Introduction
The iris is a light-transmitting diaphragm that controls the amount of light entering the pupil inside the eye.[1] Iris is also responsible for maintaining the size and diameter of the pupil.[2] It also helps achieve a good quality of vision by reducing the aberrations from the lens and cornea by decreasing the amount of light entering the pupil, preventing excessive glare, and enhancing the depth of focus.[3] Traumatic injuries to the iris may result in glare, photophobia, reduced cosmesis, and contrast sensitivity.[4]
In 1917, Key first addressed his efforts over iris reconstruction by repairing an iridodialysis. He sutured the iris to the adjacent sclera. Emmerich initially put forward the concept of iris to iris repair in 1957. Due to a lack of infrastructures like microscopes and instruments, these techniques took time to gain a wider acceptance. Traumatic iris damage can be sphincter tear, iris chaffing, tear at the root of the iris, iridodialysis, iris transillumination defects, and aniridia. Various non-surgical and surgical approaches have been proposed to manage iris reconstruction, which is discussed further in this activity.[5]
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
The human iris consists of two main parts, the anterior stromal part and the posterior double-layered pigmented epithelium. The muscular part of the iris is defined by the iris dilator muscle and the sphincter pupillae muscle. The muscles are sandwiched between the anterior and posterior layers.[6]
The stromal layer consists of stromal cells, melanocytes, and fibrocytes. These cells have large intercellular spaces in between them. These gaps consist of collagen fibers, ground matrix, and aqueous humor. Multiple crypts are present in the stroma, which allow smooth passage of aqueous humor in the anterior chamber. The stroma has loose layers of melanocytes, connective tissue matrix, and blood vessels. Hyaluronic acid is the primary component of connective tissue that takes part in stroma formation and provides elasticity during surgical interventions.[7]
The posterior layer is continuous, with the sphincter muscle ring, pigmented epithelium, and myofibrils of dilator pupillae. The dilator pupillae muscle is thickest at the iris root insertion and thins out as it goes out towards the periphery at the pupillary edge. The traumatic and iatrogenic iris wounds don't heal on their own. When an iridotomy is performed, a defect is created, and there is no support for stromal and pigment cells and even fibroblasts to migrate and bridge the defect. As a result, no fibrosis or scarring takes place.[8]
Previous studies have revealed that healing in iris defects occurs adjacent to a suture only. At the suturing site, scarring occurs with infiltration by fibroblasts, plasma cells, and macrophages with minimal collagen. The presence of a suture governs the long-term strength of the iris defect. The iris defect's closure occurs by forming a cyclitic membrane due to a fibrinoid reaction. The vascular supply of the iris is divided into the major arterial arcade and the minor arterial arcade. The major arterial circle supplies the front portion of the ciliary body, and a minor arterial circle supplies the iris stroma. This vascular supply is the main cause of hyphema during traumatic injuries to the iris.[9]
Indications
- Penetrating injuries - Foreign body, Open globe Injuries, Iatrogenic surgical trauma, traumatic mydriasis[10]
- Blunt trauma - Iridodialysis, traumatic mydriasis
- Genetic defects - Iridocorneal endothelial syndrome, Axenfeld-Reigler syndrome iris coloboma
- Peripherical iridectomy - Surgical during uveitic cases, trabeculectomy, cataract extraction, penetrating keratoplasty, therapeutic keratoplasty, and while putting implantable Collamer lenses (ICL).
- Laser peripheral iridotomy for primary angle-closure glaucoma, primary angle-closure suspect, primary angle-closure, acute angle-closure glaucoma, and pupillary block glaucoma.
- Blunt ocular trauma is primarily responsible for iridodialysis, but it may also be present with penetrating injuries.
- Idiopathic floppy iris syndrome - Iris bellowing, prolapse, iridodialysis, and chaffing
- Pseudoexfoliation – Iridodialysis
- The old history of uveitis - Iridodialysis
- Trauma induced glare, monocular diplopia, and photophobia
- Cosmetic concern - Rare
- Release of peripheral anterior synechiae may lead to iridodialysis in an old penetrating keratoplasty case.[11]
Contraindications
- The traumatic defect in the iris is not causing any significant effect on vision
- While repairing an open globe injury with a corneal tear, iridodialysis, and lens removal, reconstruction of the iris is not the priority compared to injury to other parts
- The patient doesn't aspire for an iris repair, and it's not making any difference to the patient
- Limited intraocular visibility due to hyphema
- Iris prolapse with necrotic tissue for more than 24 hours
- Iris prolapse with signs of endophthalmitis
- Superior iridodialysis where the lid is protecting from photophobia[12]
Equipment
- Angle suture tying forceps[13][14]
- Anterior chamber maintainer (Lewicki)[15]
- Kuglen hook
- Sinskey hook
- Suture holding forceps[16]
- Micrograsping forceps (MST or Alcon)
- Prolene suture 10-0[17]
- 13 mm CIF-4 needles- with tapered body and sharp cutting tip
- CTC-6L needle[18]
- Monofilament polypropylene suture- smooth, limited memory and prevent degradation
Preparation
Slit-Lamp Evaluation
A thorough slit lamp evaluation should be performed before pupillary dilation. In an open globe injury with concomitant corneal and iris injury, the corneal tear should be repaired first to have a water-tight closure for performing iris manipulations. After corneal tear repair, a thorough evaluation is necessary to assess the extent of iridodialysis, iris tears, lens injury, and associated vitreous or retinal damage. The cornea should also be examined for sensation, TBUT, staining, dry eye assessment, presence and absence of guttae.
