Introduction
Fundus photography is taking the image of the retina of the eye with a fundus camera. Fundus photography is important for diagnosing and treating various posterior segments and other ocular diseases. The illumination and reflectance of the retina occur through the common optical path, i.e., the pupil. Jackman and Webster were the first to publish retinal photographs in 1886.[1] Carl Zeiss was the first commercially available fundus camera in 1926.[1] Hansell and Beeson attached the electronic flash tube enabling light to be directed through the pupil.[2]
Over time, sharper images, non-mydriatic cameras, pupil tracking, smart-phone fundus imaging, ultrawide field fundus imaging, and artificial intelligence (AI) integrated into online or offline photography have resulted from technical advances in retinal imaging.
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
The retina is the neurosensory part of the eye where light impulses from an object are converted to electoral impulses that travel to the brain, and the person receives the details of the object. The imaging of the retina poses difficulty because the retina must be illuminated and imaged simultaneously through a narrow pathway, i.e., the pupil.[3]
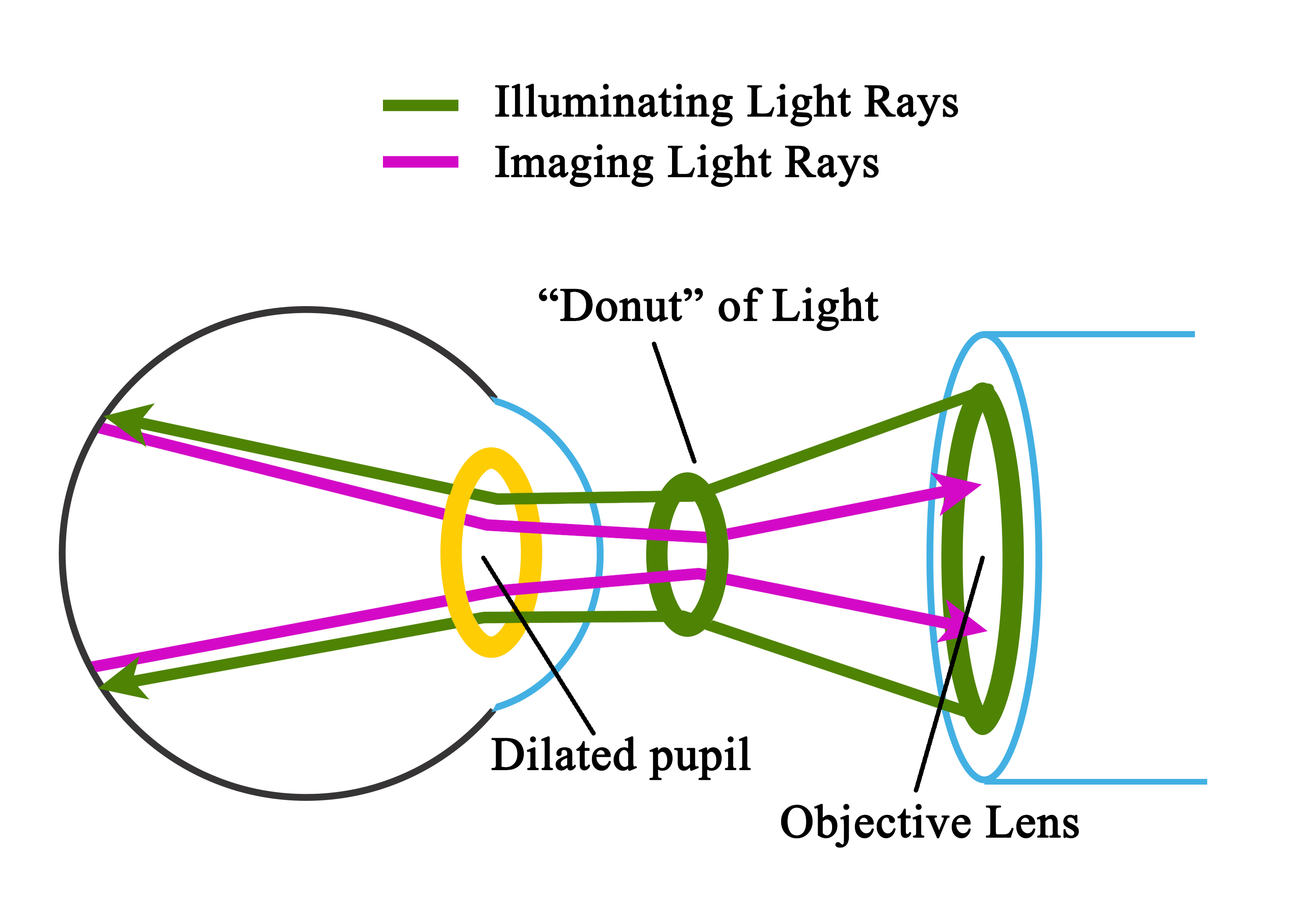
The retina is a minimally reflective surface; hence, the back reflections from the retinal surface are lesser than the combined reflections from the illuminating and imaging systems. The fundus camera uses the principle of reflex-free indirect ophthalmoscopy. Traditional fundus cameras use the rim of the pupillary aperture for illumination and the center of the pupil for imaging (Figure-1). With this, the overlapping reflections are minimized.
