Introduction
Eyes that lack sufficient capsular support for intraocular lens (IOL) placement present a unique surgical challenge. Options for IOL placement include anterior chamber intraocular lenses (ACIOLs), iris-fixated posterior chamber intraocular lenses (PCIOLs), and scleral-fixated intraocular lenses (SFIOLs).[1] Effective use of these fixation techniques in the appropriate clinical setting has been described, without clear superiority of one method.
However, SFIOLs provide a better ocular safety profile than ACIOLs or iris fixated IOLs.[2] Placement of IOL in the sulcus region keeps the IOL closer to the natural anatomic position of the crystalline lens and is safer for the corneal endothelium and iris.[3]
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
In the technique of SFIOL, the optic of the IOL is placed in the posterior chamber. At the same time, the haptic is fixed to the sclera approximately 1.5 to 2 mm from the limbus, which is the external landmark for the ciliary sulcus. Placement of IOL in the sulcus region is considered safer for the corneal endothelium and iris.[3] Haptics are usually fixated in the horizontal direction at 3 and 9 o'clock direction. However, in cases with larger eyes, such as high myopia or Marfan syndrome, haptics can be fixated vertically at 6 and 12 o'clock. The vertical diameter of the cornea is less than the horizontal diameter.
Indications
Conditions in which in-the-bag PCIOL cannot be implanted include:
Subluxation/dislocation of the lens (ectopia lentis) – Causes of ectopia lentis include:
- Hereditary ectopia lentis without systemic manifestations - Simple ectopia lentis and ectopia lentis et papillae.
- Hereditary ectopia lentis with systemic associations - Marfan syndrome, Weill Marchesani syndrome, homocystinuria, hyperlysinemia, and sulfite oxidase deficiency.
- Acquired causes - Ocular trauma, high myopia, buphthalmos, anterior uveal tumors, inflammatory causes like chronic cyclitis and syphilis, and pseudoexfoliation syndrome
Inadequate capsular support - This is seen in cases of post-surgical aphakia due to intracapsular cataract extraction surgery or complications of cataract surgery such as bag dialysis, zonular dialysis, and large posterior capsular rupture.
Contraindications
Relative contraindications for the procedure include scleral thinning, scleritis, uveitis, advanced secondary glaucoma, corneal pathology, and any pre-existing retinal disorder. Management of these conditions should be considered before SFIOL.
Equipment
Equipment required includes a vitrectomy cutter, anterior chamber maintainer, microforceps, blades, crescents, appropriate IOL, and sutures according to the technique used, in addition to the usual equipment required in cataract surgery.
Preparation
Consent is taken from the patient, or parent/guardian in case of minors, after explaining the nature of the procedure and the possible complications of surgery.
Preoperative Evaluation
A detailed history, including ocular and systemic complaints and history of any previous treatment, is taken. If ectopia lentis is suspected due to any heritable disease such as Marfan syndrome or homocystinuria, a thorough systemic workup is done, and a necessary interprofessional opinion is warranted. A complete ophthalmological examination is performed, including uncorrected and best-corrected visual acuity, slit-lamp examination to assess the anterior segment, tonometry, keratometry, posterior segment evaluation, and ultrasound B scan if the posterior segment is not visible. The IOL power is calculated using appropriate formulas.
Anesthesia
Surgery is done under peribulbar block if the patient is cooperative or under general anesthesia if the patient is not cooperative or has other systemic issues.
Technique or Treatment
The surgical site is sterilized. Then phacoemulsification, phacoaspiration, or lensectomy is performed (whichever applies to the particular case), followed by anterior vitrectomy. This is followed by scleral fixation of IOL. In aphakic eyes, scleral fixation of IOL is performed directly.
SFIOL may be sutured or sutureless.
Sutured Scleral fixated IOL (SFIOL)
IOLs used for sutured scleral fixation include:
- Foldable acrylic IOLs with two eyelets on each side[4]
- Foldable acrylic IOLs with one eyelet on each side
- Rigid polymethyl methacrylate (PMMA) IOL with one eyelet on each side[5]
Sutures used for SFIOLs are 10-0 polypropylene, 9-0 polypropylene, 8-0 polypropylene and 8-0 polytetrafluoroethylene (PTFE).[4] The use of 10-0 polypropylene fixation sutures is less durable and may be associated with high suture breakage and degradation-related complications.[6] 9-0 and 8-0 polypropylene sutures have higher tensile strength, resulting in less suture breakage and degradation. The mechanism of polypropylene suture breakage has been attributed to both suture cutting by haptic positioning and degradation of the polypropylene material itself. PTFE suture has higher tensile strength than prolene and greater resilience, which decreases the risk of suture breakage in the long term.[7] Due to its white color and greater thickness, it has better visualization during surgery. In addition, it has a less inflammatory response due to its inert nature and easier manipulation due to minimal memory. The unique properties of this suture facilitate knot tying and enable softer knots to form. Frictionless sliding ensures precise placement of the knot. However, the thickness of the PTFE suture may cause difficulty in burying the suture after surgery.
