Introduction
Refractivity is a principal property of light and explains the changes in the path of light rays following transmission or propagation via various materials or optical media. The cornea and crystalline lens are the principal refractive tissues of the human eye.[1] Geometrical optics is a branch of physics that studies the observed changes in the path of light rays refracted by various media and is directly applicable to vision.
Although D'Armate designed the first pair of spectacle lenses in the 13th century, refractive errors remained a significant irredeemable impairment. In the 19th century, the French ophthalmologist Cuignet was credited with developing what later came to be known as retinoscopy based on the work of Foucault.[2][3][4] The invention of the retinoscope, sometimes referred to as a skiascope, pupilloscope, shadowscope, scotoscope, or umbrascope, was a milestone that made it possible to determine the refractive status of the eyes.[4]
Various procedures or techniques are employed when evaluating the ocular refractive state.[5] Objective techniques include those without subjective input from test subjects or patients; retinoscopy is an objective refraction technique. Subjective refraction includes input from patients. (See Image. Optometrist Assessing Subjective Refraction During Ophthalmoscopic Examination)
Retinoscopy is an exam technique that utilizes an external light source supplied by a retinoscope to project light rays through the transparent ocular media to observe their reflection off the retina.[6] (See Image. Angle of incidence) Early retinoscopes comprised single or separate perforated mirrors through which illumination from an external source could be directed toward the eyes of the patient. Wolff invented the first internally illuminated electric retinoscope in 1901. These early electric retinoscopes projected an evenly round spot of light, which did not permit the assessment of orthogonal planes. Copeland invented the streak retinoscope in 1927 to more accurately detect astigmatism; the streak technique is still in use in modern practice.[7] While continued advancements have led to marked improvements in automated optical devices, retinoscopy remains a useful clinical technique.[5][8]
Retinoscopic procedures can be broadly categorized as static or dynamic.[9] Static retinoscopy requires the patient to be in a relaxed accommodative state, which may be natural or pharmaceutically induced. Dynamic retinoscopy requires active accommodation.
Static Retinoscopy
During static retinoscopy, the examiner observes for reflex neutralization during consistent patient fixation at an immovable visual stimulus, target, or optotype situated at optical infinity, defined as 6 m or 20 ft.[10] Static retinoscopy can be employed during routine noncycloplegic or cycloplegic objective refraction assessments. Noncycloplegic objective refraction using the retinoscope is carried out while the accommodative facility of the patient remains naturally intact; this is colloquially termed dry retinoscopy. Cycloplegic retinoscopy is performed after the instillation of cycloplegic agents to restrict the natural accommodative response temporarily and may be referred to as wet retinoscopy.[10]
Cycloplegic retinoscopy is particularly useful when assessing patients who cannot or will not fixate on a target or follow instructions, such as pediatric patients or patients with special needs.[10][11] Wet retinoscopy may also be required in patients with amblyopia, tropias, accommodative phorias, accommodative spasm, latent hyperopia, moderate-to-high anisometropia, high lenticular astigmatism, high myopia, other pediatric ametropias, or oscillatory nystagmus.[12][13] Commonly utilized topical cycloplegic agents include tropicamide, cyclopentolate, scopolamine, homatropine, and atropine; selecting the most appropriate agent requires consideration of the age of the patient, allergy profiles, and other comorbidities.[14][15]
