Introduction
Keratometer or ophthalmometer is an instrument used to measure the anterior corneal curvature and the axis and extent of astigmatism.[1] The process of these measurements is called keratometry. Hermann von Helmholtz invented the first keratometer, and it came into vogue in 1851.[2] The earlier keratometer was designed by Jesse Ramsden and Everard Home in 1796. In keratometry, the measurements are performed at a fixed chord length of 2 to 3 mm, which falls within the spherical zone of the cornea.[3]
The keratometry is based on the principle that the anterior corneal surface behaves like a mirror and the image size varies with the corneal curvature. Hence the radius of curvature of the cornea can be calculated based on image size from the anterior corneal surface.[4]
In a keratometer, the relationship between the object, image, radius of refractive surface, and distance between the surface and object is denoted as r = 2ul/ o, where r is the radius of the reflective surface, o is the object size, l is the image size, and u is the distance measured between the reflective surface and object.[5] However, the exact measurement of image size poses a problem since it is difficult to entirely still a living eye while the image is being observed. The various type of manual keratometers can be Helmholtz keratometer, Bausch and Lomb, and Javal Schiotz keratometer.[6]
There can be surgical or operating keratometers as well as automated keratometers. The activity describes various types of keratometers, parts of a keratometer, indications of keratometry, limitations, complications, patient safety, education, and clinical significance of a keratometer.[7]
Procedures
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Procedures
Manual Keratometers
Helmholtz Keratometer
This consists of two plates. The image is displaced half of its length by both the plates, and total changes in distance or displacement give the size of the image. This doubling of the image helps with the necessity of not moving the living eye. If there is eye movement, the image will also move together during the process. Therefore, any difficulty in the adjustment of the eye is avoided. The plates used are made of glass and are a known thickness and refractive index. These plates are placed adjacent to each other so that each plate cover half of the object of a short telescope. The prime necessity is that the cylinder axis should coincide with the plane of separation of the glass plates. The glass plates can be inclined at an angle, and the angle of incident light can be varied and measured from a point in front.[2]
Bausch and Lomb Keratometer
This keratometer is based on the principle of constant object size and image size variability.[8]
Optics and Parts
Object: This is a circular mire with two plus and two minus signs. A bulb or a lamp is used to illuminate the mires with the help of mirrors placed diagonally. When light from the mire strikes the patient cornea, it produces a diminished image behind it. The image acts as an object for the rest of the optical system.
Objective lens: helps focus the light from the image of the mire (that acts as an object) along the central axis.[9]
Diaphragm and doubling prisms: A four aperture diaphragm is placed near the objective lens. Two doubling prisms are placed beyond the diaphragm, one having a base up and another a base out prism. The prisms can move independently and parallel to the central axis of the instrument. When light passes through the left diaphragmatic aperture, it is made to deviate by the base-up prism above the main optical axis. Similarly, when the light passes through the right diaphragmatic aperture, it is made to deviate by the base out prism, thus placing the second image to the right of the central axis. When light passes through the upper and lower aperture, it doesn't pass through the prism, and an image is produced on the axis.
The total area of combined upper and lower apertures is the sum of each aperture separately, but the brightness of the image is equal. The upper and lower apertures act as Scheiner's disc, doubling the image size. Hence this helps in continuous monitoring of the correct focus. The image doubling phenomenon is a unique phenomenon for Bausch and Lomb keratometer. Double images are produced adjacent as well as 90 degrees to each other; this helps in calculating the power of the cornea in two different meridians without any rotation of the instrument. Hence, this is also labeled as one position keratometer.[1]
Eyepiece: This lens helps get a magnified view of the doubled image.
Keratometry Procedure
Instrument Calibration: The keratometer is calibrated with steel balls. A whiteboard is placed in front of the objective piece, and a black line is seen sharply focussed on it. The steel ball of the particular radius of curvature is used, the ball is placed in front of the keratometer, and the value is set on the scale. The mires are focussed on the hit and trial method by the anticlockwise and clockwise movement of the eyepiece. When the mires are focused, the instrument is said to be calibrated.[1]
Patient Adjustment: To obtain perfect keratometry, patient positioning is of utmost importance. The head should be against the headrest, and the chin should rest on the chin rest. An occluder should cover the other eye which is not being examined. This is followed by chin adjustment till the patient's pupil and the projective knob are at the same level.
Mire Focusing
After instrument calibration, alignment, and positioning of the patient, the mires are focused in the corneal center.