A potential complication after all sutured SFIOL techniques is knot erosion through the conjunctiva after surgery. This can be associated with an increased risk of endophthalmitis.[8] To avoid this, knots can be covered with partial-thickness scleral flaps, buried in the sclera, or covered using corneoscleral pockets (Hoffman technique).
The points of fixation on the haptic can vary from two-point to four-point fixation. The two-point fixation method is more commonly used but is associated with an increased incidence of IOL tilt and decentration, which can induce high order spherical aberrations.[9] In contrast, the four-point fixation method has decreased the risk of IOL tilt and decentration.[10][11][12]
The techniques for sutured SFIOLs can broadly be classified into ab externo and ab interno techniques.[10][11] Endoscopy-assisted sutured scleral fixation of IOL has also been described.[13] Conjunctival peritomy is almost always required in sutured SFIOL, except when corneoscleral pockets are formed using the Hoffman technique.[14]
In the ab externo technique, two partial-thickness scleral flaps are made 180 degrees apart in horizontal meridian after conjunctival flap dissection. The long straight needle of the suture is passed underneath one flap 1 mm from the limbus, while a 27 gauge (G) needle is passed underneath the second flap. The long straight needle of the suture is then docked inside the 27 G needle within the anterior chamber of the eye. The needle of the suture is exteriorized through the opposite flap. The middle of the suture is pulled out from the corneal section and cut into two. Each end of this portion is tied to the eyelet of the haptics of the IOL. The IOL is then placed behind the iris in the posterior chamber. The suture ends at the scleral flap are tied to the sclera beneath the scleral flaps. Scleral flaps are reposited, and the corneoscleral wound and conjunctiva are sutured. In case of a four-point fixation, one more suture with a straight needle is passed in a similar fashion parallel to the first one and similarly cut and tied to the eyelet of haptics.
In the ab interno technique, after constructing two partial-thickness scleral flaps, the curved needle ends of a suture are passed through the corneoscleral incision under the iris. Then, each curved needle is passed through the scleral flap, aiming to emerge from the ciliary sulcus. The rest of the procedure is similar to ab externo: the part of the suture at the corneoscleral incision is cut, and the two ends are tied to each IOL haptic. The IOL is then placed behind the iris in the posterior chamber. Next, the suture ends at the scleral flap are tied, scleral flaps are reposited, and the conjunctival and corneoscleral wounds are sutured. The ab interno technique utilizes a blind maneuver, which is associated with unpredictable placement of haptics, and may lead to complications such as retinal detachment and hemorrhage. However, it is quicker than ab externo and easier to perform in cases of combined surgery with penetrating keratoplasty.
Endoscopy-assisted SFIOL has also been described. In this technique, the endoscope is inserted through the limbus or pars plana, enabling direct visualization of the ciliary sulcus. Thereafter, surgery can be done using a bimanual method or a one-handed method. In the bimanual method, the surgeon holds the endoscope with one hand, while the other hand is used to introduce the suture needle through the sclera, either through ab externo or ab interno technique. Conversely, in the one-handed method, the needle is attached by a silicone sleeve to the endoscopic probe and is passed through the sclera using the ab interno approach. An endoscope has the advantage of direct visualization of the ciliary sulcus and needle penetration site. In addition, it enables the removal of vitreous strands at the penetration site, allows exact positioning of haptics in the sulcus, and aids in the examination of the posterior segment.
Last but not least, in the Hoffmann technique of SFIOL, two scleral pockets are constructed 180 degrees apart through peripheral clear corneal incisions. A double-armed suture is passed through the scleral pocket and conjunctiva on each side using an ab interno or ab externo approach. After removing the needles, the suture ends are then retrieved with a hook through the corneal incision and tied. This method avoids the need for conjunctival dissection, sclera cauterization, or sutured wound closure. Thus, this method may have advantages in eyes with conjunctival scarring due to any cause and eyes which have undergone glaucoma filtration surgeries.