Indications
Any pathology of the posterior segment of the eye can be detected with a fundus camera. The common indications are enumerated in the following table.
|
Serial No. |
Sub-Specialties |
Conditions including |
|
1 |
Vitreo-Retinal diseases |
|
|
|
|
Age-related macular degeneration |
|
|
|
Retinal vascular occlusions[8] |
|
|
|
|
|
|
|
Retinopathy of prematurity |
|
|
|
Tumors of the eye, vascular lesions[11] |
|
|
|
Complications of the anterior segment surgeries like cataractous lens drop and intraocular lens (IOL) drop |
|
|
|
Macular pathologies like a macular hole, epiretinal membrane, and macular edema[12][13][14] |
|
|
|
Retinal detachment[15] and choroidal detachment |
|
|
|
Vitreous abnormalities like vitreous hemorrhage, vitreous cyst, and asteroid hyalosis[16][17] |
|
2 |
Glaucoma |
|
|
|
|
Retinal nerve fiber layer damage resulting from glaucoma |
|
3 |
Uvea |
Posterior uveitis like vasculitis, chorioretinitis, choroidal granuloma,[21] secondary deposits from primary malignancy elsewhere |
|
|
|
Intermediate uveitis like snow banking and snow-balls[22][23] |
|
4 |
Neuro-ophthalmology |
Anterior ischemic optic neuropathy, optic atrophy, and morning glory syndrome[24] |
|
5 |
Anterior segment and ocular adnexa (Figure) |
Contraindications
Absolute contraindications: There are no absolute contraindications to fundus imaging.
Possible difficulties during fundus photography:
- Musculoskeletal diseases may not allow the patient to keep the chin in the chin rest.
- Severe photophobia in conditions like an acute ocular injury may cause blepharospasm and increased lacrimation creating a challenge for a good capture.
Equipment
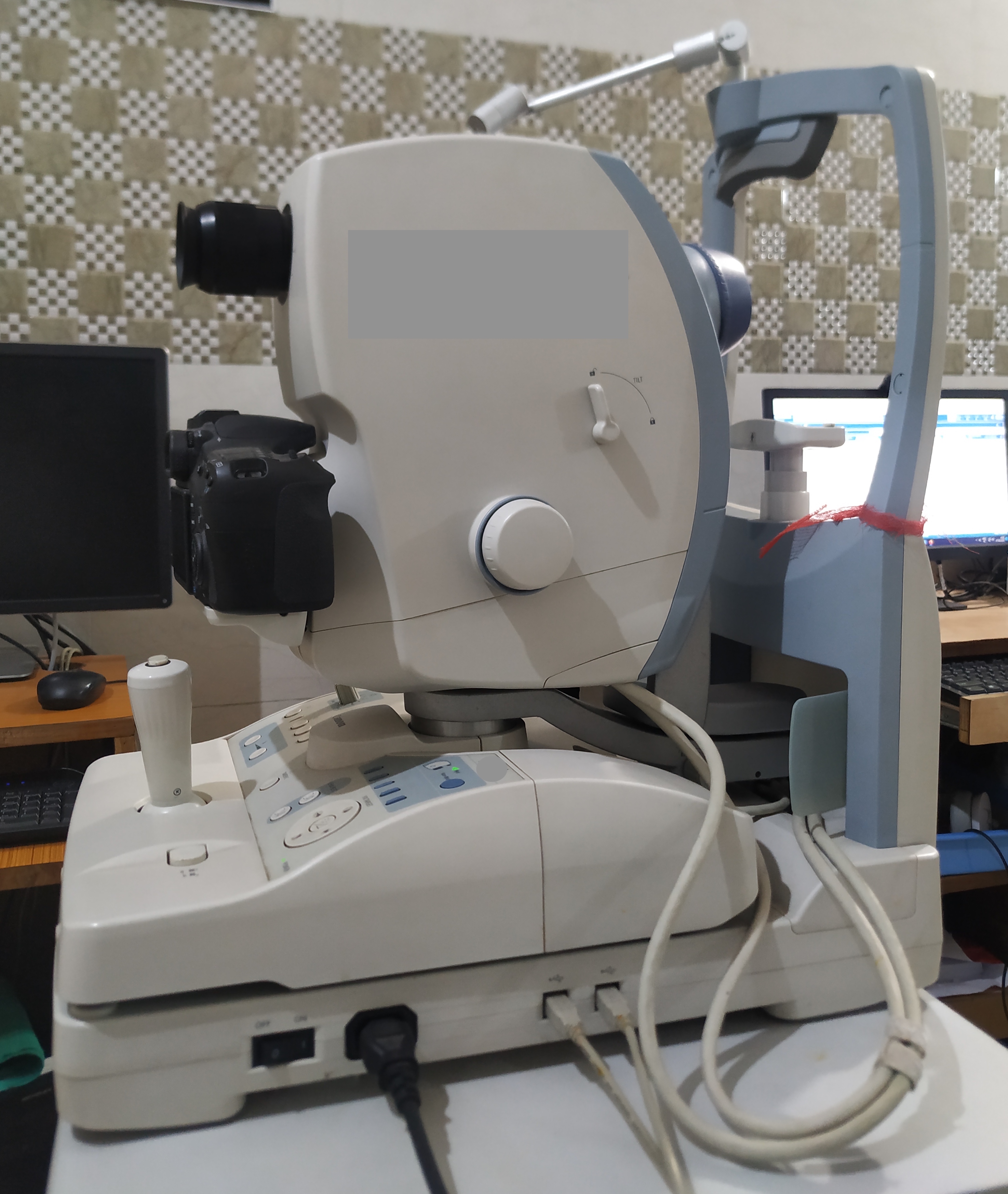
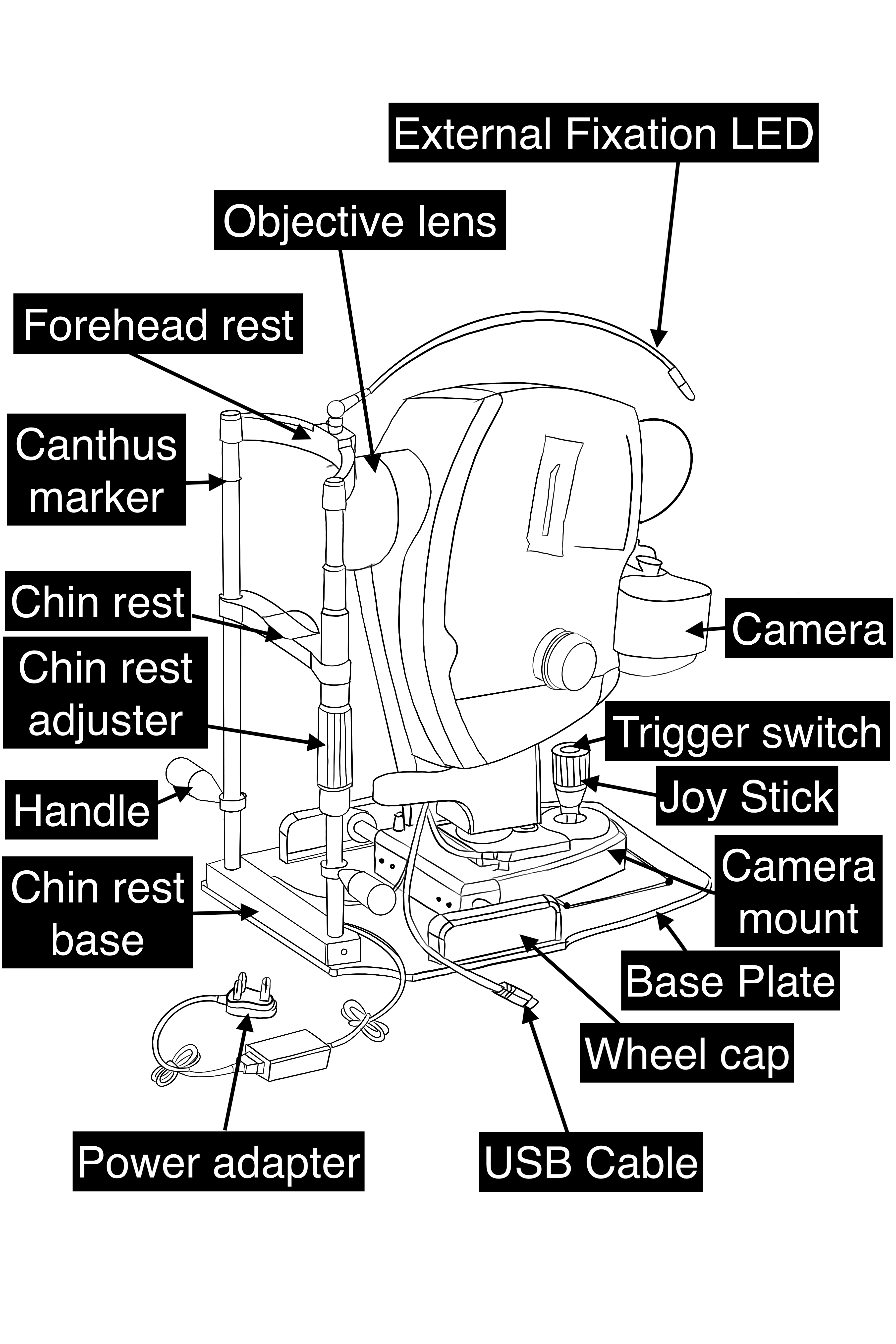
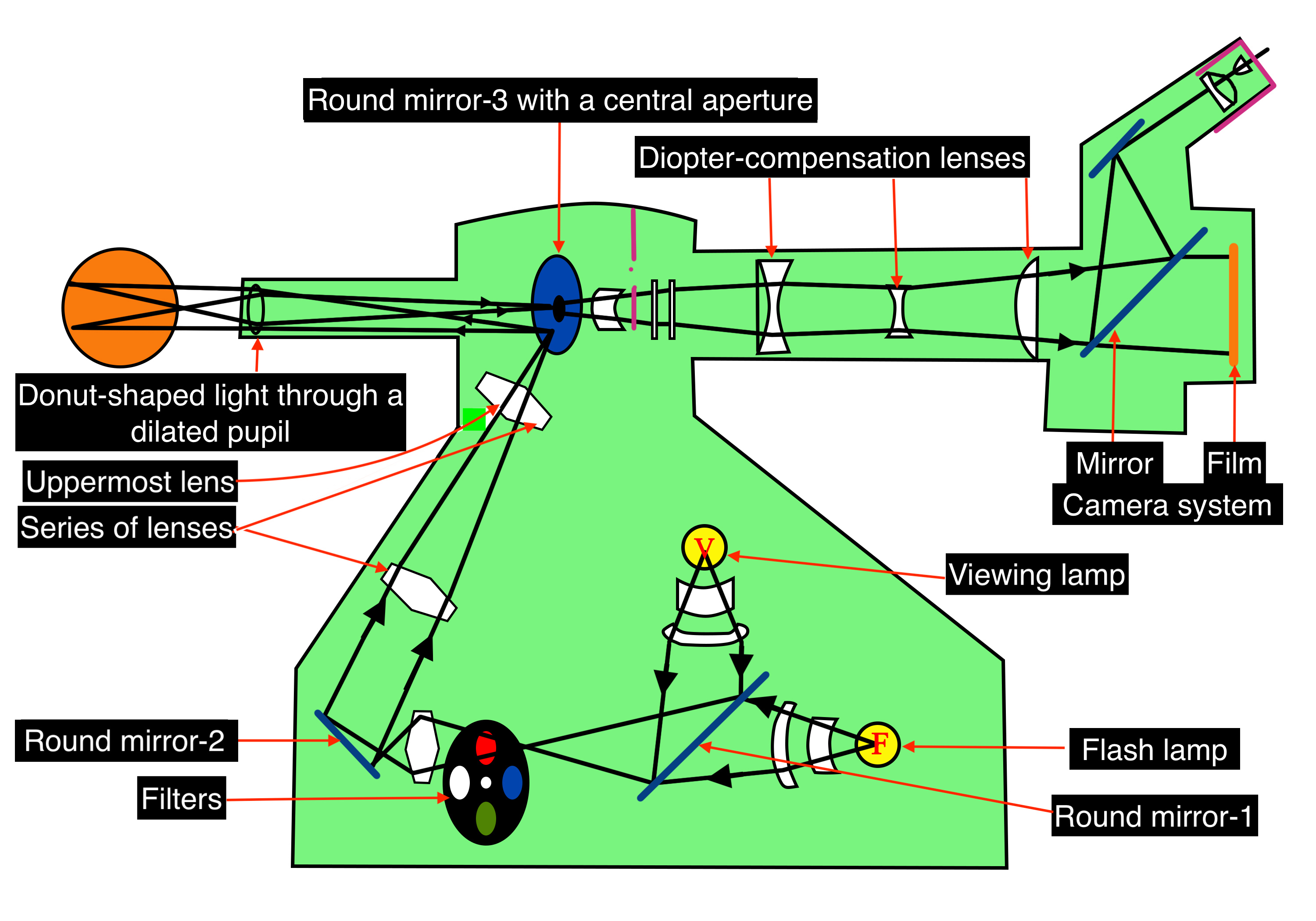
A fundus camera is a complex system with multiple lenses and a camera utilizing the principle of indirect ophthalmoscope (Figure-2). The parts of a typical fundus camera are shown in the figure (Figure-3).