Corneal Curvature Assessment
The keratometer is focused on the corneal image so that there is no doubling of the central corneal image. To assess the curvature in the horizontal meridian, the plus sign of the central and left image is superimposed, taking into account the horizontal measuring control. Similarly, the central and upper images are taken into account for assessing the curvature in the vertical meridian. If there is oblique astigmatism, the two-plus signs will not be aligned. The instrument has to be then rotated till both plus signs are aligned.[10]
Javal Schiotz Keratometer
This instrument is based on variable object size and the constant image size principle.[11]
Optical and Parts
Object- This consists of two mires mounted on the arc which can be moved synchronously. The two mires combinedly form the object; hence the variable size is obtained by the movement. The first mire is stepped and has a green filter, and the other mire is rectangular and has a red filter. The mires are split in the center horizontally and are illuminated by a lamp. The first image obtained from the mires acts as an object for the rest of the optical axis.
The objective lens and doubling prisms
They form a doubled image of the new object (mires images created by the cornea). It uses a Wollaston prism which is a type of doubling prism. There is a fixed image doubling by the birefringent, also known as double refracting).[12]
Eyepiece Lens
It helps to obtain a magnified view of the doubled image.
The keratometry procedure of the Javal Schiotz keratometer is more or less similar to Bausch and Lomb keratometer.
Automated Keratometers
They are similar to manual keratometers. In this, the image reflected off the target is focused on the photodetector, which assesses the image size, and hence the radius of curvature is calculated. The mire is illuminated with the IR rays, and an infrared photodetector is used. The various advantages of automated keratometers are that they are compact, less time-consuming, and require less skill to operate.
The majority of the previous studies have found good accuracy using autokeratometry. In the market, the autokeratometers are available as isolated or autorefractometers of autokeratorefractometers. The various types of automated keratometers available are the IOL master, Pentacam, Orbscan, and corneal topographer.[13]
Surgical Keratometer
In this, the keratometers are attached to the microscope. The surgical keratometer helps in monitoring astigmatism while performing corneal and limbal procedures. However, the instrument has limited accuracy due to varied factors such as:
- It is challenging to align the visual axis of the patient with the optical axis of the keratometer.
- Anterior chamber air creates a second target reflection.
- The external compression on the globe results in a change in the corneal curvature.
- The calibrations for keratometers are for a fixed distance from the anterior corneal surface. Hence the different microscope lenses result in different working distances.[7]
Parts of Keratometer
- Headrest
- Chinrest
- Anteroposterior rotation axis scale
- Eyepiece
- Horizontal knob
- Vertical knob
- Focusing knob
- Locking knob
- Elevating knob
- Chin height knob
- Keratometer height knob
- Occluding shield
- Leveling sight
- Horizontal measuring drum
- Vertical measuring drum
- Axis scale[14]
Indications
There are various clinical indications of keratometers in routine ophthalmic practice:
- Astigmatism assessment: Keratometers help to assess the corneal astigmatic error[15]
- Contact lens fitting: Keratometers help to assess the anterior corneal surface, thus prove valuable for contact lens fitting[16]
- Corneal shape assessment: Keratometers help to assess the shape in keratoconus and kertaoglobus[17]
- Contact lens flexure assessment: Keratometers help assess the rigid gas permeable lens flexure.[18]
- Anisometropia: Keratometers help to differentiate between axial versus curvatural anisometropia[19]
- Refractive error assessment: Keratometers help to assess the refractive error in case of hazy media.[20]
- IOL power calculation: Keratometer helps to know the K reading, an essential component of the SRK formula for IOL power calculation.[21]
- Astigmatism monitoring: They help to assess the pre and post-surgical astigmatism[22]
Normal and Critical Findings
Relation Between Radius of Curvature and Power of Cornea
This is indicated by the following equation D= n-1/r, where D is the power of cornea in diameters, n is the refractive index of the cornea, and r is the radius of curvature. Ever since the invention of the keratometer by Helmholtz, the refractive index of the cornea has been 1.3375 for calibrating the instrument. Therefore the formula is read as D= 1.3375-1/r or 0.3375/r or r = 0.3375/D. Hence, the parameters of the keratometers are always labeled for the radius of curvature and dioptric power.[23]
Range of Keratometer
This ranges from 36 to 52 D (6.5 to 9.38 mm). The lower limit is 30D (5.6 mm), and the upper limit is 61 D (10.9 mm) using a lens of -1.0 D and +1.25 D, respectively, in front of the telescope's objective.[24]
Interfering Factors
Limitations
- The keratometer measurements are based on the false belief that the cornea is a sphere or has a spherocylindrical configuration, where the two principal meridians are at 90 degrees to each other. In reality, the cornea is aspheric in configuration.[25]
- The peripheral corneal surface is not considered while having refractive measurements. The keratometers take into account only the central curvature of 3 to 4 mm, which is a smaller portion and is a potential limitation.[26]
- The keratometer has limited accuracy and loses accuracy in the very flat or steep cornea.[27]
- Corneal irregularities like abrasion, erosions, epithelial defects, etc., will preclude the perfect keratometry reading due to irregular astigmatism.[28]
- Keratometers have assumed the index of refraction in radius to diopter conversion[29]
- It employs para axial optics to measure the corneal surface power.[23]
- It approximates the distance from the focal point to the distance to the image.