In cases where cycloplegic agents are not indicated or inappropriate, the Mohindra retinoscopy technique may be employed. This technique presents the retinoscope light as a near stimulus to elicit direct fixation from the patient throughout the assessment and derives final objective values using an algebraic sum of objective findings and a constant factor of -1.25 D from the habitual working distance and resting state of accommodation.[16][17]
Dynamic Retinoscopy
Dynamic retinoscopy requires fixation at a near target at a distance less than optical infinity and is employed to determine innate accommodative response to presented stimuli at given distances.[18] Many dynamic retinoscopic techniques have been described. While the most commonly utilized retinoscopic techniques are the monocular estimation method and the Nott method, other techniques include the Bell, Book, stress point, and binocular cross-cylinder retinoscopic methods.[18][19][20]
The monocular estimation method (MEM) of dynamic retinoscopy proposed by Haynes in 1960 requires maintaining the near-fixation target and retinoscope at equivalent distances while utilizing lenses to attempt reflex neutralization. The impression of an accommodative lag or lead can be derived from the resultant dioptric powers.[18]
Nott dynamic retinoscopy employs a static near-fixation target and moves the retinoscope until reflex neutralization can be observed. The distance between the instrument and the patient is used to derive the accommodative response.[18]
Indications
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Indications
The principal function of retinoscopy is the objective determination of refractive error. However, unlike refractometry-only modalities, retinoscopy can be used to assess accommodative function and provide objective diagnostic clues to ocular diseases of the cornea and crystalline lens, including but not limited to keratoconus, cataracts, or postsurgical corneal ectasia.[21][22] Retinoscopy can also detect irregular corneal and lenticular astigmatism, seen as a scissor-like motion of the retinoscope streak. Retinoscopy can provide early diagnosis of progressive corneal diseases, especially when more sophisticated equipment such as keratometers, corneal topographers, videokeratography, and higher-definition slit lamp biomicroscope instruments are unavailable.[21]
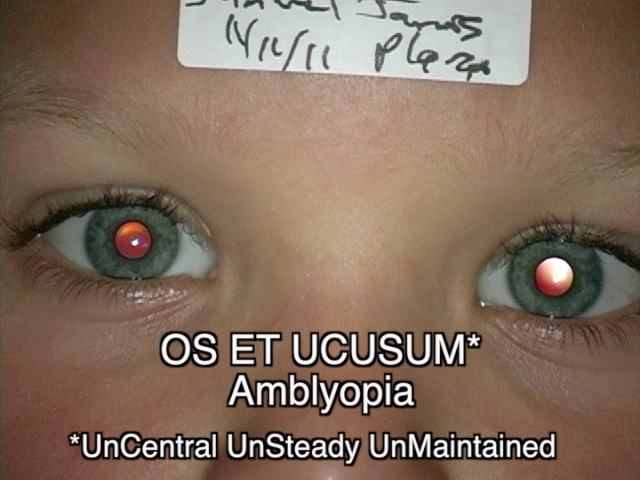
Retinoscopy can also be employed during a routine retinal reflex screening of infants.[23] Leukocoria identified during retinoscopy may indicate pediatric cataracts, retinal hamartomas, or retinoblastoma.[23] (See Image. Leukocoria) The Bruckner test may be performed during retinoscopy to determine amblyopia or anisometropia. (See Image. Amblyopia) Objective refraction may be the only way to determine a refractive endpoint in young children or patients with significant ocular deviation.
Contraindications
There are no known contraindications to retinoscopy.
Equipment
Minimal equipment is required to perform retinoscopy.[24][25][26][27] Recommended equipment includes:
- Retinoscope: streak retinoscope is preferred
- Trial frames or phoropter
- Lenses of various powers (phoropter mounted lenses, loose lenses from the trial frame, or lens racks)
- Distant or near-calibrated fixation targets.
Personnel
Retinoscopy may be performed by any personnel trained and found to be proficient in the technique.