Optics of Fundus Camera
Light from the viewing lamp is projected onto a round mirror (Figure-4, round mirror-1) and then through a set of filters (Figure-4, filters) onto another round mirror (Figure 4, round mirror -2). The light is reflected from the mirror (round mirror-2) to a series of lenses (Figure 4, series of lenses).
Due to the presence of a mask in the uppermost lens (Figure 4, uppermost lens), the light is finally focused as a donut-shaped beam. This donut-shaped light beam falls on another round mirror with a central aperture (Figure-4, round mirror-3 with a central aperture), and the reflection exits the camera system through the objective lens and enters through the cornea into the eye (Figure-4, donut-shaped light through a dilated pupil), the photo of which is to be taken.
When both the illuminating rays through the pupillary border and the image at the center of the pupil are correctly aligned, the imaging rays exit through the center of the pupil, i.e., the central non-illuminated portion of the donut of the light (Figure-1, Figure-4, donut-shaped light through a dilated pupil)
The imaging rays pass through the central aperture of the mirror as mentioned above (Figure-4, round mirror-3 with a central aperture), through the astigmatic correction and diopter compensation lenses (Figure-4, diopter compensation lenses), then back to the single-lens reflex camera system (Figure-4, camera system).
The commonly used table-top fundus cameras include iCam (Optovue Inc. Fremont, CA), 3nethra (Forus Inc. Bengaluru, India), digital retinography system (dRS, CenterVue, Padova, Italy), EasyScan (iOptics, Den Haag, The Netherlands), TRCNW8Fplus (Topcon, Tokyo, Japan), Visucam (Zeiss, Oberkochen, Germany), Nonmyd7 (Kowa, Torrance, CA), and Canon CR-2 ( Canon, Tokyo, Japan).[1]
Over time, there have been many upgrades to the traditional table-top fundus camera. These are as described below.
Wide-field and ultra-widefield fundus cameras:
Wide-field fundus imaging refers to taking retinal images of more than 50 degrees.[25] Ultra-wide-field fundus imaging was defined by DRCR.net (diabetic retinopathy clinical research network) to be more than 100 degrees of field of area.[26]
Recently a consensus nomenclature defined wide-field imaging (WFI) to be a single captured retinal image centered on the fovea and extending beyond the posterior pole but posterior to the vortex vein ampullae in all the four quadrants. Ultra-wide-field image (UWFI) is a single captured retinal image that captures retinal images anterior to the vortex vein ampullae in all four quadrants.[27]
|
WFI and UWFI Systems |
Contact/ Non-contact |
Field of area |
Method of imaging |
Advantages |
Disadvantages |
|
Equator-plus camera [by O Pomerantzeff][28]
|
Contact |
148 degrees from the nodal point |
Patient in sitting position |
One of the earlier introduced UWFI fundus cameras is equipped with interference filters. |
The peripheral illumination through the peripheral cornea reduces high resolution and causes brilliance/bright artifacts at the peripheral retina.
|
|
RetCam (Clarity Medical Systems, Inc., Pleasanton, CA, USA).
|
Contact |
130- degree |
The patient is in the supine position. It is mainly used for retinopathy of prematurity (ROP) babies. |
Contact ultra-widefield fundus camera for a neonatal eye examination. The machine can be transported to neonatal intensive care units along with the ROP team. The images can be sent to the base hospital via the internet/cloud. |
High cost of the machine. The learning curve for the personnel capturing the images. |
|
Optos® camera (Optos PLC, Dunfermline, UK)
|
Non-contact |
Up to 200 degrees |
Sitting position or flying baby position |
A non-contact ultra-widefield fundus camera has the widest field of view, i.e., up to 200 degrees. UWF Fundus auto-fluorescence (FAF) can be done. Upgraded versions have features like UWF fundus fluorescein angiography (FFA), indocyanine green angiography (ICGA), and UWF optical coherence tomography (OCT).[23][15][29][30] |
High cost of the machine. cSLO images are not true color fundus images. |
|
Heidelberg Spectralis with the Staurenghi lens (Ocular Staurenghi 230 SLO Retina Lens; Ocular Instruments Inc, Bellevue, WA, USA)
|
Non-contact and Contact |
105 degrees in non-contact [31]
150 degrees in contact Staurenghi lens
|
The sitting position of the patient |
Both non-contact and contact fundus imaging modes are available.
|
High cost of the machine. cSLO images are not true color fundus images. |
|
Clarus® 500 (Carl Zeiss Meditec)
|
Non-Contact |
Single capture 133 degrees, Montage 200 degrees |
The sitting position of the patient |
Non-contact ultra-widefield True color imaging, auto-fluorescence, Blue, Green, Infrared, and FFA can be done.