A thorough retinal evaluation is a must before attempting traumatic iris repair. The presence of iris atrophy, peripheral anterior or posterior synechiae, transillumination defects, and the presence or absence of pseudo-exfoliative material should be noted. The pupillary margin should be assessed for atrophy, persistent pupillary membranes, new vessels, sphincter tear, and ectropion uvea. If there is a traumatic cataract, the lens must be removed, and a decision on PCIOL or SFIOL can be made in the primary sitting or as a secondary procedure.
It is mandatory to perform a thorough contralateral eye assessment. If there is aphakia, the capsular support must be determined after full dilatation. In the case of pseudophakia, the stability and type of IOL must be noted.
Gonioscopy
A gonioscopy should be performed to rule out any neovascularization of angles, angle recession glaucoma, the extent of iridodialysis, presence of pigments, and peripheral anterior synechiae.[19]
Imaging
When slit lamp examination is not possible or inconclusive, anterior segment optical coherence tomography (ASOCT) or ultrasound biomicroscopy (UBM) to assess the angle of the anterior chamber, the thickness of iris, and posterior chamber details.[20]
X-ray, CT, and MRI
An anterior-posterior and lateral view X-ray is indicated in occult impacted foreign bodies in the skull and orbital area. CT and MRI are indicated in bony deformities and soft tissue injuries, respectively, and suspected foreign bodies. In the case of metallic foreign bodies, MRI is contraindicated.[21]
Pre-Operative Preparation
- The iris repair should be performed in an aphakic or pseudophakic eye as there is a high risk of lens capsule injury during the suture bites.
- The peribulbar or the retrobulbar block is preferred to perform the iris repair.
- Pilocarpine should be used to constrict the pupil.
- Centripetal pulling of the iris by mechanical force will help in loosening the tone of the iris and prepare it for suturing.
- The prolapsed vitreous, if any on the anterior or posterior surface of the pupil and iris, must be removed before any surgical manipulations. A manual vitrectomy will be enough in such scenarios. It is necessary to do a vitreous cut to prevent retinal tears or detachments.
- Liberal viscoelastic use is recommended to safeguard the endothelium, and viscoelastic should be pushed in the sulcus to push the iris upwards to facilitate easy passage of suture. The anterior chamber maintainer and pars plana infusion can also be used in eyes that have undergone vitrectomy.
- The needle can be docked to a 25 gauge cannula as it enters and exits the anterior chamber. This will prevent damage to the Descemet membrane.[22]
Technique or Treatment
Non-Surgical Approaches
The non-surgical techniques include contact lenses and tattooing.
Not all traumatic iris reconstructions require surgical management and can be managed non-surgically. Non-surgical management options are broadly divided into miotics like pilocarpine, brimonidine, carbachol, and contact lenses.[23]
Pilocarpine
The drug has a minimal effect on the peripheral iris. Pilocarpine has no or minimal action when there is traumatic mydriasis and pupillary sphincter tear. For the sphincter muscle to act, it should pull against another structure. In this scenario, it's the pupillary opening, but when the area of a pupil is damaged, it cannot constrict. In mild cases, pilocarpine has a good amount of role to play.[24]
Brimonidine
It is an alpha two agonist. It induces temporary pupillary constriction, especially in reflective surgery cases when the patient complains of halos in a dilated pupil during the nighttime.[25]
Contact Lenses
Contact lenses can be another treatment option for patients with traumatic iridodialysis, aniridia, and partial iris tissue loss. Special lenses are available for patients with a central clear pupillary zone and peripheral opaque margin. The pupillary diameter can also be customized to get a pinhole effect to reduce glare and photophobia. The commonly employed lenses are soft and rigid gas permeable lenses having a bigger diameter. Gas permeability is another factor that has a role in determining the success of contact lenses.[26]
Surgical Approaches
Corneal Tattooing
This technique is primarily used to treat corneal opacities for cosmesis. India ink, carbon particle, gold, or platinum chloride are embedded in the anterior to mid stroma by the corneal stromal puncture. The same technique can be used to hide an iridectomy or an area of iridodialysis to improve cosmesis and reduce symptoms of glare, photophobia, and monocular diplopia. The technique is often repeated after a few months as the tattooing wipes off to improve the color and density of the pigment. One drawback of this technique is that pigment may become plaque stuck on the surface.