Sutureless Scleral Fixated IOL
Sutureless implantation retains the advantages of SFIOLs, whilst avoiding suture-related complications. There have been several modifications of sutureless techniques since their inception. They can be broadly categorized into two groups: techniques using scleral tunnel with scleral flaps and techniques using scleral tunnel without scleral flaps.
Techniques of Sutureless SFIOL Using Scleral Tunnel With Scleral Flaps
In the Scharioth technique, after performing a 25-gauge pars plana vitrectomy, the cannulas are plugged, and the eye is prepared for intrascleral haptic fixation. Two ab externo 23-gauge ciliary sulcus sclerotomies are created 1.5 to 2 mm from the limbus 180 degrees apart. Limbus parallel 23-gauge intrascleral Scharioth tunnels are created in a counterclockwise manner from the sclerotomies at 50% depth, exiting through the conjunctiva after 2 to 3 mm. Then, 25-gauge end-gripping forceps externalize the leading haptic, which is subsequently fed into the Scharioth tunnel. The same technique is repeated with the trailing haptic.[15]
Glued IOL is another technique of sutureless SFIOL with scleral flaps. In this procedure, two partial-thickness scleral flaps are made 180 degrees apart at 3 and 9 o’clock positions. Then, two ab externo sclerotomies are made under the scleral flaps 1.5 mm from the limbus using a 24 G needle. Scleral tunnels are made at the edge of the scleral flap near the sclerotomy sites with the help of a 26 G bent needle. A three-piece IOL is inserted through the main corneoscleral incision, and the leading haptic is externalized by micro forceps using a handshake technique. Similarly, the trailing haptic is externalized. Both haptics are tucked into their respective scleral tunnels. The area is dried, and fibrin glue is put under the sclera flaps. The flap is deposited, and pressure is applied for 10-20 seconds. Finally, the corneoscleral incision is closed, and the conjunctiva is sutured.[16] The glued IOL technique allows for precise centering of the IOL, as the length of the exteriorized haptic can be adjusted. It also allows the tilt of the IOL to be adjusted by altering the direction of the scleral tunnel.
This technique usually requires an assistant to secure the leading haptic while the trailing haptic is being exteriorized. However, a few alterations can be made to make the procedure less challenging. Narang et al. developed a no-assistant technique (NAT), which works on the principle of vector forces.[17] Once the leading haptic is externalized, the trailing haptic is flexed inside the eye. As it crosses the mid-pupillary plane close to the 6 o’clock position, vector forces act in a way that further extrudes the leading haptic, minimizing chances of slippage back into the eye. Beiko et al. described the use of silicone retainer tires from iris and capsular hooks to secure the leading haptic while the trailing haptic is being externalized.
A few other modifications to the glued IOL technique have been described. One modification involves the position of the initial scleral flaps. Partial-thickness scleral flaps are usually made at 3 and 9 o’clock positions if the white-to-white (WTW) distance is 11 mm or less. However, in certain cases, such as Marfan syndrome, the WTW distance may be 12 mm or more. In such conditions, to ensure that an adequate length of the haptics can be externalized, the flaps are made at 6 and 12 o’clock positions, as the vertical diameter of the cornea is less than the horizontal.
In another modification, the sclerostomy can be made 0.5 mm from the limbus instead of 1.5 mm. This shifts the IOL plane anteriorly, thereby allowing haptics to traverse a lesser distance and allowing greater haptic externalization. However, these modifications may be associated with their own set of complications, such as iridodialysis, intraoperative bleeding, and pigmentary disturbances. Some of these complications are preventable by doing a prior vitrector-assisted peripheral iridectomy.[17]
Recently a new design of the lens, also known as the Carlevale lens, has been described. It is a 13.2-mm-long single-piece hydrophilic acrylic IOL with a 6.5-mm-wide optic plate featuring T-shaped harpoons protruding off the closed haptics to allow self-anchoring on the sclera without the need for sutures. However, a scleral flap is needed to cover the harpoons.[18]
Techniques of Sutureless SFIOL Using Scleral Tunnel Without Scleral Flaps
Gabor and Pavlidis first popularized sutureless intrascleral haptic fixation using a 24 G needle to create sclerostomies and scleral tunnels adjacent to each other without creating scleral flaps.[19] The authors found that since the sclerotomy entry site and scleral tunnel were adjacent, it made tucking-in of haptics difficult.