- Regular astigmatism due to one position astigmatism is also a limitation.
Factors Leading to Errors in Keratometry
- Faulty or improper calibration
- Excessive lacrimation
- Faulty lid position
- The patient has not fixed the instrument
- Abnormal patient position
- Accommodation error
- Corneal folds or distortion
- The abnormal focus of the corneal image[30]
Complications
- Improper functioning due to dust accumulation
- Damage to the eyepiece and prisms
- Friction between instrument parts due to reduced lubrication
- Damage to the bulb or fuse bulb
- Damage to on and off button and cable
- Improper calibration[31]
Patient Safety and Education
Keratometry is a routine investigation in day-to-day clinical practice. Every patient must be educated regarding the keratometry procedure and the importance of doing it. The patient must be educated regarding the position and how to align themselves with the instrument. The patient should also be educated on how the mires appear.
Clinical Significance
An ideal keratometer can measure the radius in various meridians from the axis of the cornea. The keratometers are designed to be rotated along a particular axis. The objects are labeled as mires. A double device has been incorporated to avoid errors and confusion due to the continuous movement of the eyes.[32]
Spherical Cornea
This is characterized by no difference in power between the two principal meridians, and the mire appears as a perfect sphere.[33]
Astigmatism
This is characterized by the difference in the power between the two principal meridians. As with the rule of astigmatism, horizontally oval mires are seen. As against the rule of astigmatism, vertically oval mires are seen. In oblique astigmatism, the principal meridian lies between 30 and 60 degrees and 120 and 150 degrees. The irregular anterior corneal surface has irregular mires and a doubling of mires.[34]
Keratoconus
Inclination and jumping of mires are seen, also called pulsating mires. Minification of mires is seen in advanced keratoconus due to high myopia. Significant astigmatism shows oval mires. In advanced keratoconus, wavy, irregular, and distorted mires are also seen.[35]
Media
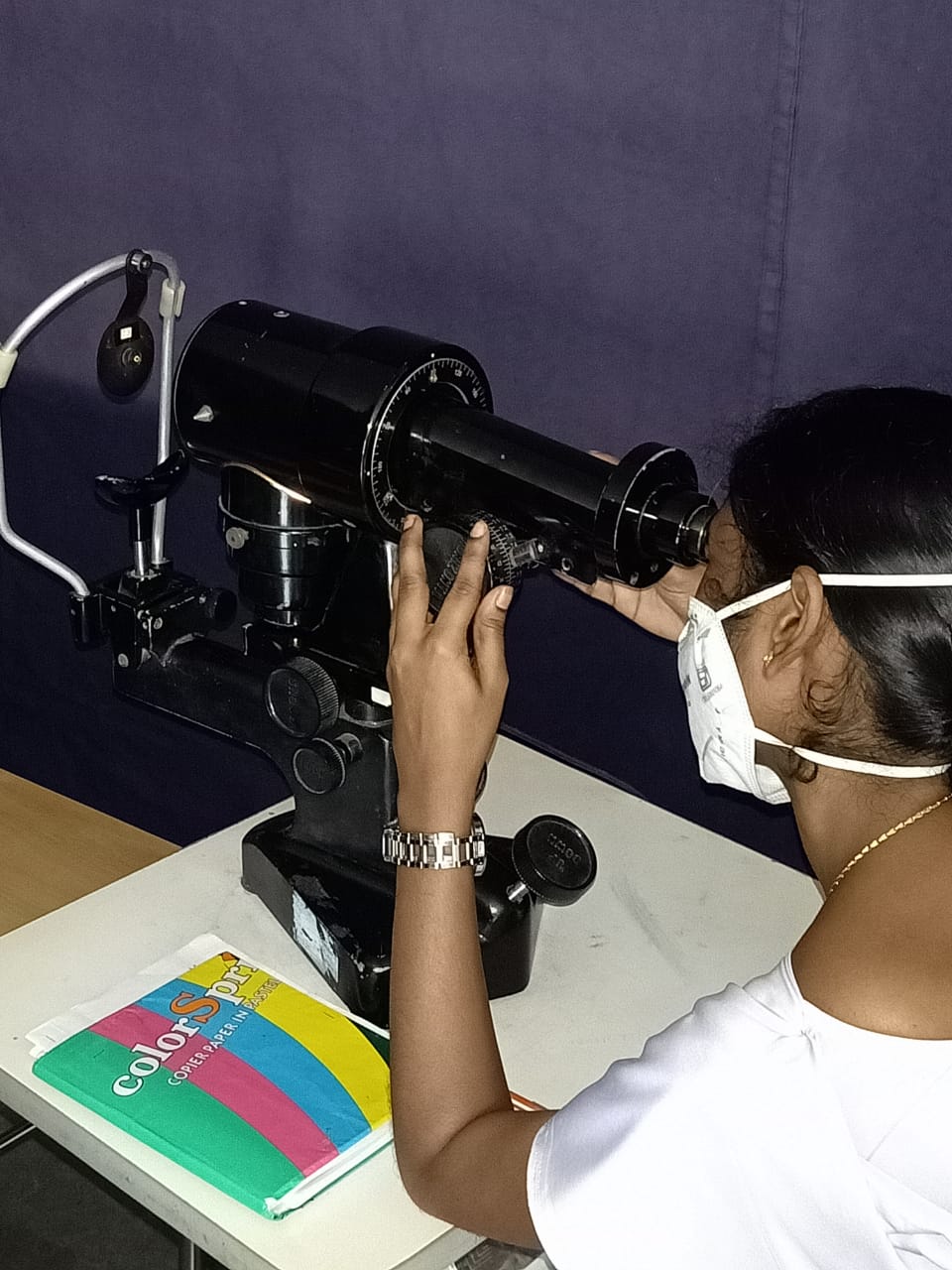
(Click Image to Enlarge)
References
Cordero I. Verifying the calibration of a manual one-position keratometer. Community eye health. 2013:26(84):77 [PubMed PMID: 24782588]
Godefrooij DA, Galvis V, Tello A. Von Helmholtz's ophthalmometer: historical review and experience with one of the last surviving original devices. Acta ophthalmologica. 2018 May:96(3):314-320. doi: 10.1111/aos.13493. Epub 2017 Aug 3 [PubMed PMID: 28772001]
Hashemi H, Heydarian S, Khabazkhoob M, Yekta A, Emamian MH, Fotouhi A. Keratometry in children: Comparison between auto-refractokeratometer, rotating scheimpflug imaging, and biograph. Journal of optometry. 2019 Apr-Jun:12(2):99-110. doi: 10.1016/j.optom.2018.12.002. Epub 2019 Mar 14 [PubMed PMID: 30879970]