Laser Iridoplasty
Argon laser iridoplasty was first used in 1958 to treat several ocular surface diseases. Cleasby first defined its use for altering the shape, size, and pupillary position whenever there is pupillary miosis, cyclitic membrane, and eccentric or ectopic pupil. Laser spots can be applied at the pupil margin or targeted on the collarette, resulting in functional sphincter destruction. Wise described another technique in 1985 by performing a straight incision sphincterotomy with the help of an argon laser. Less laser energy is necessary in these cases. A total of 0.02 seconds, 50-micrometer spot size, and 800-1500 milliwatt parameters are needed to cut the iris sphincter in parallel radial lines. This technique is helpful when laser spots are applied to the superficial stroma. For deep stroma, the laser exposure time has to be reduced to 0.01 seconds to prevent collateral damage and damage to the lens.[27]
Iridopexy
Suturing Iris Defects
Small Iris Defect
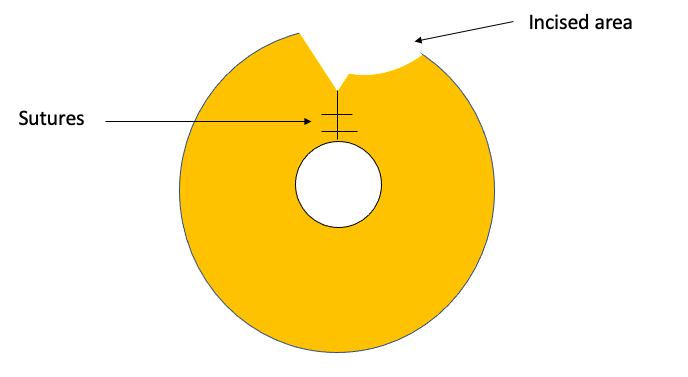
The iris defects in the form of a small coloboma can be sutured together by bringing the margins together and applying full-thickness sutures through the iris sphincter. The first suture should be close to the edge to prevent tenting of the iris and the other in the sphincter. If the coloboma involves the root of the iris, then additional sutures will be required.
Large Iris Defect
The large iris defects that involve the iris root may pose difficulty in repair. The circumferential incisional technique is used for large colobomas. Surgical iridectomy can be closed by one or two closely applied sutures at the pupillary margin. If the peripheral pupillary margins are taut and it's challenging to pull them apart, small sphincterotomies will be needed so that the iris tissue can be pulled and the defect can be closed with sutures. If sphincterotomies are not performed, it will result in the untoward pulling of the iris, resulting in cheese wiring of the suture and creating additional iris defects. An additional circumferential incision at the iris root will help pull the iris easily. Another technique of repair is the rotational flap technique. In this, the pupillary margins of the coloboma are clubbed together, leaving a remaining eyebrow-shaped portion in the periphery. Thick capsular remnants can also be used to close the gap providing more stability.[28]
Closed Globe, Single Armed, Peripheral Approach
McCannel Technique
In this technique, two paracenteses are made at the limbus perpendicular to the iris defect. A long thin needle with 10-0 polypropylene suture is first passed through the paracentesis, taking both the iris bite at the edge. The same needle is taken out through the paracentesis. The viscoelastic is instilled in the anterior chamber to maneuver inside the chamber, and viscoelastic can be injected below the iris. The uveal tissue will nudge upwards and help in easy passage of suture. A full-thickness stab incision is made at the peripheral corneoscleral junction between the two paracentesis sites. A sinskey or a Kuglen hook can be passed through the stab incision. Both the sutures can be brought out, tied, and cut. The technique is repeated multiple times till the iris defect closes.[29]
Shin's Technique
This was a modification of McCannel's technique. Shin utilized a 1.6 cm 25- gauge hypodermic needle clubbed to a tuberculin syringe. This needle is passed from the end of the paracentesis, and then it pierces the iris wound margin from anterior to posterior on both proximal and distal ends. The needle is taken out from the opposite end. The 25 gauge needle is then removed, and the 10-0 polypropylene suture is then extracted through the stab incision with the help of sinskey or Kuglen hook. The suture's ends are then tied, cut, and then buried.[30]
Modified Siepser Slipknot Technique
This technique further modified the McCannel technique by using two paracenteses and a slipknot. The 10-0 propylene suture is passed through the paracentesis, and a large peripheral suture is left at either end. The peripheral loop is grasped with the Kuglen hook or a sinskey hook and brought through the opposite paracentesis bypassing the anterior chamber. A double-throw slipknot is then performed, and both the suture are extracted outwards, pulling then knots back into the anterior chamber and opposing the iris tissue at the edges. Another knot is taken similarly. Finally, the suture ends are trimmed, and the same technique is repeated till the iris defect is closed.[31]
Closed-Globe, Double-Armed, Peripheral Approach
Pallin's Technique
The iris defect can be closed by a single limbal incision by using a double-armed peripheral approach. In this technique, a stab incision is made in the clear cornea adjacent to the iris defect. The needle with a 10-0 polypropylene suture from the stab incision is passed through the iris and brought out the respective paracentesis. The sutures then can be looped with the help of a sinskey or a Kuglen hook and brought out through the stab incision. Both the ends can be cut and tied together. This technique can be repeated till the iris defect closes.[32]
Lasso Technique
This is a technique done by using a lasso suture; it is used primarily for traumatic mydriasis or sluggish pupils using the three-port entry technique. A total of 3 limbal or clear corneal stab entries are fashioned at 1, 5, and 9 o clock. Viscoelastic is injected in the anterior chamber, and a 10-0 polypropylene suture is inserted through a nine o clock. A forceps commonly used to grasp epiretinal membrane is used to hold the iris tissue inserted from 10 o clock. The first iris bite is at the peripheral pupillary edge. This process is repeated till a continuous row of 3-4 suture bites are taken in the inferior iris at five o clock. A loop is formed from 1 to 5 o clock, then 1 to 9 o clock. In this way, three loops are formed at 1, 5, and 9 o clock, and the suture tension can then be adjusted for the required pupillary size before applying the final knot.[33]
Iridopexy
A small iridodialysis can usually be observed unless it causes troublesome glare, diplopia, or photophobia. A single stay suture is usually enough for symptomatic treatment when a repair is required. Large defect closure will require additional sutures for cosmetic and visual indications. Sometimes refixation of the iris at two points is needed. In case of vitreous prolapse, a prior vitrectomy is required before iridodialysis repair.