Flanged Intrascleral Intraocular Lens Fixation with Double-Needle Technique.
Nowadays, a flapless, sutureless transconjunctival technique using a 30-gauge needle is very popular, also known as the Yamane technique.[20] A three-piece IOL is inserted into the anterior chamber using an injector, and the trailing haptic is kept outside to prevent the IOL from falling into the vitreous cavity. An angled sclerotomy is made through the conjunctiva 2 mm from the limbus using a 30-gauge needle with an ultra-thin wall. The leading haptic is threaded into the lumen of the needle using forceps. A second sclerotomy is then made with a second needle that is 180 degrees from the first sclerotomy. The trailing haptic is inserted into the lumen of the second needle. Then, both of the haptics are externalized onto the conjunctiva. The ends of the haptics are cauterized using an ophthalmic cautery device to make a flange with a diameter of 0.3 mm. The flange of the haptics is pushed back and fixed into the scleral tunnels.
Recently, Canabrava et al. have described a four-flanged intrascleral fixation of IOL. This technique utilizes 5-0 polypropylene sutures that are inserted through eyelets of the haptics of a single-piece non-foldable IOL. A flange is created at the ends of the suture at the eyelets using an ophthalmic cautery device. Another flange is created after the suture is externalized through the sclera on both sides.[21]
Complications
Although long term studies in patients with SFIOLs have generally been favorable, this surgery has its own set of complications, which include:
- Transient corneal edema
- Postoperative hypotony
- Ocular hypertension
- Cystoid macular edema
- IOL dislocation[22]
- IOL tilt and resultant astigmatism[23]
- Pupillary capture of IOL
- Pseudophacodonesis
- Suprachoroidal or vitreous hemorrhage[23]