Martin R. Cornea and anterior eye assessment with placido-disc keratoscopy, slit scanning evaluation topography and scheimpflug imaging tomography. Indian journal of ophthalmology. 2018 Mar:66(3):360-366. doi: 10.4103/ijo.IJO_850_17. Epub [PubMed PMID: 29480244]
Miller JM. A handheld open-field infant keratometer (an american ophthalmological society thesis). Transactions of the American Ophthalmological Society. 2010 Dec:108():77-95 [PubMed PMID: 21212850]
Manning CA, Kloess PM. Comparison of portable automated keratometry and manual keratometry for IOL calculation. Journal of cataract and refractive surgery. 1997 Oct:23(8):1213-6 [PubMed PMID: 9368167]
Ventura L, De Groote JJ, Saia P, Faria e Sousa SJ. Keratometry device for surgical support. Biomedical engineering online. 2009 Dec 8:8():37. doi: 10.1186/1475-925X-8-37. Epub 2009 Dec 8 [PubMed PMID: 19995421]
Douthwaite WA, Burek H. The Bausch and Lomb keratometer does not measure the tangential radius of curvature. Ophthalmic & physiological optics : the journal of the British College of Ophthalmic Opticians (Optometrists). 1995 May:15(3):187-93 [PubMed PMID: 7659418]
Szirth BC, Matsumoto E, Wright KW, Murphree AL. Attachment for the Bausch & Lomb keratometer in pediatrics. Journal of pediatric ophthalmology and strabismus. 1987 Jul-Aug:24(4):186-9 [PubMed PMID: 3668766]
Chang M, Kang SY, Kim HM. Which keratometer is most reliable for correcting astigmatism with toric intraocular lenses? Korean journal of ophthalmology : KJO. 2012 Feb:26(1):10-4. doi: 10.3341/kjo.2012.26.1.10. Epub 2012 Jan 14 [PubMed PMID: 22323879]
Dehnavi Z, Khabazkhoob M, Mirzajani A, Jabbarvand M, Yekta A, Jafarzadehpur E. Comparison of the Corneal Power Measurements with the TMS4-Topographer, Pentacam HR, IOL Master, and Javal Keratometer. Middle East African journal of ophthalmology. 2015 Apr-Jun:22(2):233-7. doi: 10.4103/0974-9233.151884. Epub [PubMed PMID: 25949084]
Tennen DG, Keates RH, Montoya C. Comparison of three keratometry instruments. Journal of cataract and refractive surgery. 1995 Jul:21(4):407-8 [PubMed PMID: 8523284]
Leyland M, Benjamin L. Clinical assessment of a hand-held automated keratometer in cataract surgery. Eye (London, England). 1997:11 ( Pt 6)():854-7 [PubMed PMID: 9537145]
Level 1 (high-level) evidenceKarabatsas CH, Cook SD, Papaefthymiou J, Turner P, Sparrow JM. Clinical evaluation of keratometry and computerised videokeratography: intraobserver and interobserver variability on normal and astigmatic corneas. The British journal of ophthalmology. 1998 Jun:82(6):637-42 [PubMed PMID: 9797664]