Technique or Treatment
The "hand-to-eye" rule is advised during retinoscopy to maintain the instrument along a longitudinal axis to the eye being assessed so that light rays are not incident at acute or oblique angles to the plane of the observer. The "hand-to-eye" rule mandates retinoscopists whose capabilities permit handling the instrument and viewing through its aperture with the hand and eye ipsilateral to the eye being examined. For example, the right hand and right eye of the examiner are engaged while assessing the right eye of the patient, and vice-versa.[10]
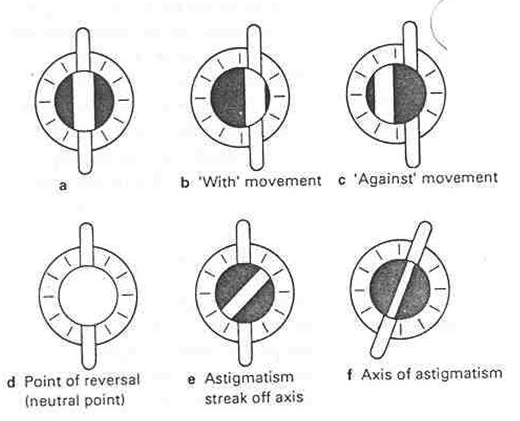
While observing the pupillary red reflex with the retinoscope streak oriented vertically, the instrument is gently moved from side to side to scope the horizontal meridia. (See Image. Steps of Retinoscopy) When the retinoscope streak is oriented horizontally, the streak is moved upward and downward along the pupillary margin to scope the vertical meridia. Either a "with-motion" or an "against-motion" can be observed. Observation of "with-motion" indicates the addition of plus lens powers, while "against-motion" indicates the addition of minus lens powers.[28]
The principal meridia to observe during retinoscopy are the power and axis meridia. During static retinoscopy, the power meridian is the slower, or further from neutralization, of 2 "with-motion" reflexes for hyperopes or the quicker, or closer to neutralization, of 2 "against-motion" reflexes for myopes.[10] The axis meridian is neutralized by introducing minus cylindrical lenses oriented along the observed streak axis and progressively increasing lens powers until reflex neutralization or motion reversal is first observed. Proper axis orientation can be estimated by observing the intrapupillary streak and comparing it against the orientation of the external streak of light projected from the retinoscope.[1]
Although precise axis determination is often improbable, gross axis orientation may be estimated as an acute, oblique, or perpendicular objective finding. Refinement of the cylindrical axis can be pursued during a subjective refraction procedure.[29][30] Lens transposition formulae can convert to plus cylindrical findings following retinoscopy if preferable.
Issues of Concern
There are several issues of concern about retinoscopy for exact refractive error localization, particularly in cases where the subjective technique is not the recommended endpoint.[10][31][32][33][34] These issues include:
- The accuracy of the results from retinoscopy is very dependent on the skill and observation of the examiner.
- Procedural variation in vertex distance and spectacle plane-to-mirror distance influence objective outcomes. The distance is estimated as an algebraic value in diopters.
- Reflex saccades and involuntary extrinsic ocular movements alter streak orientation.
- The attention span of the patient undergoing retinoscopy must be adequate to ensure completion of the procedure; retinoscopy may be of limited use in specific populations.
- Failure to pull the retinoscope sleeve into the correct position can lead to false negative results.
- General measures of instrument care are essential to avoid misalignment of the internal projecting apparatus or damage to components of the illumination system.
- Retinoscopists must be aware of atypical reflexive movements, often due to spherical aberrations, astigmatism, or scissoring reflexes.