- Retinal detachment, especially in patients with high myopia and Marfan syndrome
- Endophthalmitis[8]
In addition, transscleral knot erosion through sclera and suture breakage in sutured SFIOL and haptic erosion and haptic dislodgement in the sutureless SFIOL may occur.
Clinical Significance
Whenever in the bag PCIOL can not be implanted, SFIOLs provide a better ocular safety profile than ACIOLs or iris fixated IOLs. IOL is implanted in the sulcus region which is closer to the natural anatomic position of the crystalline lens and is safer for the corneal endothelium and iris.
Enhancing Healthcare Team Outcomes
An anterior segment surgeon generally does SFIOL surgery. However, in cases with posterior segment complications such as macular edema and retinal detachment, a retinal surgeon should be involved in management. Optometrists play a critical role in ascertaining if a high degree of astigmatism or refractive error is present after surgery, which leads to the diagnosis and management of complications such as IOL tilt and dislocation. In addition, a thorough systemic evaluation by an interprofessional team such as the general physician, pediatrician, and cardiologist is necessary if a syndromic cause for ectopia lentis is suspected, leading to better patient care and enhanced outcomes.
Media
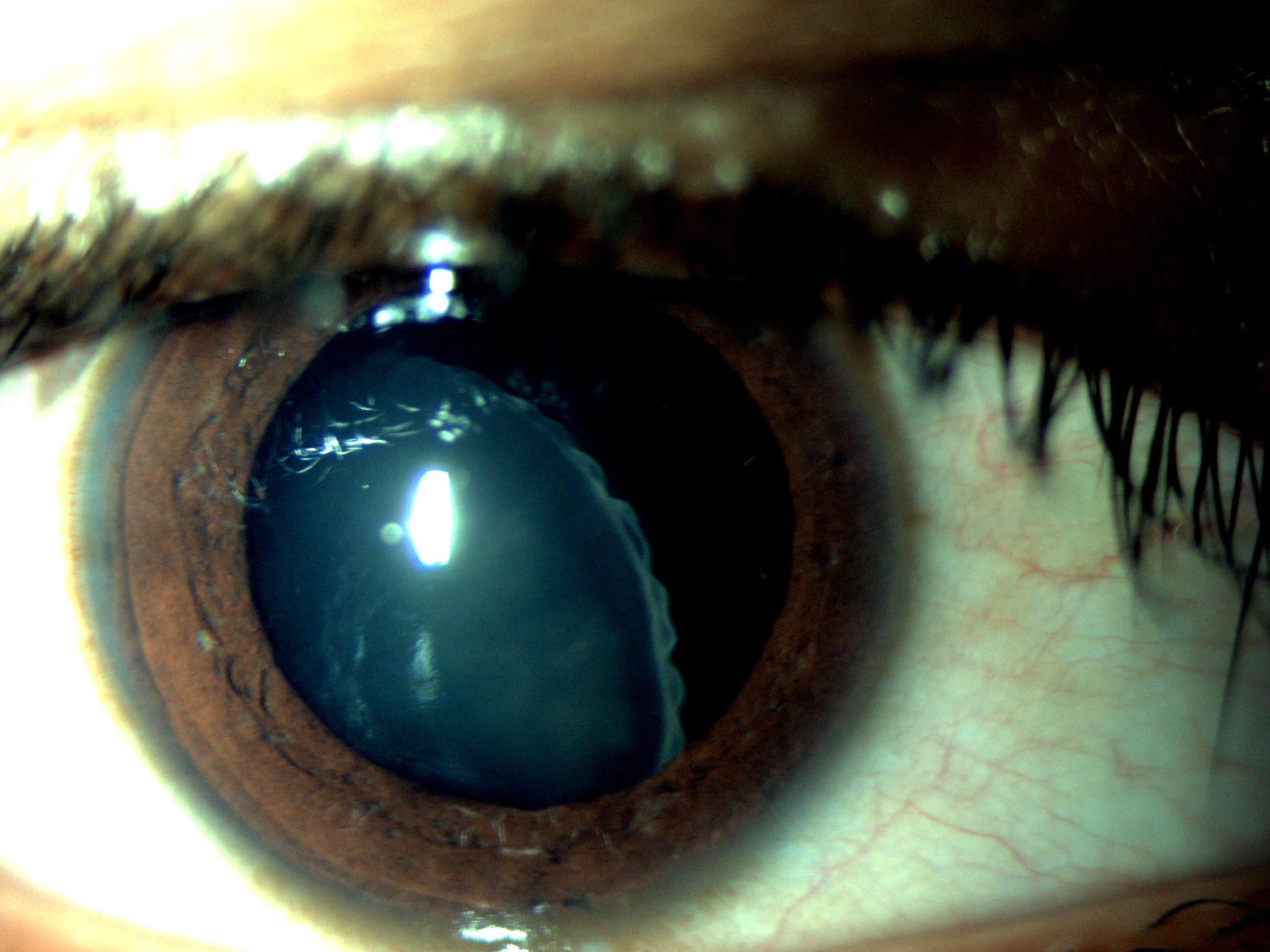
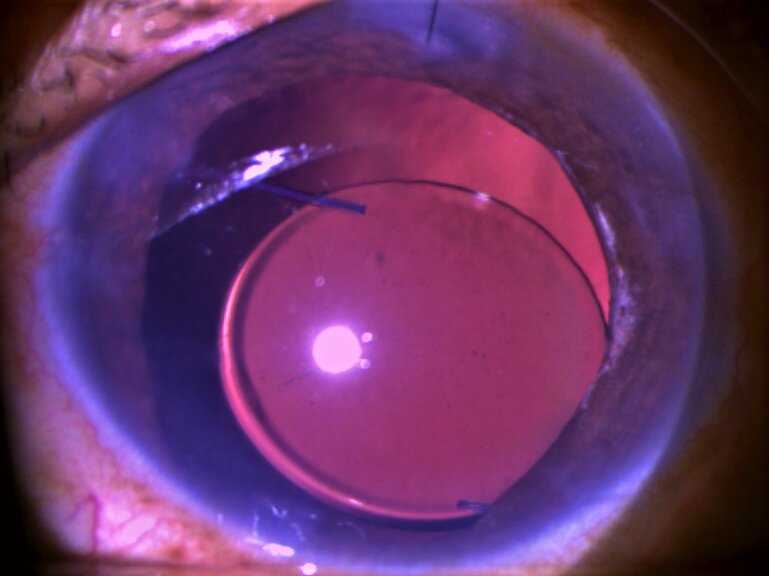
(Click Image to Enlarge)
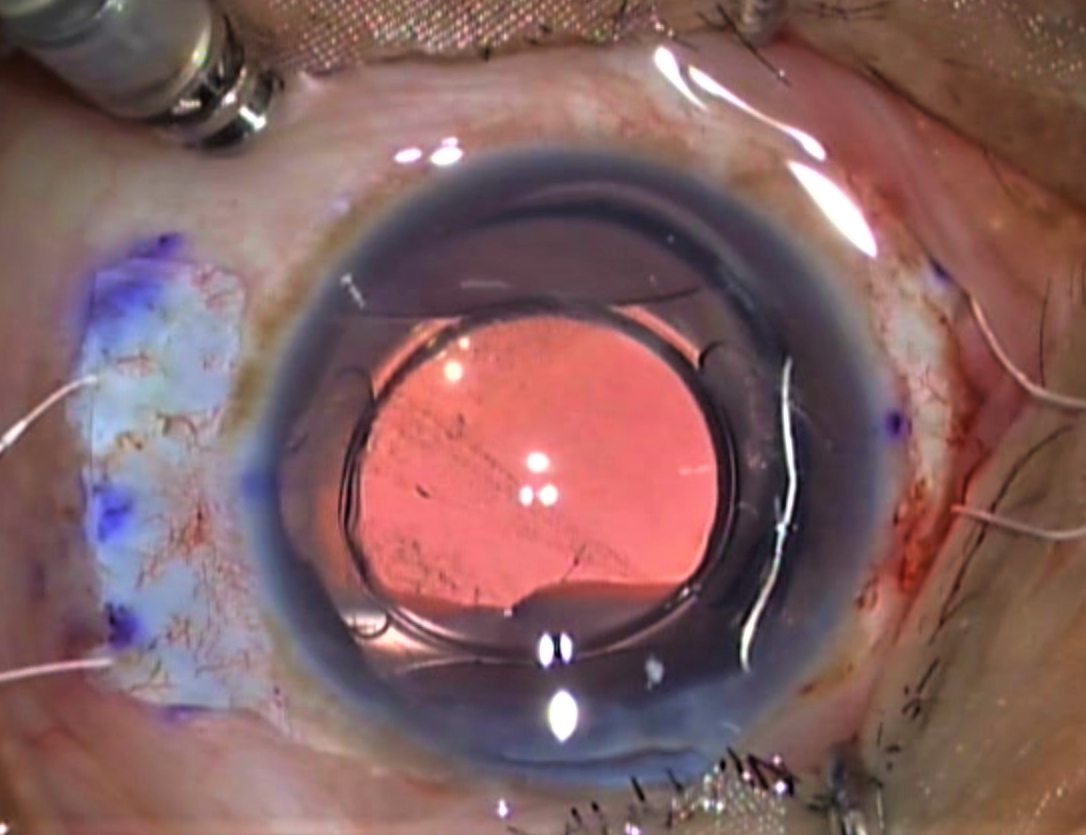
(Click Image to Enlarge)
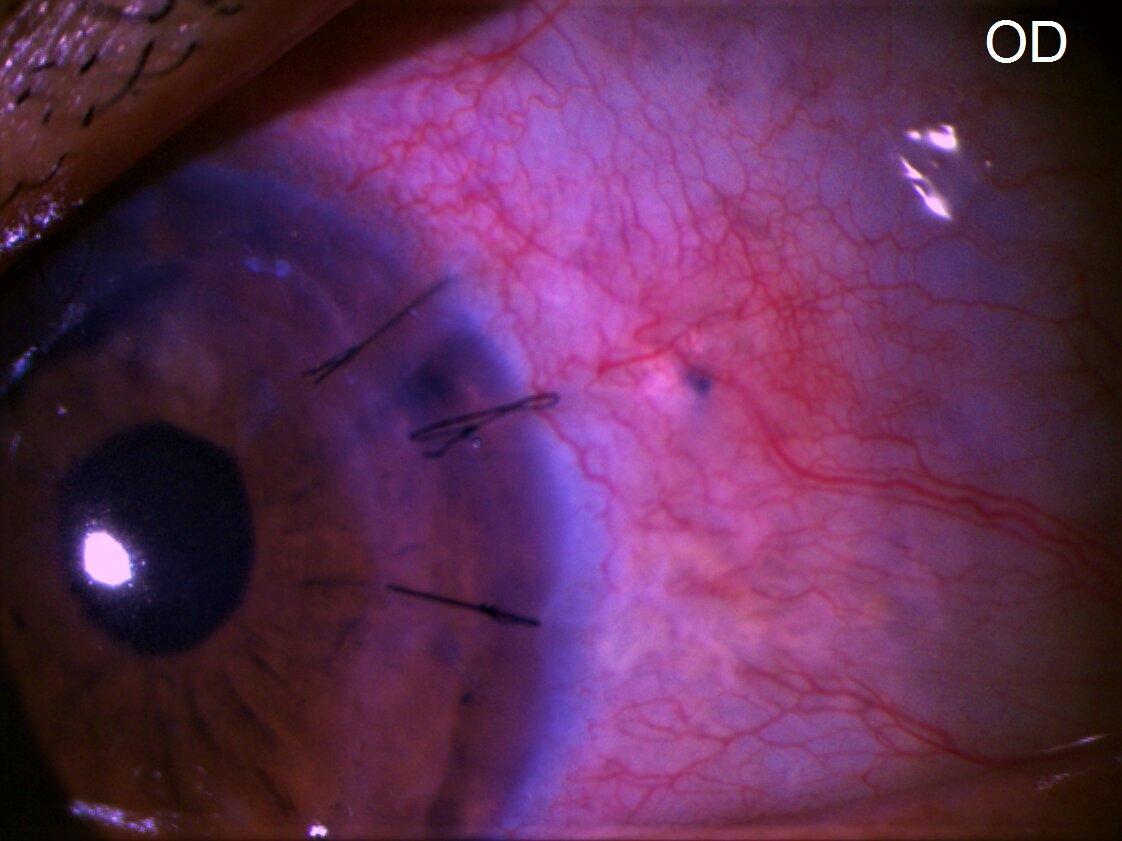
(Click Image to Enlarge)
References
Holt DG, Young J, Stagg B, Ambati BK. Anterior chamber intraocular lens, sutured posterior chamber intraocular lens, or glued intraocular lens: where do we stand? Current opinion in ophthalmology. 2012 Jan:23(1):62-7. doi: 10.1097/ICU.0b013e32834cd5e5. Epub [PubMed PMID: 22081029]