Closed-Globe, Single-Armed, Cross-Pupillary Approach
In this technique, a 17 mm straight needle with a 10-0 polypropylene suture is used. A paracentesis is made 180 degrees away from the iridodialysis site. Along with the suture, the needle is passed from the torn iris and brought out from the sclera near the area of normal iris insertion. Similarly, a second paracentesis is fashioned just above the suture exit area. A sinskey or an iris hook can then bring the other end of the suture out. The suture ends are adequately tightened, knots are buried, and flaps are closed. Additional flaps may be needed if an extensive repair is necessary.[34]
Bardak Modification
Bardak modified the above technique by using a 22 mm, 26 G hypodermic needle having a 9-0 or 10-0 polypropylene suture. Similarly, an MVR blade can be used having a hole of 0.4-0.6 mm at the tip.[35]
Closed-Globe, Double-Armed, Cross-Pupillary Approach
In this technique, a peritomy is fashioned in the zone of iridodialysis, and paracentesis is performed 180 degrees away. The same 17 mm needle with 10-0 polypropylene suture is used. First, the needle is passed from the paracentesis. The iris bite is taken in the iridodialysis area and brought out from the opposite end from the sclera at a distance of 1-1.25 mm away from the surgical limbus. The second end of the suture is passed from the same paracentesis engaging the torn iris approximately 1-1.5 mm lateral to the initial suture. The two suture ends are tied, and knots are buried then. Alternatively, the needles can be brought out through the old groove, and knots are tied and cut short.
Closed-Globe, Single-Armed, Peripheral Approach
McCannel Technique
This is another closed system approach. A peritomy is first created in the area of iridodialysis. A required number of 1mm scleral pockets are made 1 mm behind the limbus in the area of iridodialysis. 10-0 polypropylene sutures are passed from the scleral incision, iris bite is taken, and the needle is brought out from the cornea or another scleral pocket. A Sinskey, Kuglen, or iris hook is used to retrieve the suture end. The suture ends are then tied to themselves at the scleral edge. This process can be repeated till the iris defects close.[36]
Open-Globe Peripheral Approach
In this technique, a full-thickness scleral pocket is fashioned in the area of iridodialysis. The forceps are used to hold the iris bring it close to the wound margin, and then suture it to the sclera. This technique has a few disadvantages: large wound size, open globe approach, unstable wound, and high incidence of astigmatism.