Complications
Complications of retinoscopy are restricted to cycloplegic agents and may include blurred vision or temporary photophobia; allergic reactions to cycloplegic agents are uncommon.[14]
Clinical Significance
The large-scale availability of automated refractometers has undoubtedly improved the repeatability, speed, and accuracy of objective refraction, albeit while offering chiefly quantitative findings.[11] Retinoscopy, on the other hand, offers qualitative clinical value beyond a quantitative measure of the refractive state.[19] MEM retinoscopy is also adjunctive in the workup of accommodative and vergence anomalies. Retinoscopy offers greater flexibility and practicality when performing eye examinations on toddlers and young children; automated refractometers require patients to remain still to achieve accurate results.[17][18]
Enhancing Healthcare Team Outcomes
Uncorrected refractive errors remain among the leading global causes of preventable functional visual limitations.[35] Basic retinoscopic evaluations are a viable tool for the early detection and correction of refractive errors within underserved communities. Clinical education strategies centered around skill acquisition and continuing professional development are essential to ensure retinoscopy proficiency for optometrists, primary care practitioners, ophthalmologists, community health or ophthalmic nurses, and other targeted allied personnel.[36] Primary care practitioners should know critical retinoscopic signs and their triage indications, particularly when practicing in a system characterized by a shortage of specialized eye health professionals. Although automated objective refractometry offers many benefits, the cost of individual units is frequently prohibitive to systems with limited resources. Additionally, retinoscopy can provide quantitative results of clinical diseases outside the refractive state, promoting early referral to specialty care and improved patient outcomes.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
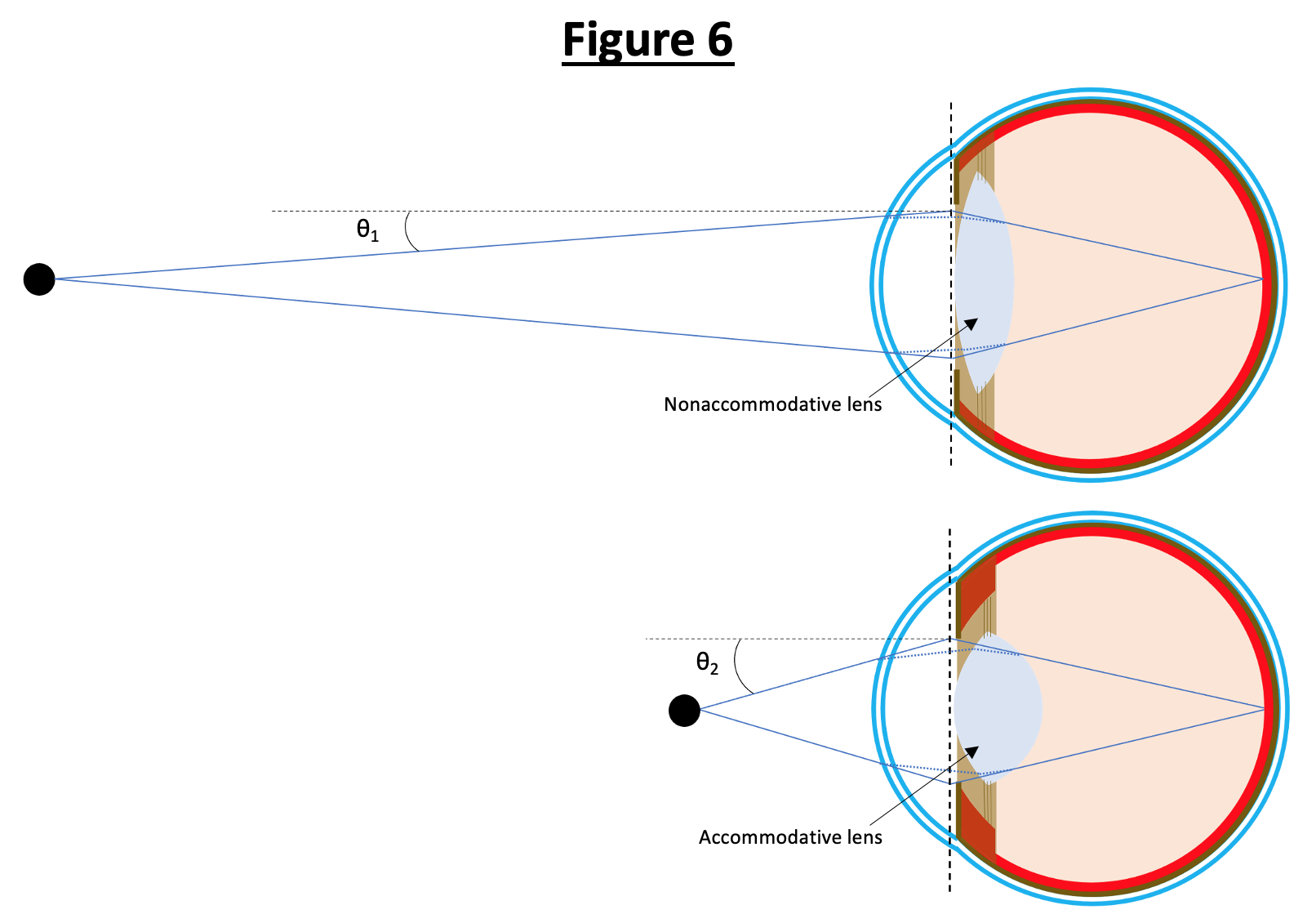
Angle of Incidence. This schematic demonstrates the different angles of incidence for objects of differing distances. Light rays from objects of greater distances have smaller angles of incidence (θ1) and thus require less refraction to focus on the retina, which is accomplished by the nonaccommodative lens (less spherical, less optic power) in the top eye. Light rays from objects of shorter distances have greater angles of incidence (θ2) and therefore require more refraction, which is accomplished by accommodation of the lens (more spherical, greater optical power) in the bottom eye. The black, dashed line represents the theoretical lens axis for the eye’s total optical power, while the blue-dotted lines represent the true path of light rays, first refracted by the cornea and later by the lens.