Level 3 (low-level) evidenceChan TC, Lam JK, Jhanji V, Li EY. Comparison of outcomes of primary anterior chamber versus secondary scleral-fixated intraocular lens implantation in complicated cataract surgeries. American journal of ophthalmology. 2015 Feb:159(2):221-6.e2. doi: 10.1016/j.ajo.2014.10.016. Epub 2014 Oct 22 [PubMed PMID: 25448990]
Level 2 (mid-level) evidenceHannush SB. Sutured posterior chamber intraocular lenses: indications and procedure. Current opinion in ophthalmology. 2000 Aug:11(4):233-40 [PubMed PMID: 10977767]
Level 3 (low-level) evidenceKhan MA, Gupta OP, Smith RG, Ayres BD, Raber IM, Bailey RS, Hsu J, Spirn MJ. Scleral fixation of intraocular lenses using Gore-Tex suture: clinical outcomes and safety profile. The British journal of ophthalmology. 2016 May:100(5):638-43. doi: 10.1136/bjophthalmol-2015-306839. Epub 2015 Aug 28 [PubMed PMID: 26319945]
Level 2 (mid-level) evidenceSindal MD, Nakhwa CP, Sengupta S. Comparison of sutured versus sutureless scleral-fixated intraocular lenses. Journal of cataract and refractive surgery. 2016 Jan:42(1):27-34. doi: 10.1016/j.jcrs.2015.09.019. Epub [PubMed PMID: 26948775]
Price MO, Price FW Jr, Werner L, Berlie C, Mamalis N. Late dislocation of scleral-sutured posterior chamber intraocular lenses. Journal of cataract and refractive surgery. 2005 Jul:31(7):1320-6 [PubMed PMID: 16105601]
Level 2 (mid-level) evidenceKhan MA, Gerstenblith AT, Dollin ML, Gupta OP, Spirn MJ. Scleral fixation of posterior chamber intraocular lenses using gore-tex suture with concurrent 23-gauge pars plana vitrectomy. Retina (Philadelphia, Pa.). 2014 Jul:34(7):1477-80. doi: 10.1097/IAE.0000000000000233. Epub [PubMed PMID: 24949717]
Schechter RJ. Suture-wick endophthalmitis with sutured posterior chamber intraocular lenses. Journal of cataract and refractive surgery. 1990 Nov:16(6):755-6 [PubMed PMID: 2258814]