|
High cost of the machine. |
|
Mirante device by Nidek (Nidek Co., Ltd, Gamogori, Japan)
|
Non-Contact |
163° ultra-wide field imaging with a single image capture
|
The sitting position of the patient |
Color fundus photo, FFA, ICG, FAF, retro mode imaging, OCT, angio-scan OCT-angiography, and anterior segment OCT.
|
High cost of the machine. cSLO images are not true color fundus images. |
|
Eidon (CenterVue, Italy) |
Non-contact |
Single capture 90 degrees maximum (measured from the center of the eye), up to 160 degrees in a mosaic fashion. |
The sitting position of the patient |
True color fundus images with advantages of cSLO images. Infra-red and red-free images are available. |
The field of view in a single capture is 90 degrees maximum, which is not UWF imaging |
The Optos non-contact ultra-widefield pseudocolor fundus camera uses a scanning laser ophthalmoscope (SLO), two laser light sources of wavelengths 532 nm (green) and either 633 nm or 635 nm (red), and an ellipsoidal mirror with two conjugal focal points which enables capturing the retinal images up to 200 degrees.[32]
Advantages of WFI and UWFI
- Better resolution
- Possible for image acquisition in non-compliant young pediatric patients
- Patients with undilated pupils and hazy media due to cataracts or other diseases
- Simultaneous imaging of central and peripheral retina; use of UWF FFA to evaluate peripheral retinal ischemia and new vessels in patients with familial exudative vitreoretinopathy, diabetic macular edema, and other vascular complications.
- Counseling and education of the patients
Confocal scanning laser ophthalmoscope (cSLO) based fundus cameras: The confocal scanning laser ophthalmoscope (cSLO) uses laser light instead of a flashlight to illuminate the retina. This reduces the scatter of light in the images acquired, forming a sharp, high-contrast image located within the focal plane.
Currently, the imaging systems using cSLO-based fundus imaging are increasingly used. The common cSLO-based fundus cameras include Optos, the non-contact ultra-widefield fundus camera with 200 degrees field of view. This imaging system has UWF fundus imaging, choroidal imaging, fundus autofluorescence (FAF), fundus fluorescein angiography (FFA), indocyanine green (ICG) angiography, and optical coherence tomography (OCT) imaging.[33]
Heidelberg Spectralis multi-color imaging has additional features like OCT, OCT-angiography, and fundus auto-fluorescence (FAF).
Using Mirante, the cSLO-based multimodal imaging platform, in addition to the UWF fundus photo, the additional features like FFA, ICGA, FAF, and retro mode imaging for visualizing pathologies deeper than the retinal pigment epithelium (RPE), and detecting pathologic changes in the choroid, OCT, OCT-Angiography, and an anterior segment OCT with an additional adapter can be performed.
Eidon (CenterVue) combines the cSLO with the conventional fundus imaging (white light emitting diode/LED) system to give true color-wide field fundus images.
Red-free fundus photography (RFFP): The red-free fundus photography (RFFP) is monochromatic retinal imaging that uses gree contrast filters and enables an excellent view of the retina as the peak spectral sensitivity of the human eye falls in the green-yellow range of the spectrum. Retinal vasculature and nerve fiber layers are better seen in RFFP. The RFFP image is routinely taken as a baseline image before the FFA.[34]
Fundus autofluorescence (FAF): The FAF uses the fluorescent properties of the fluorophores. The important fluorophores in the retina are lipofuscin and melanin. Lipofuscin is a byproduct of the lysosomal breakdown of the outer photoreceptor segments within the RPE. The concentration of the lipofuscin pigments increases from the equator of the retina to the posterior pole, except for the fovea.
Lipofuscin absorbs light in the blue spectrum with a wavelength of 470 nm and emits the light in the yellow-green spectrum at a wavelength of 600 to 610 nm. Lipofuscin-based autofluorescence is known as shortwave autofluorescence (SWAF) or blue auto-fluorescence (BAF). Melanin has an excitation wavelength of 787 nm and an emission wavelength at a near-infrared wavelength. Melanin-based autofluorescence is known as near-infrared autofluorescence (NIRAF).[35]
In BAF, the fovea is darker (hypo-autofluorescent) due to less lipofuscin at the fovea. In contrast, in NIRAF, the fovea is brighter (hyper-autofluorescent) due to the highest concentration of melanin in this region. FAF has diagnostic and prognostic utility in various diseases like central serous chorioretinopathy (CSCR), age-related macular degeneration (ARMD), retinal dystrophies, and uveitic entities like choroiditis. FAF images of the retina can be taken in a conventional fundus camera with a 50 to 55-degree field of view with the facility of FAF. UWF FAF is available in Optos, Heidelberg Spectralis, Mirante, and Clarus.