Illustrated and contributed by S Tenney.
References
Musa MJ, Zeppieri M. Subjective Refraction Technique: Astigmatic Dial. StatPearls. 2023 Jan:(): [PubMed PMID: 36943999]
Pai-Dhungat JV, Parikh F. Benjamin Franklin. The Journal of the Association of Physicians of India. 2014 Nov:62(11):73-4 [PubMed PMID: 26281492]
Norn M. Danish Ophthalmology - from start to 1865. Acta ophthalmologica. 2016 Mar:94(2):205-9. doi: 10.1111/aos.12775. Epub [PubMed PMID: 26899921]
Hallak J. Reflections on retinoscopy. American journal of optometry and physiological optics. 1976 May:53(5):224-8 [PubMed PMID: 937499]
Gurnani B, Kaur K. Autorefractors. StatPearls. 2023 Jan:(): [PubMed PMID: 35593828]
Mutti DO, Ver Hoeve JN, Zadnik K, Murphy CJ. The artifact of retinoscopy revisited: comparison of refractive error measured by retinoscopy and visual evoked potential in the rat. Optometry and vision science : official publication of the American Academy of Optometry. 1997 Jul:74(7):483-8 [PubMed PMID: 9293514]
Level 3 (low-level) evidenceFau C, Nabzo S. Copeland streak retinoscope. Archivos de la Sociedad Espanola de Oftalmologia. 2018 Oct:93(10):e70-e72. doi: 10.1016/j.oftal.2018.05.001. Epub 2018 Jun 12 [PubMed PMID: 29907350]
Ascaso Puyuelo FJ, Cristóbal Bescós JA. [About eyeglasses, glasses, lenses or spectacles]. Archivos de la Sociedad Espanola de Oftalmologia. 2002 Dec:77(12):689-91 [PubMed PMID: 12471517]
Bingöl-Kızıltunç P, Yürümez E, Atilla H. Does methylphenidate treatment affect functional and structural ocular parameters in patients with attention deficit hyperactivity disorder? - A prospective, one year follow-up study. Indian journal of ophthalmology. 2022 May:70(5):1664-1668. doi: 10.4103/ijo.IJO_2966_21. Epub [PubMed PMID: 35502047]
Kaur K, Gurnani B. Cycloplegic and Noncycloplegic Refraction. StatPearls. 2023 Jan:(): [PubMed PMID: 35593830]
Krishnacharya PS. Study on accommodation by autorefraction and dynamic refraction in children. Journal of optometry. 2014 Oct-Dec:7(4):193-202. doi: 10.1016/j.optom.2014.07.001. Epub 2014 Aug 15 [PubMed PMID: 25130066]
Level 2 (mid-level) evidenceHirota M, Takigawa R, Okabe C, Kato K, Nakagomi R, Sasaki K, Hayashi T. Refractive changes with post-rotatory nystagmus in healthy individuals. International ophthalmology. 2022 Feb:42(2):559-573. doi: 10.1007/s10792-021-02028-0. Epub 2021 Oct 19 [PubMed PMID: 34665371]
Ilechie AA, Addo NA, Abraham CH, Owusu-Ansah A, Annan-Prah A. Accuracy of Noncycloplegic Refraction for Detecting Refractive Errors in School-aged African Children. Optometry and vision science : official publication of the American Academy of Optometry. 2021 Aug 1:98(8):920-928. doi: 10.1097/OPX.0000000000001742. Epub [PubMed PMID: 34460453]