Level 3 (low-level) evidenceTsai YY, Tseng SH. Transscleral fixation of foldable intraocular lens after pars plana lensectomy in eyes with a subluxated lens. Journal of cataract and refractive surgery. 1999 May:25(5):722-4 [PubMed PMID: 10330654]
Level 3 (low-level) evidenceGüell JL, Barrera A, Manero F. A review of suturing techniques for posterior chamber lenses. Current opinion in ophthalmology. 2004 Feb:15(1):44-50 [PubMed PMID: 14743019]
Level 3 (low-level) evidencePor YM, Lavin MJ. Techniques of intraocular lens suspension in the absence of capsular/zonular support. Survey of ophthalmology. 2005 Sep-Oct:50(5):429-62 [PubMed PMID: 16139038]
Level 3 (low-level) evidenceChakrabarti A, Gandhi RK, Chakrabarti M. Ab externo 4-point scleral fixation of posterior chamber intraocular lenses. Journal of cataract and refractive surgery. 1999 Mar:25(3):420-6 [PubMed PMID: 10079450]
Level 2 (mid-level) evidenceSasahara M, Kiryu J, Yoshimura N. Endoscope-assisted transscleral suture fixation to reduce the incidence of intraocular lens dislocation. Journal of cataract and refractive surgery. 2005 Sep:31(9):1777-80 [PubMed PMID: 16246783]
Level 2 (mid-level) evidenceHoffman RS, Fine IH, Packer M. Scleral fixation without conjunctival dissection. Journal of cataract and refractive surgery. 2006 Nov:32(11):1907-12 [PubMed PMID: 17081894]
Vote BJ,Tranos P,Bunce C,Charteris DG,Da Cruz L, Long-term outcome of combined pars plana vitrectomy and scleral fixated sutured posterior chamber intraocular lens implantation. American journal of ophthalmology. 2006 Feb; [PubMed PMID: 16458685]
Level 2 (mid-level) evidenceKumar DA, Agarwal A, Prakash D, Prakash G, Jacob S, Agarwal A. Glued intrascleral fixation of posterior chamber intraocular lens in children. American journal of ophthalmology. 2012 Apr:153(4):594-601, 601.e1-2. doi: 10.1016/j.ajo.2011.09.027. Epub 2012 Jan 20 [PubMed PMID: 22264692]