Single Four-Throw (SFT) Pupilloplasty
In this technique, a single suture loop is taken to close the defect. Dr. Amar Agarwal first described this technique. In this, four times, the suture is wrapped around the angle ties and attached to the proximal suture. The two ends are then tied together, and the knot is then advanced in the AC and attached to the iris. The suture ends are then cut. Creating a second loop is not needed as the knot is self-retaining. In this way, this suture can be wrapped around itself four times to make a self-retaining knot.[37]
Intraocular Prostheses
Choyce proposed the first colored diaphragm anterior chamber intraocular lens in 1959. Later Sundmacher introduced posterior chamber black diaphragm lenses. The lenses were indicated in patients with congenital or acquired aniridia, albinism cases, and traumatic mydriasis. These lenses are available in various diameters and apertures.
Complications
- Corneal edema
- Corneal decompensation
- Descemet membrane detachment
- Hemorrhage
- Hyphema
- Secondary glaucoma
- Iridodilaysis
- Peripheral anterior synechiae
- Posterior synechiae
- Post-operative uveitis
- Endophthalmitis
- Vitreous loss
- Vitreous prolapse
- Vitreous touch syndrome
- Vitreous wick syndrome
- Cystoid macular edema
- IOL tilt or decentration
- IOL subluxation
- IOL dislocation
- Retinal detachment
Clinical Significance
Several innovations and advances have taken place in traumatic iris reconstruction. The treating ophthalmologist should also consider the non-surgical management options like miotics and contact lenses. Traumatic iris reconstruction is an area of innovation, and recently, many crucial innovative management techniques have been described. The surgeon's expertise in managing iridodialysis benefits the patient by reducing diplopia, photophobia, glare, and preserving visual acuity.[38]
Enhancing Healthcare Team Outcomes
Ophthalmologists should meticulously evaluate any case of trauma to the iris. The ophthalmologists should be aware of various non-surgical and surgical management options for iris repair. If an extensive iridodialysis repair is needed, the patient should be referred to a cataract or cornea surgeon well-versed in complex anterior segment surgical repair. The assisting nurses have a crucial role in the surgical operation theater, counseling, and post-operative management of the patient. The pharmacist plays a vital role in arranging the required drugs. In case of associated retinal trauma, the retinal surgeon also plays a crucial role in managing retinal tear, detachment, vitreous hemorrhage, nucleus, or IOL drop. The interprofessional healthcare team approach helps achieve a perfect outcome in these cases.[39]