Multi-color imaging: Multi-color imaging (MCI) uses cSLO to capture three reflectance images simultaneously 1) blue reflectance (BR; 488 nm), (2) green reflectance (GR; 515 nm), and the (3) near-infrared reflectance (IR; 820 nm). The blue reflectance enables the details of the inner retina, the green reflectance details the retinal blood vessels and exudations in the retinal layers, if any, and the infrared reflectance details the outer retina, including the RPE abnormalities. The near-infrared reflectance has been most helpful in imaging the choroidal nodules in neurofibromatosis type 1, and these nodules have been correlated with the presence of Lisch nodules of the iris.[36]
The blue reflectance is better than the green reflectance for detecting dissociated optic nerve fiber layer after internal limiting membrane peeling.[37] Multi-color images are captured at both 30 degrees and 55 degrees in the Heidelberg Spectralis machine. In the Mirante imaging system, 163 degrees UWF multi-color images with single image capture are possible. MCI has been beneficial in diagnosing and managing diseases like ARMD, diabetic retinopathy, vitreoretinal interface disorders, retinal vein occlusions, and retinal dystrophies.[38]
Multi-color imaging is useful in detecting vitreoretinal interface abnormalities better than posterior uveitic lesions like retinochoroiditis and retinal lesions like intraretinal hemorrhages.[39]
Smartphone-Based fundus cameras: Recently, smartphone-based fundus imaging has been proven to be a low-cost alternative to standard fundus photography. It can capture images in both the dilated and undilated pupils. It has an immense role in screening diseases like DR, ARMD, ROP, and Glaucoma. It is becoming a boon for teleophthalmology.[40] Low-cost fundus cameras have been developed to help screen for retinal diseases in remote parts of the world.[41]
Smartphone-based fundus photography has been effective in detecting DR.[42] In smartphone-based fundus photography, the diagnostic accuracy for PDR is 92%, and that for referable DR is 91%.[43]
Some of the FDA-approved smartphone-based fundus imaging systems include Welch Allyn iExaminer (Welch Allyn, Skaneateles Falls, NY), Remidio Fundus on Phone device (Remidio Innovative Solutions, Bangalore, India), D-Eye, and iNview (Volk Optical, Inc.). Recently, the integration of artificial intelligence (AI) has increased the capability of fundus imaging, especially in the screening of DR.[44]
IDx-DR is an autonomous AI system that has been approved by the USFDA for the detection of DR stages more than mild DR or absence of DR. It has an imageability rate of 96.1%, a sensitivity of 87.2%, and a specificity of 90.7%.[45] USFDA cleared EyeArt (Eyenuk) for autonomous detection of more than mild DR and vision-threatening DR.[4]
Personnel
Fundus photography by a fundus camera can be performed by an ophthalmologist, optometrist, paramedical personnel, mid-level ophthalmic practitioner (MLOP), or anyone trained in ophthalmic photography.
Preparation
Before obtaining the fundus images, the patient should be informed about the procedure and the purpose of the test. The chin rest, forehead rest, and the holding support of the camera should be cleaned with an alcohol swab to maintain hygiene. If the patient wears a spectacle, they should remove the spectacle. The patient should sit and position themselves in the chinrest and forehead rest comfortably. Most fundus cameras need pupillary dilation for an optimal image free of artifacts.
Technique or Treatment
A photo of one eye of the patient is taken at a time. First, align the circle on the screen with the patient’s iris and pupil. Adjust the height to make the three white dots in a symmetric position. Then focus on the retina of the patient. Ask the patient to focus on the green light they see. Adjust the joystick forwards, backward, and sideways to get a sharper view of the two dots on the three o clock and nine o clock positions (to ensure the optimal distance of the camera from the eye) or a sharper image of the reticules.
There is an indicator indicating the good focus of the retina (two vertical lines which have to be aligned in some cameras). For manual capture, the eyepiece must be correctly set. The photographer must wear the refractive error corrections, if any. The accommodation of the photographer must be at rest. When the reticules are sharper, and the view of the retina is sharper, the button is pressed to capture the image (Figure-5). Fundoscopy has been taught to students using virtual platforms, which proved useful, especially during the COVID pandemic.[46]
Stereophotography uses two images taken from the right and left, which are then viewed with a stereo viewer. Optional lenses must be employed for focusing anterior objects (mid-vitreous, anterior segment). To focus posterior objects or the retina in pathological myopia, minus lenses have to be added. For extremes of refractive errors (around +15 diopter or -15 diopters), the autofocus function of the fundus camera may not work, and manual focusing should be used to focus the retina.
Complications
As a non-invasive technique, fundus cameras do not have complications. However, there is a risk of cross-infection from patients with active eye infections like conjunctivitis to the other patients who undergo fundus imaging in the same camera. Also, the strong flashlight might not be tolerable to some patients with photophobia.
Artifacts in Fundus Photography
Multiple artifacts (figure) may occur during the use of the fundus camera.
- The orange or bright crescent at the margin of the photo is due to the illuminated iris, specifically in a poorly dilated pupil. The joystick should be moved in the opposite direction so that the cone of light passes through the pupil and does not hit the iris.
- Eyelashes create hazy veils over some areas of the picture. The eyelids should be held open in such cases so that lashes do not obstruct the light or come in the path of the light.
- If the camera is very near or far from the eye, there is a haze and loss of detail. The distance between the eye and camera should be optimal to get the deepest tone of color of the fundus.
- A smudge in the system will produce a spot at the same place in the photos taken at different times. This is usually due to the touch of the objective lens by the patient's face, nose, or eyelashes, which resolves after removing the dirt or smudge from the system.
Clinical Significance
Fundus cameras are used for fundus photography. Fundus photography is useful for diagnosing, educating patients, counseling, monitoring, and forecasting many ophthalmic conditions, notably DR, ARMD, Retinal vascular disorders, ROP, and glaucoma (Figures).
The traditional tabletop fundus cameras with a 50-degree field of view can detect the pathology of the posterior pole of the eye. The wide field and ultra-widefield fundus cameras are helpful in the imaging of retinal pathology beyond the equator of the retina. The presence of predominantly peripheral lesions in DR can be detected with the help of UWFI and carries a higher risk of progression to PDR.[47]
The contact ultra-widefield fundus camera for a neonatal eye examination (RetCam) has been used extensively for the diagnosis and follow-up of neonates at risk with and suffering from retinopathy of prematurity (ROP). This camera is portable and can be taken to remote places.