Level 2 (mid-level) evidenceNarang P, Agarwal A. Glued intrascleral haptic fixation of an intraocular lens. Indian journal of ophthalmology. 2017 Dec:65(12):1370-1380. doi: 10.4103/ijo.IJO_643_17. Epub [PubMed PMID: 29208817]
Rossi T, Iannetta D, Romano V, Carlevale C, Forlini M, Telani S, Imburgia A, Mularoni A, Fontana L, Ripandelli G. A novel intraocular lens designed for sutureless scleral fixation: surgical series. Graefe's archive for clinical and experimental ophthalmology = Albrecht von Graefes Archiv fur klinische und experimentelle Ophthalmologie. 2021 Jan:259(1):257-262. doi: 10.1007/s00417-020-04789-3. Epub 2020 Jun 11 [PubMed PMID: 32529278]
Gabor SG, Pavlidis MM. Sutureless intrascleral posterior chamber intraocular lens fixation. Journal of cataract and refractive surgery. 2007 Nov:33(11):1851-4 [PubMed PMID: 17964387]
Yamane S, Sato S, Maruyama-Inoue M, Kadonosono K. Flanged Intrascleral Intraocular Lens Fixation with Double-Needle Technique. Ophthalmology. 2017 Aug:124(8):1136-1142. doi: 10.1016/j.ophtha.2017.03.036. Epub 2017 Apr 27 [PubMed PMID: 28457613]
Canabrava S, Canêdo Domingos Lima AC, Ribeiro G. Four-Flanged Intrascleral Intraocular Lens Fixation Technique: No Flaps, No Knots, No Glue. Cornea. 2020 Apr:39(4):527-528. doi: 10.1097/ICO.0000000000002185. Epub [PubMed PMID: 31658168]
Chan CK. An improved technique for management of dislocated posterior chamber implants. Ophthalmology. 1992 Jan:99(1):51-7 [PubMed PMID: 1741140]
Level 3 (low-level) evidencePrice FW Jr, Whitson WE. Suprachoroidal hemorrhage after placement of a scleral-fixated lens. Journal of cataract and refractive surgery. 1990 Jul:16(4):514-5 [PubMed PMID: 2199668]
Level 3 (low-level) evidence