Media
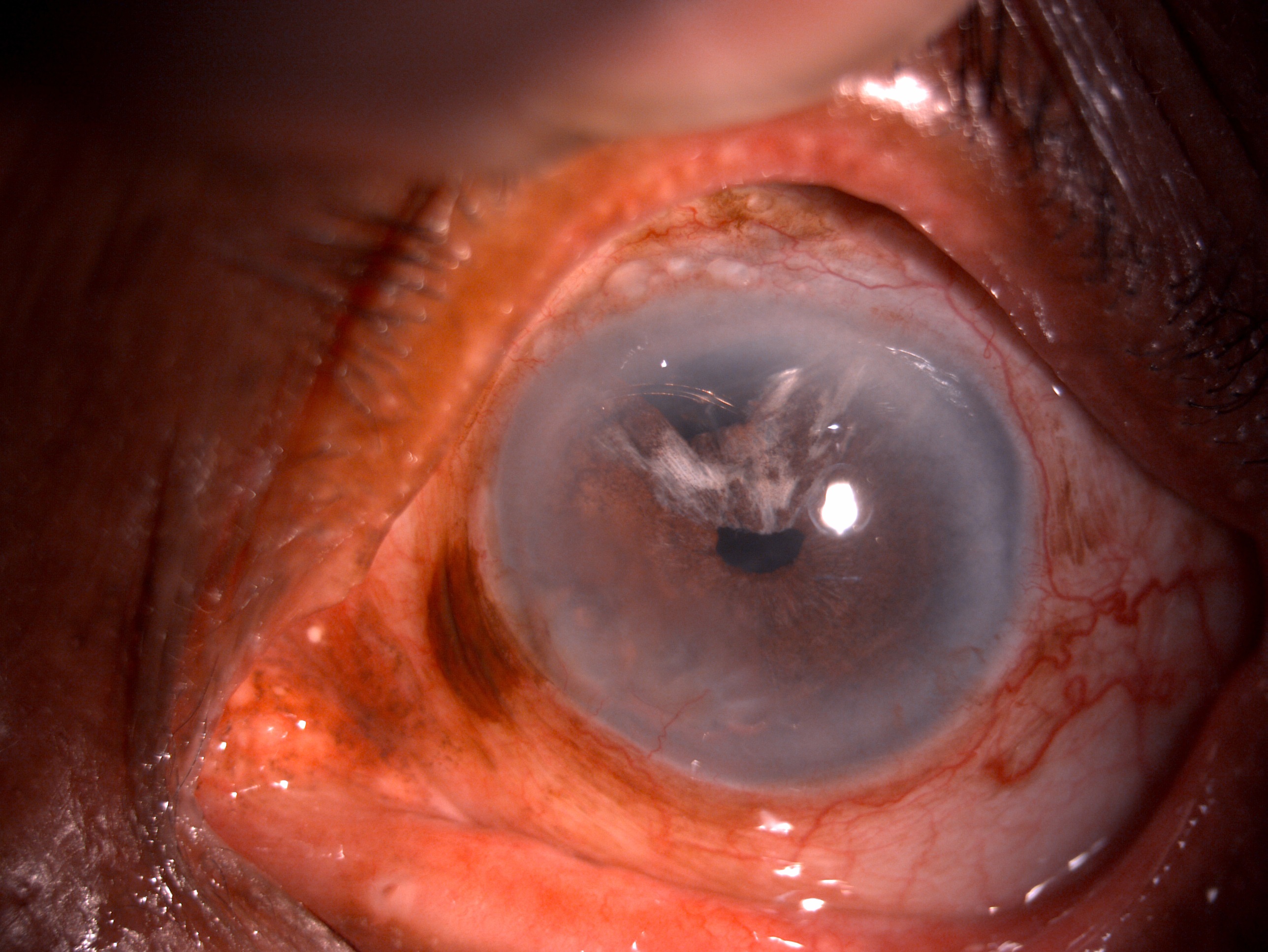
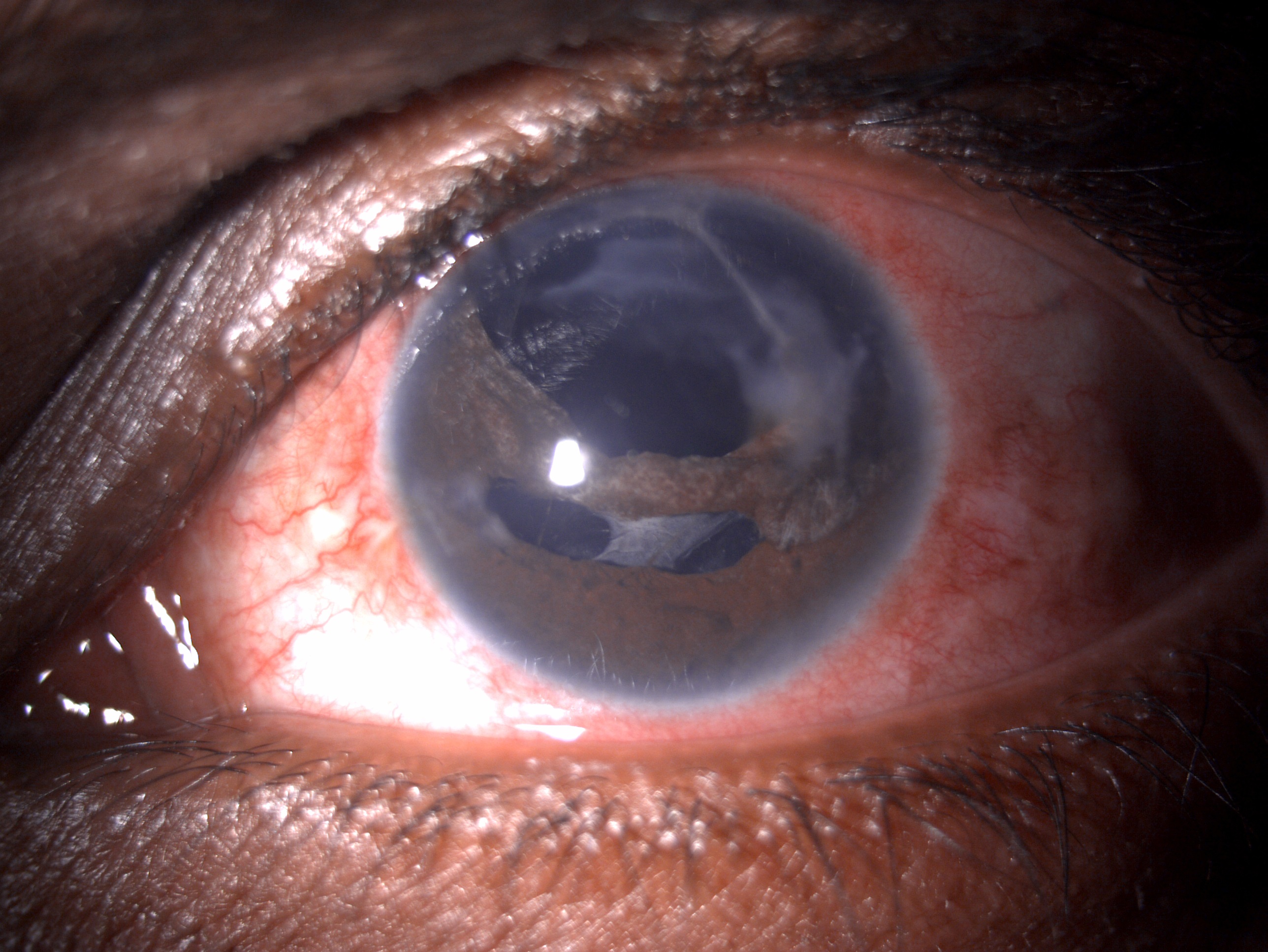
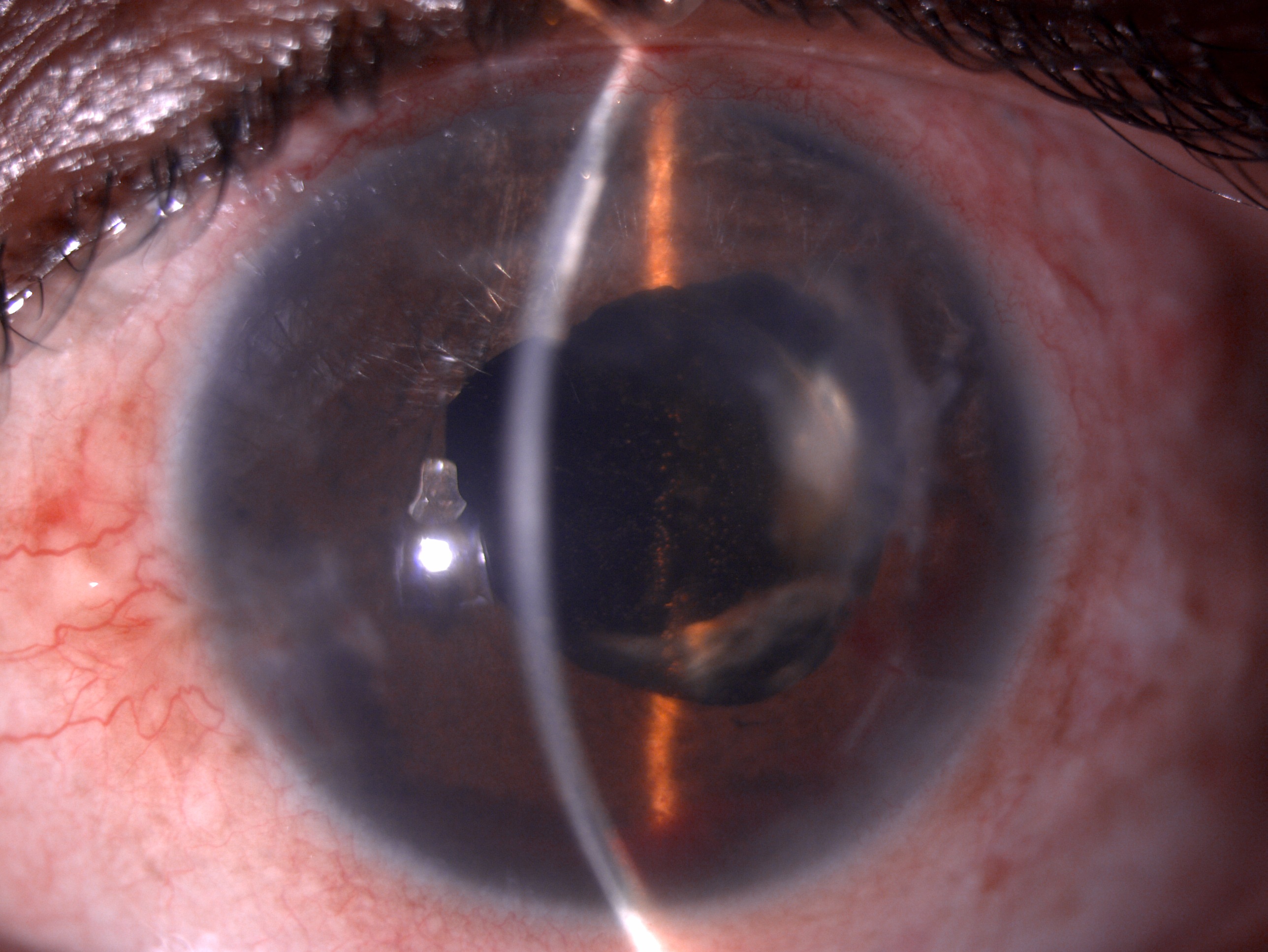
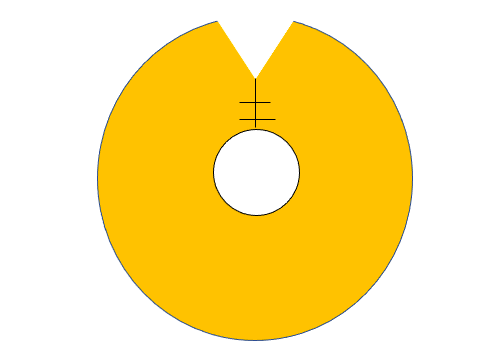
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Vásquez Quintero A,Pérez-Merino P,De Smet H, Artificial iris performance for smart contact lens vision correction applications. Scientific reports. 2020 Sep 4; [PubMed PMID: 32887927]
Laeng B,Endestad T, Bright illusions reduce the eye's pupil. Proceedings of the National Academy of Sciences of the United States of America. 2012 Feb 7; [PubMed PMID: 22308422]
Kanclerz P,Toto F,Grzybowski A,Alio JL, Extended Depth-of-Field Intraocular Lenses: An Update. Asia-Pacific journal of ophthalmology (Philadelphia, Pa.). 2020 May-Jun; [PubMed PMID: 32511121]
Mayer CS,Baur ID,Storr J,Khoramnia R, Bilateral Artificial Iris implantation in patients with bilateral iris defects. American journal of ophthalmology case reports. 2021 Jun; [PubMed PMID: 34027229]
Level 3 (low-level) evidenceOmar Yousif M, Single suture customized loop for large iridodialysis repair. Clinical ophthalmology (Auckland, N.Z.). 2016; [PubMed PMID: 27729765]
Bloom J,Motlagh M,Czyz CN, Anatomy, Head and Neck, Eye Iris Sphincter Muscle StatPearls. 2022 Jan; [PubMed PMID: 30335285]
Li S,Liang L, Protruding Iris Collarette. The New England journal of medicine. 2017 Mar 16; [PubMed PMID: 28296615]
Tamm ER,Ohlmann A, [Development of the human eye]. Der Ophthalmologe : Zeitschrift der Deutschen Ophthalmologischen Gesellschaft. 2012 Sep; [PubMed PMID: 22932837]
Level 3 (low-level) evidenceWynn TA,Vannella KM, Macrophages in Tissue Repair, Regeneration, and Fibrosis. Immunity. 2016 Mar 15; [PubMed PMID: 26982353]
Al-Thowaibi A,Kumar M,Al-Matani I, An overview of penetrating ocular trauma with retained intraocular foreign body. Saudi journal of ophthalmology : official journal of the Saudi Ophthalmological Society. 2011 Apr [PubMed PMID: 23960924]
Level 3 (low-level) evidenceLee WK,Aljic S,Barry P 2nd,Ganti L, Traumatic Iridodialysis Associated With Hyphema Secondary to Injury From a Bungee Cord. Cureus. 2021 Feb 11; [PubMed PMID: 33728213]
Qayum S,Anjum R,Rather S, Epidemiological profile of pediatric ocular trauma in a tertiary hospital of northern India. Chinese journal of traumatology = Zhonghua chuang shang za zhi. 2018 Apr; [PubMed PMID: 29605433]