Alpins N, Ong JKY, Stamatelatos G. Assessing Total Keratometry Astigmatism, Simulated Keratometry, and Total Corneal Topographic Astigmatism Against Manifest Refractive Cylinder. Journal of refractive surgery (Thorofare, N.J. : 1995). 2021 Mar:37(3):198-201. doi: 10.3928/1081597X-20210105-01. Epub 2021 Mar 18 [PubMed PMID: 34038302]
Rajabi MT, Mohajernezhad-Fard Z, Naseri SK, Jafari F, Doostdar A, Zarrinbakhsh P, Rajabi MB, Kohansal S. Rigid contact lens fitting based on keratometry readings in keratoconus patients: predicting formula. International journal of ophthalmology. 2011:4(5):525-8. doi: 10.3980/j.issn.2222-3959.2011.05.13. Epub 2011 Oct 18 [PubMed PMID: 22553715]
Lauschke JL, Lawless M, Sutton G, Roberts TV, Hodge C. Assessment of corneal curvature using verion optical imaging system: a comparative study. Clinical & experimental ophthalmology. 2016 Jul:44(5):369-76. doi: 10.1111/ceo.12687. Epub 2016 Feb 20 [PubMed PMID: 27381574]
Level 2 (mid-level) evidenceSorbara L, Fonn D, MacNeill K. Effect of rigid gas permeable lens flexure on vision. Optometry and vision science : official publication of the American Academy of Optometry. 1992 Dec:69(12):953-8 [PubMed PMID: 1300519]
Level 1 (high-level) evidencePalamar M, Degirmenci C, Biler ED, Egrilmez S, Uretmen O, Yagci A. Evaluation of the anatomic and refractive differences in hyperopic anisometropia. International ophthalmology. 2016 Dec:36(6):881-886 [PubMed PMID: 26887566]
Moghadas Sharif N, Yazdani N, Shahkarami L, Ostadi Moghaddam H, Ehsaei A. Analysis of Age, Gender, and Refractive Error-Related Changes of the Anterior Corneal Surface Parameters Using Oculus Keratograph Topography. Journal of current ophthalmology. 2020 Jul-Sep:32(3):263-267. doi: 10.4103/JOCO.JOCO_7_20. Epub 2020 Jul 4 [PubMed PMID: 32775801]
Lawless M, Jiang JY, Hodge C, Sutton G, Roberts TV, Barrett G. Total keratometry in intraocular lens power calculations in eyes with previous laser refractive surgery. Clinical & experimental ophthalmology. 2020 Aug:48(6):749-756. doi: 10.1111/ceo.13760. Epub 2020 Apr 27 [PubMed PMID: 32279436]
Pontikos N, Chua S, Foster PJ, Tuft SJ, Day AC, UK Biobank Eye and Vision Consortium. Frequency and distribution of corneal astigmatism and keratometry features in adult life: Methodology and findings of the UK Biobank study. PloS one. 2019:14(9):e0218144. doi: 10.1371/journal.pone.0218144. Epub 2019 Sep 19 [PubMed PMID: 31536508]
Tang M, Chen A, Li Y, Huang D. Corneal power measurement with Fourier-domain optical coherence tomography. Journal of cataract and refractive surgery. 2010 Dec:36(12):2115-22. doi: 10.1016/j.jcrs.2010.07.018. Epub [PubMed PMID: 21111315]
Level 2 (mid-level) evidenceHashemi H, Yekta A, Shokrollahzadeh F, Aghamirsalim M, Ostadimoghaddam H, Hashemi A, Heydarian S, Khabazkhoob M. The Distribution of Keratometry in a Population Based Study. Journal of current ophthalmology. 2021 Jan-Mar:33(1):17-22. doi: 10.1016/j.joco.2019.06.004. Epub 2021 Mar 26 [PubMed PMID: 34084952]