Advances in Fundus Imaging and Future Perspectives
Bog data, machine learning, and artificial intelligence are promising in improving healthcare.[48] The integration of AI into the fundus cameras has shown good accuracy for the detection of diseases like DR. Machine learning algorithms using preoperative fundus photography along with some other preoperative data, including anterior chamber depth, central corneal depth, age, planned ablation thickness, has been shown to identify at-risk eyes for postoperative myopic regression after refractive surgery.[49]
Deep learning algorithms using fundus photographs have been used to predict cerebral white matter hyperintensity in magnetic resonance imaging (MRI) scans.[50] A deep learning framework for the earlier detection of DR from fundus images has been developed, and it could differentiate the healthy and harmful images with 95.6% precision.[51] Studies using AI to establish the role of fundus photos, OCT, and external eye photography with systemic diseases and parameters show promising results.[52]
AI for the screening of DR has shown a lot of promise. These findings underscore the prospective role of AI integrated fundus imaging in the screening, diagnosis, and management of different retinal diseases.[53]
Combining OCT imaging with fundus photography has been shown to increase the efficacy of glaucoma screening.[54] This combination has also been shown to effectively diagnose cases of high myopia with retinopathy.[55] This approach demonstrates the beneficial role of multi-modal imaging. Studies on handheld fundus cameras are on the rise. Comparative studies have shown that the handheld fundus camera effectively diagnoses referrable cases of DR.[56]
Similarly, smartphone-based fundus imaging is on the rise and is most useful for teleophthalmology. However, in detecting ROP, though the smartphone-based cameras provide a moderate agreement for the detection of the presence or absence of plus disease, they failed to identify the stages and zones of the disease.[57]
Enhancing Healthcare Team Outcomes
The fundus camera plays an important role in diagnosing and managing ophthalmic diseases. Apart from the ophthalmologists, optometrists, ophthalmic photographers, and paramedical workers are involved in taking images in the fundus cameras. While doing fundus fluorescein angiography or indocyanine green angiography, the nurses should be aware of the possible side effects of the dye-related invasive procedure.[29][30]
Coordination between all the team members and caregivers and updating their knowledge about the fundus photography and procedures related to the fundus cameras is crucial.
Nursing, Allied Health, and Interprofessional Team Interventions
Nurses are involved in the procedure of fundus photography. Their support during any side effects of the procedures like fundus fluorescein angiography is vital. They should possess strong knowledge regarding the emergency medicines needed during any complications related to the investigations.
Retinal diseases are associated with various systemic illnesses like diabetes, systemic hypertension, and systemic drug toxicity. Clinical history provided by colleagues from specialties other than ophthalmology will help interpret the fundus images.
Nursing, Allied Health, and Interprofessional Team Monitoring
The fundus camera is used for non-invasive procedures like fundus photography and invasive procedures like FFA. Monitoring the quality of images taken, the indications for which the images are taken, a note of any adverse events, and their management is crucial for operating a fundus photography unit. Nurses, allied health personnel, ophthalmologists, and doctors from other specialties can use the fundus camera. An audit and monitoring of the events happening in the fundus photography unit are crucial for the smooth functioning of the unit.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Panwar N, Huang P, Lee J, Keane PA, Chuan TS, Richhariya A, Teoh S, Lim TH, Agrawal R. Fundus Photography in the 21st Century--A Review of Recent Technological Advances and Their Implications for Worldwide Healthcare. Telemedicine journal and e-health : the official journal of the American Telemedicine Association. 2016 Mar:22(3):198-208. doi: 10.1089/tmj.2015.0068. Epub 2015 Aug 26 [PubMed PMID: 26308281]
Level 3 (low-level) evidenceHANSELL P, BEESON EJ. Retinal photography in colour. The British journal of ophthalmology. 1953 Feb:37(2):65-9 [PubMed PMID: 13032356]
DeHoog E, Schwiegerling J. Fundus camera systems: a comparative analysis. Applied optics. 2009 Jan 10:48(2):221-8 [PubMed PMID: 19137032]
Level 2 (mid-level) evidenceShukla UV, Tripathy K. Diabetic Retinopathy. StatPearls. 2024 Jan:(): [PubMed PMID: 32809640]
Mishra C, Tripathy K. Retinal Traction Detachment. StatPearls. 2024 Jan:(): [PubMed PMID: 32644378]
Tripathy K, Chawla R, Vohra R. Evaluation of the fundus in poorly dilating diabetic pupils using ultrawide field imaging. Clinical & experimental optometry. 2017 Nov:100(6):735-736. doi: 10.1111/cxo.12484. Epub 2016 Oct 5 [PubMed PMID: 27704602]
Tripathy K, Sharma YR, R K, Chawla R, Gogia V, Singh SK, Venkatesh P, Vohra R. Recent advances in management of diabetic macular edema. Current diabetes reviews. 2015:11(2):79-97 [PubMed PMID: 25801496]
Level 3 (low-level) evidenceTripathy K, Mazumdar S, Sarma B. Central retinal arterial occlusion in a patient with pyoderma gangrenosum. Indian journal of ophthalmology. 2018 Jul:66(7):1019-1021. doi: 10.4103/ijo.IJO_1229_17. Epub [PubMed PMID: 29941761]