Level 2 (mid-level) evidenceTalbot EM,Thorpe AW,Mushtaq I, Controlled-tension suture-tying forceps. Journal of the Royal College of Surgeons of Edinburgh. 1991 Oct; [PubMed PMID: 1757915]
Junjie Y,Tingting P,Huafang G,Han L,Suowang Z, Implantation of intraocular lens without viscoelastic agent in phacoemulsification cataract surgery. International ophthalmology. 2022 Jan 6; [PubMed PMID: 34993842]
Mayali H,Baser EF,Kurt E,Ilker SS, Corneal endothelial damage in phacoemulsification using an anterior chamber maintainer compared with using an ophthalmic viscosurgical device. Journal of cataract and refractive surgery. 2021 May 1; [PubMed PMID: 33252564]
Amon M,Bernhart C,Geitzenauer W,Kahraman G, The forceps-needle: Combining needle and grasping functions in a single instrument. Journal of cataract and refractive surgery. 2021 Jan 1; [PubMed PMID: 32675649]
Safran SG,Bonaffini SG,Chatha U, Thirty-three-gauge hypodermic needle-guided iris suturing technique. Journal of cataract and refractive surgery. 2021 Nov 1; [PubMed PMID: 33298777]
Kleinmann G,Chew J,Apple DJ,Assia EI,Mamalis N, Suturing a tear of the anterior capsulorhexis. The British journal of ophthalmology. 2006 Apr; [PubMed PMID: 16547318]
European Glaucoma Society Terminology and Guidelines for Glaucoma, 4th Edition - Chapter 2: Classification and terminologySupported by the EGS Foundation: Part 1: Foreword; Introduction; Glossary; Chapter 2 Classification and Terminology. The British journal of ophthalmology. 2017 May; [PubMed PMID: 28424171]
Riva I,Micheletti E,Oddone F,Bruttini C,Montescani S,De Angelis G,Rovati L,Weinreb RN,Quaranta L, Anterior Chamber Angle Assessment Techniques: A Review. Journal of clinical medicine. 2020 Nov 25; [PubMed PMID: 33255754]
Voss JO,Maier C,Wüster J,Beck-Broichsitter B,Ebker T,Vater J,Dommerich S,Raguse JD,Böning G,Thieme N, Imaging foreign bodies in head and neck trauma: a pictorial review. Insights into imaging. 2021 Feb 15; [PubMed PMID: 33587198]
Naveh N,Wysenbeek Y,Solomon A,Melamed S,Blumenthal M, Anterior capsule adherence to iris leading to pseudophakic pupillary block. Ophthalmic surgery. 1991 Jun; [PubMed PMID: 1896174]
Level 3 (low-level) evidenceCrawford A,Freundlich S,Zhang J,McGhee CNJ, Iris reconstruction: A perspective on the modern surgical armamentarium. Oman journal of ophthalmology. 2021 May-Aug; [PubMed PMID: 34345138]
Level 3 (low-level) evidencePanarese V, Moshirfar M. Pilocarpine. StatPearls. 2024 Jan:(): [PubMed PMID: 32310588]
