re-approximating the wound edges without blanching the tissue, then place an additional overhand throw in the opposite direction to lock the knot.[10][5]
Suturing techniques consist of interrupted and continuous suturing methods. The simple interrupted and crisscross (Figure 3) are two interrupted techniques frequently utilized in dentoalveolar settings to approximate tension-free wounds and flaps.
The simple interrupted technique is accomplished by first penetrating the buccal gingiva, crossing the wound, and exiting the lingual tissue with the needle oriented medially throughout this movement. A loop is created, and the suture thread is tied off at the original entry point. This technique may be utilized for closing small wounds or placed in multiples to close larger wounds.[10][5]
The crisscross technique is an ideal choice for extraction sites, maintaining both the blood clot and materials packed into the socket, such as gel foam, collagen plugs, and graft material. The crisscross technique can be performed in two manners. The first is where the needle is inserted into the mesial/buccal gingiva and exits the distal/buccal gingiva. The needle crosses over the alveolar arch or extraction site, enters the mesial/lingual gingiva, and exits the distal/lingual tissue. The suture is then tied off to the non-working end of the suture thread at the original entry point on the buccal/mesial of the extraction site. The crisscross technique can also be performed where the needle enters the mesial/buccal gingiva, crosses the extraction site, and exits the mesial/lingual tissue. The suture thread is brought across the extraction site, enters the distal/buccal gingiva, and exits the distal/lingual gingiva. The suture thread is then tied off at the original entry point at the mesial/buccal non-working end. The crisscross and interrupted techniques are not recommended for flaps or wounds that are under tension.[5][10][11]
The horizontal mattress technique (Figure 4) is an interrupted suturing technique recommended for flaps under tension where the flap is released beyond the mucogingival junction. This technique is performed by first entering the mesial/buccal gingiva and exiting the mesial/lingual gingiva. The suture thread enters the distal/lingual tissue, crosses the wound, penetrates the distal/lingual tissue, and is then tied off at the original entry point at the mesial/buccal non-working end. Since prolonged tension is expected when using this technique, it's prudent to use a longer-lasting resorbable or permanent suture.[5][10][11]
The continuous suture (Figure 5) is used when longer wounds are present, such as full mouth extractions. The continuous suture can be locking and non-locking. The advantage of the locking variation is that some security will remain if either knot unties. With the non-locking variation, if either knot comes untied, the flap is compromised, and the wound will likely dehisce. The advantage to the continuous suture is that it applies evenly distributed pressure across the entirety of the wound. Continuous sutures under tension can be reinforced with separate, simple horizontal mattress sutures.[11]
Clinical Significance
Successful outcomes when performing procedures such as dental implant placement, soft tissue grafting, bone harvesting, and grafting are dependent on the clinician's knowledge and familiarity with the basic suturing materials and techniques discussed in this paper. Post-surgical complications and infections have dramatically reduced with the innovations in suturing materials. Our responsibility as clinicians is to remain knowledgeable regarding suture innovation to continue providing the highest quality of care.[10]
Enhancing Healthcare Team Outcomes
Suturing is a foundational surgical skill that must be mastered to provide optimal outcomes for our patients. Unfortunately, there often is a lack of suturing guidance within the dental field. We can learn from our medical colleagues who frequently use silicone suturing molds in medical school and residency before suturing real human tissue. As dentoalveolar surgeons, we can utilize silicone training models to hone our skills and practice the basic knots and suturing methods previously discussed in the article. This enables us as clinicians to develop competency before suturing within a patient’s mouth. In addition, many suturing materials and instructions are available to those pursuing a surgical specialty or general practitioners desiring to perform more dentoalveolar surgery.[12]
A study where 38 medical students completed surveys regarding confidence before and after completing a suturing lab with silicone models unsurprisingly revealed that all students felt more comfortable with their suturing capabilities after performing the suturing labs. The study's goal was to perform a quantitative measure of the competence and confidence gained by the students.[12]
Practice on silicone models before live patients is not only optimal, but ethical. There are numerous resources to improve suturing competency. It is our responsibility as dental professionals to utilize the resources available and take the initiative to hone our suturing skills before performing dentoalveolar surgery on patients.[12]
Media
References
Byrne M, Aly A. The Surgical Suture. Aesthetic surgery journal. 2019 Mar 14:39(Suppl_2):S67-S72. doi: 10.1093/asj/sjz036. Epub [PubMed PMID: 30869751]
Burkhardt R, Lang NP. Influence of suturing on wound healing. Periodontology 2000. 2015 Jun:68(1):270-81. doi: 10.1111/prd.12078. Epub [PubMed PMID: 25867989]
Minozzi F, Bollero P, Unfer V, Dolci A, Galli M. The sutures in dentistry. European review for medical and pharmacological sciences. 2009 May-Jun:13(3):217-26 [PubMed PMID: 19673173]
Wang PH, Huang BS, Horng HC, Yeh CC, Chen YJ. Wound healing. Journal of the Chinese Medical Association : JCMA. 2018 Feb:81(2):94-101. doi: 10.1016/j.jcma.2017.11.002. Epub 2017 Nov 21 [PubMed PMID: 29169897]
Kurtzman GM, Silverstein LH, Shatz PC, Kurtzman D. Suturing for surgical success. Dentistry today. 2005 Oct:24(10):96-102; quiz 103 [PubMed PMID: 16277068]
O'Neal RB, Alleyn CD. Suture materials and techniques. Current opinion in periodontology. 1997:4():89-95 [PubMed PMID: 9655027]
Level 3 (low-level) evidenceRegula CG, Yag-Howard C. Suture Products and Techniques: What to Use, Where, and Why. Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al.]. 2015 Oct:41 Suppl 10():S187-200. doi: 10.1097/DSS.0000000000000492. Epub [PubMed PMID: 26418685]
Koyuncuoglu CZ, Yaman D, Kasnak G, Demirel K. Preference of Suture Specifications in a Selected Periodontal and Implant Surgeries in Turkey. European journal of dentistry. 2019 Feb:13(1):108-113. doi: 10.1055/s-0039-1688732. Epub 2019 Jun 6 [PubMed PMID: 31170760]
Torres-Lagares D, Barranco-Piedra S, Rodríguez-Caballero A, Serrera-Figallo MA, Segura-Egea JJ, Gutiérrez-Pérez JL. Suture needles in oral surgery: alterations depending on the type and number of sutures. Medicina oral, patologia oral y cirugia bucal. 2012 Jan 1:17(1):e129-34 [PubMed PMID: 22157669]
Silverstein LH, Kurtzman GM, Shatz PC. Suturing for optimal soft-tissue management. The Journal of oral implantology. 2009:35(2):82-90. doi: 10.1563/1548-1336-35.2.82. Epub [PubMed PMID: 19400063]
Brandt MT, Jenkins WS. Suturing principles for the dentoalveolar surgeon. Dental clinics of North America. 2012 Jan:56(1):281-303, xi. doi: 10.1016/j.cden.2011.08.004. Epub [PubMed PMID: 22117956]
Gallagher PO, Bishop N, Dubrowski A. Investigating the Perceived Efficacy of a Silicone Suturing Task Trainer Using Input from Novice Medical Trainees. Cureus. 2020 Jan 9:12(1):e6612. doi: 10.7759/cureus.6612. Epub 2020 Jan 9 [PubMed PMID: 32064192]