Tao Y, Li M, Tan J, Huang J, Cheng X, Xie P, Liu X, Zhou Q, Ouyang J. Effects of atropine and tropicamide on ocular biological parameters in children: a prospective observational study. BMC ophthalmology. 2023 Mar 13:23(1):96. doi: 10.1186/s12886-023-02840-5. Epub 2023 Mar 13 [PubMed PMID: 36915059]
Level 2 (mid-level) evidencePrincelle A, Hue V, Pruvost I, Potey C, Dubos F, Martinot A. [Systemic adverse effects of topical ocular instillation of atropine in two children]. Archives de pediatrie : organe officiel de la Societe francaise de pediatrie. 2013 Apr:20(4):391-4. doi: 10.1016/j.arcped.2013.01.012. Epub 2013 Feb 22 [PubMed PMID: 23433845]
Level 3 (low-level) evidenceMorales Ruiz H, Fernández-Agrafojo D, Cardona G. Correlation and agreement between the Mohindra and cycloplegic retinoscopy techniques in children. Archivos de la Sociedad Espanola de Oftalmologia. 2022 Jan:97(1):9-16. doi: 10.1016/j.oftale.2021.01.011. Epub 2021 Nov 23 [PubMed PMID: 35027148]
Kauser F, Gupta Y, Amitava AK, Saxena J, Raza SA, Masood A, Alam MS. Do all children need a cycloplegic refraction? A comparison of Mohindra's versus cycloplegic refraction. Indian journal of ophthalmology. 2020 Nov:68(11):2458-2461. doi: 10.4103/ijo.IJO_229_20. Epub [PubMed PMID: 33120640]
Nguyen AT, Wayne JL, Ravikumar A, Manny RE, Anderson HA. Accommodative accuracy by retinoscopy versus autorefraction spherical equivalent or horizontal meridian power. Clinical & experimental optometry. 2018 Nov:101(6):778-785. doi: 10.1111/cxo.12678. Epub 2018 Mar 25 [PubMed PMID: 29575034]
Tarczy-Hornoch K. Modified bell retinoscopy: measuring accommodative lag in children. Optometry and vision science : official publication of the American Academy of Optometry. 2009 Dec:86(12):1337-45. doi: 10.1097/OPX.0b013e3181be9d9c. Epub [PubMed PMID: 19797992]
Level 2 (mid-level) evidenceLocke LC, Somers W. A comparison study of dynamic retinoscopy techniques. Optometry and vision science : official publication of the American Academy of Optometry. 1989 Aug:66(8):540-4 [PubMed PMID: 2771345]
Rashid ZA, Moodley VR, Mashige KP. Diagnosis and management of keratoconus by eye care practitioners in Kenya. BMC ophthalmology. 2023 Jan 27:23(1):37. doi: 10.1186/s12886-023-02792-w. Epub 2023 Jan 27 [PubMed PMID: 36707782]
Chukwuyem EC, Musa MJ, Zeppieri M. Prescribing Glasses for Children. StatPearls. 2023 Jan:(): [PubMed PMID: 36256752]
Nguyen M, Blair K. Red Reflex. StatPearls. 2023 Jan:(): [PubMed PMID: 31985932]
Bakare PN, Gogate P, Magdum R, Phadke S, Maheshgauri R. Estimation of the Prevalence of Uncorrected Refractive Error and Other Ocular Morbid Conditions in School Children of Industrial Area in a Non-metro City in India. Cureus. 2022 Aug:14(8):e27972. doi: 10.7759/cureus.27972. Epub 2022 Aug 13 [PubMed PMID: 35978677]