Berridge TL,Gadie B,Roach AG,Tulloch IF, alpha 2-Adrenoceptor agonists induced mydriasis in the rat by an action within the central nervous system. British journal of pharmacology. 1983 Mar; [PubMed PMID: 6132641]
Level 3 (low-level) evidenceVásquez Quintero A,Pérez-Merino P,Fernández García AI,De Smet H, Smart contact lens: A promising therapeutic tool in aniridia. Archivos de la Sociedad Espanola de Oftalmologia. 2021 Nov; [PubMed PMID: 34836591]
L'Esperance FA Jr,James WA Jr, Argon laser photocoagulation of iris abnormalities. Transactions. Section on Ophthalmology. American Academy of Ophthalmology and Otolaryngology. 1975 Mar-Apr; [PubMed PMID: 1170672]
Ogawa GSH, Congenital iris coloboma repair with excision of colobomatous sphincter muscle. Journal of cataract and refractive surgery. 2021 Aug 1; [PubMed PMID: 32947385]
McCannel MA, A retrievable suture idea for anterior uveal problems. Ophthalmic surgery. 1976 Summer; [PubMed PMID: 778720]
Shin DH, Repair of sector iris coloboma. Closed-chamber technique. Archives of ophthalmology (Chicago, Ill. : 1960). 1982 Mar; [PubMed PMID: 7039574]
Siepser SB, The closed chamber slipping suture technique for iris repair. Annals of ophthalmology. 1994 May-Jun; [PubMed PMID: 7944159]
Pallin SL, Closed chamber iridoplasty. Ophthalmic surgery. 1981 Mar; [PubMed PMID: 7015214]
Level 3 (low-level) evidenceBehndig A, Small incision single-suture-loop pupilloplasty for postoperative atonic pupil. Journal of cataract and refractive surgery. 1998 Nov; [PubMed PMID: 9818329]
Nunziata BR, Repair of iridodialysis using a 17-millimeter straight needle. Ophthalmic surgery. 1993 Sep; [PubMed PMID: 8233338]
Level 3 (low-level) evidenceBardak Y,Ozerturk Y,Durmus M,Mensiz E,Aytuluner E, Closed chamber iridodialysis repair using a needle with a distal hole. Journal of cataract and refractive surgery. 2000 Feb; [PubMed PMID: 10683783]
Wachler BB,Krueger RR, Double-armed McCannell suture for repair of traumatic iridodialysis. American journal of ophthalmology. 1996 Jul; [PubMed PMID: 8659581]
Level 3 (low-level) evidenceNarang P,Agarwal A, Single-Pass Four-Throw Pupilloplasty Knot Mechanics. Journal of refractive surgery (Thorofare, N.J. : 1995). 2019 Mar 1; [PubMed PMID: 30855099]
Hu S,Wang M,Xiao T,Zhao Z, Iris reconstruction combined with iris-claw intraocular lens implantation for the management of iris-lens injured patients. Indian journal of ophthalmology. 2016 Mar; [PubMed PMID: 27146932]
Blair K,Alhadi SA,Czyz CN, Globe Rupture StatPearls. 2022 Jan; [PubMed PMID: 31869101]