Mohammadi SF, Khorrami-Nejad M, Hamidirad M. Posterior corneal astigmatism: a review article. Clinical optometry. 2019:11():85-96. doi: 10.2147/OPTO.S210721. Epub 2019 Aug 12 [PubMed PMID: 31496856]
Cavas-Martínez F, De la Cruz Sánchez E, Nieto Martínez J, Fernández Cañavate FJ, Fernández-Pacheco DG. Corneal topography in keratoconus: state of the art. Eye and vision (London, England). 2016:3():5. doi: 10.1186/s40662-016-0036-8. Epub 2016 Feb 22 [PubMed PMID: 26904709]
Luft N, Siedlecki J, Reinking F, Mayer WJ, Schworm B, Kassumeh S, Priglinger SG, Dirisamer M. Impact of extreme (flat and steep) keratometry on the safety and efficacy of small incision lenticule extraction (SMILE). Scientific reports. 2021 Sep 8:11(1):17854. doi: 10.1038/s41598-021-97375-4. Epub 2021 Sep 8 [PubMed PMID: 34497302]
Roh HC, Chuck RS, Lee JK, Park CY. The effect of corneal irregularity on astigmatism measurement by automated versus ray tracing keratometry. Medicine. 2015 Apr:94(13):e677. doi: 10.1097/MD.0000000000000677. Epub [PubMed PMID: 25837759]
Savini G, Hoffer KJ. Intraocular lens power calculation in eyes with previous corneal refractive surgery. Eye and vision (London, England). 2018:5():18. doi: 10.1186/s40662-018-0110-5. Epub 2018 Jul 8 [PubMed PMID: 30038922]
Mittelviefhaus H, Gentner C. [Errors in keratometry for intraocular lens implantation in infants]. Der Ophthalmologe : Zeitschrift der Deutschen Ophthalmologischen Gesellschaft. 2000 Mar:97(3):186-8 [PubMed PMID: 10789175]
Piñero DP, Camps VJ, Caravaca-Arens E, de Fez D, Blanes-Mompó FJ. Algorithm for Correcting the Keratometric Error in the Estimation of the Corneal Power in Keratoconus Eyes after Accelerated Corneal Collagen Crosslinking. Journal of ophthalmology. 2017:2017():8529489. doi: 10.1155/2017/8529489. Epub 2017 Oct 22 [PubMed PMID: 29201459]
Ventura L, Riul C, Sousa SJ. Optical projection mires for measurements of the radii of curvature of the cornea in biomicroscopes. Applied optics. 2007 Oct 10:46(29):7155-61 [PubMed PMID: 17932523]
Al-Sayyari TM, Fawzy SM, Al-Saleh AA. Corneal spherical aberration and its impact on choosing an intraocular lens for cataract surgery. Saudi journal of ophthalmology : official journal of the Saudi Ophthalmological Society. 2014 Oct:28(4):274-80. doi: 10.1016/j.sjopt.2014.06.005. Epub 2014 Jun 25 [PubMed PMID: 25473343]
Refai TA. Evaluation of the orientation of the steepest meridian of regular astigmatism among highly myopic Egyptian patients seeking non-ablative surgical correction of the refractive error. Electronic physician. 2015 Sep:7(5):1296-300. doi: 10.14661/1296. Epub 2015 Sep 16 [PubMed PMID: 26435831]
Espandar L, Meyer J. Keratoconus: overview and update on treatment. Middle East African journal of ophthalmology. 2010 Jan:17(1):15-20. doi: 10.4103/0974-9233.61212. Epub [PubMed PMID: 20543932]
Level 3 (low-level) evidence