Moreno JRA, Micó V, Albarrán Diego C. Subjective refraction using power vectors by updating a conventional phoropter with a Stokes lens for continuous astigmatic power generation. Ophthalmic & physiological optics : the journal of the British College of Ophthalmic Opticians (Optometrists). 2023 Sep:43(5):1029-1039. doi: 10.1111/opo.13181. Epub 2023 Jun 1 [PubMed PMID: 37264763]
Rossato M, Nart A, Messina G, Favro F, Rossato V, Rrutja E, Biancalana V. The Refraction Assessment and the Electronic Trial Frame Measurement during Standing or Sitting Position Can Affect Postural Stability. International journal of environmental research and public health. 2022 Jan 29:19(3):. doi: 10.3390/ijerph19031558. Epub 2022 Jan 29 [PubMed PMID: 35162580]
Wing GL. A makeshift retinoscopy rack. American journal of ophthalmology. 1980 Jan:89(1):142 [PubMed PMID: 7356780]
Schrimpf B, Dalby M, Mülhaupt M, Michel F, Holschbach A, Schiefer U, Ungewiss J. [Interactive training using a smartphone video retinoscope : Video article]. Der Ophthalmologe : Zeitschrift der Deutschen Ophthalmologischen Gesellschaft. 2020 Apr:117(4):384-388. doi: 10.1007/s00347-020-01054-0. Epub [PubMed PMID: 32052133]
Kaur K, Gurnani B. Subjective Refraction Techniques. StatPearls. 2023 Jan:(): [PubMed PMID: 35593807]
Aluyi-Osa G, Musa MJ, Zeppieri M. Jackson Cross Cylinder. StatPearls. 2023 Jan:(): [PubMed PMID: 36508527]
McCullough SJ, Doyle L, Saunders KJ. Intra- and inter- examiner repeatability of cycloplegic retinoscopy among young children. Ophthalmic & physiological optics : the journal of the British College of Ophthalmic Opticians (Optometrists). 2017 Jan:37(1):16-23. doi: 10.1111/opo.12341. Epub [PubMed PMID: 28030881]
Mutti DO. Sources of normal and anomalous motion in retinoscopy. Optometry and vision science : official publication of the American Academy of Optometry. 2004 Sep:81(9):663-72 [PubMed PMID: 15365385]
Manna P, Karmakar S, Bhardwaj GK, Mondal A. Accommodative spasm and its different treatment approaches: A systematic review. European journal of ophthalmology. 2023 May:33(3):1273-1286. doi: 10.1177/11206721221136438. Epub 2022 Nov 16 [PubMed PMID: 36384286]
Level 1 (high-level) evidenceKaur G, Thomas S, Jindal M, Bhatti SM. Visual Function and Ocular Status in Children with Disabilities in Special Schools of Northern India. Journal of clinical and diagnostic research : JCDR. 2016 Oct:10(10):NC01-NC04 [PubMed PMID: 27891365]
Musa MJ, Zeppieri M. Spectacle Correction of Ametropias. StatPearls. 2023 Jan:(): [PubMed PMID: 36251812]
Barcsay-Veres A, Szamosi A, Bausz M, Nagy ZZ. [The impact of district nurses in screening visual impairments]. Orvosi hetilap. 2023 Jan 22:164(3):88-95. doi: 10.1556/650.2023.32689. Epub 2023 Jan 22 [PubMed PMID: 36681996]