Elnahry AG, Tripathy K. Gyrate Atrophy of the Choroid and Retina. StatPearls. 2024 Jan:(): [PubMed PMID: 32491691]
Jena S, Tripathy K, Chawla R, Mansour AM. Ultrawide field imaging to document the progression of gyrate atrophy of the choroid and retina over 5 years. BMJ case reports. 2021 Aug 17:14(8):. doi: 10.1136/bcr-2021-244695. Epub 2021 Aug 17 [PubMed PMID: 34404670]
Level 3 (low-level) evidenceRavani R, Patel C, Tripathy K. Optical coherence tomography of racemose angioma. Clinical case reports. 2020 Jul:8(7):1299-1300. doi: 10.1002/ccr3.2841. Epub 2020 Apr 12 [PubMed PMID: 32695379]
Level 3 (low-level) evidenceTripathy K, Sharma YR, Chawla R, Jain S, Behera A. Ultra-wide Field Imaging of an Operated Macular Hole in Gyrate Atrophy. Journal of ophthalmic & vision research. 2016 Jul-Sep:11(3):336-7. doi: 10.4103/2008-322X.188404. Epub [PubMed PMID: 27621797]
Majumdar S, Tripathy K. Macular Hole. StatPearls. 2023 Jan:(): [PubMed PMID: 32644626]
Tripathy K. Cystoid Macular Edema in Retinitis Pigmentosa with Intermediate Uveitis Responded Well to Oral and Posterior Subtenon Steroid. Seminars in ophthalmology. 2018:33(4):492-493. doi: 10.1080/08820538.2017.1303521. Epub 2017 Mar 29 [PubMed PMID: 28353369]
Tripathy K, Chawla R, Wadekar BR, Venkatesh P, Sharma YR. Evaluation of rhegmatogenous retinal detachments using Optos ultrawide field fundus fluorescein angiography and comparison with ETDRS 7 field overlay. Journal of current ophthalmology. 2018 Sep:30(3):263-267. doi: 10.1016/j.joco.2018.06.006. Epub 2018 Jul 3 [PubMed PMID: 30197958]
Mishra C, Tripathy K. Asteroid Hyalosis. StatPearls. 2023 Jan:(): [PubMed PMID: 32119262]
Tripathy K. Asteroid Hyalosis. The New England journal of medicine. 2018 Aug 23:379(8):e12. doi: 10.1056/NEJMicm1712355. Epub [PubMed PMID: 30134134]
Mahabadi N, Foris LA, Tripathy K. Open Angle Glaucoma. StatPearls. 2024 Jan:(): [PubMed PMID: 28722917]
Zeppieri M, Tripathy K. Pigment Dispersion Glaucoma. StatPearls. 2024 Jan:(): [PubMed PMID: 35593820]
Okonkwo ON, Tripathy K. Posner-Schlossman Syndrome. StatPearls. 2024 Jan:(): [PubMed PMID: 35015437]
Chawla R, Venkatesh P, Tripathy K, Chaudhary S, Sharma SK. Successful Management of Proliferative Diabetic Retinopathy and Multiple Choroidal Tubercles in a Patient with Miliary Tuberculosis. Journal of ophthalmic & vision research. 2018 Apr-Jun:13(2):210-211. doi: 10.4103/jovr.jovr_203_16. Epub [PubMed PMID: 29719654]
Chauhan K, Tripathy K. Pars Planitis. StatPearls. 2024 Jan:(): [PubMed PMID: 28613790]
Tripathy K, Chawla R, Venkatesh P, Vohra R, Sharma YR, Gogia V, Jain S, Behera A. Ultra-wide Field Fluorescein Angiography in Retinitis Pigmentosa with Intermediate Uveitis. Journal of ophthalmic & vision research. 2016 Apr-Jun:11(2):237-9. doi: 10.4103/2008-322X.183929. Epub [PubMed PMID: 27413510]
Gupta A, Singh P, Tripathy K. Morning Glory Syndrome. StatPearls. 2024 Jan:(): [PubMed PMID: 35593815]
Witmer MT, Kiss S. Wide-field imaging of the retina. Survey of ophthalmology. 2013 Mar-Apr:58(2):143-54. doi: 10.1016/j.survophthal.2012.07.003. Epub 2013 Jan 29 [PubMed PMID: 23369515]
Level 3 (low-level) evidenceGhasemi Falavarjani K, Tsui I, Sadda SR. Ultra-wide-field imaging in diabetic retinopathy. Vision research. 2017 Oct:139():187-190. doi: 10.1016/j.visres.2017.02.009. Epub 2017 Jul 20 [PubMed PMID: 28688908]
Choudhry N, Duker JS, Freund KB, Kiss S, Querques G, Rosen R, Sarraf D, Souied EH, Stanga PE, Staurenghi G, Sadda SR. Classification and Guidelines for Widefield Imaging: Recommendations from the International Widefield Imaging Study Group. Ophthalmology. Retina. 2019 Oct:3(10):843-849. doi: 10.1016/j.oret.2019.05.007. Epub 2019 May 13 [PubMed PMID: 31302104]
Pomerantzeff O. Equator-plus camera. Investigative ophthalmology. 1975 May:14(5):401-6 [PubMed PMID: 1126828]
Ruia S, Tripathy K. Fluorescein Angiography. StatPearls. 2024 Jan:(): [PubMed PMID: 35015403]
Muraleedharan S, Tripathy K. Indocyanine Green (ICG) Angiography. StatPearls. 2024 Jan:(): [PubMed PMID: 35593804]
Tripathy K, Ying H, Maldonado Cerda A, Filipowicz A, Kaya M, Seymen Z, Anesi SD, Chang PY, Foster CS. Widefield Fundus Fluorescein Angiography Features of Uveitis Associated with Juvenile Idiopathic Arthritis. Ocular immunology and inflammation. 2022 May 19:30(4):829-838. doi: 10.1080/09273948.2020.1834586. Epub 2020 Dec 2 [PubMed PMID: 33264037]
Kato Y, Inoue M, Hirakata A. Quantitative comparisons of ultra-widefield images of model eye obtained with Optos(®) 200Tx and Optos(®) California. BMC ophthalmology. 2019 May 17:19(1):115. doi: 10.1186/s12886-019-1125-y. Epub 2019 May 17 [PubMed PMID: 31101026]
Yannuzzi LA, Ober MD, Slakter JS, Spaide RF, Fisher YL, Flower RW, Rosen R. Ophthalmic fundus imaging: today and beyond. American journal of ophthalmology. 2004 Mar:137(3):511-24 [PubMed PMID: 15013876]
Bennett TJ, Barry CJ. Ophthalmic imaging today: an ophthalmic photographer's viewpoint - a review. Clinical & experimental ophthalmology. 2009 Jan:37(1):2-13. doi: 10.1111/j.1442-9071.2008.01812.x. Epub 2009 Sep 23 [PubMed PMID: 18947332]
Yung M, Klufas MA, Sarraf D. Clinical applications of fundus autofluorescence in retinal disease. International journal of retina and vitreous. 2016:2():12. doi: 10.1186/s40942-016-0035-x. Epub 2016 Apr 8 [PubMed PMID: 27847630]
Makino S, Tampo H, Arai Y, Obata H. Correlations between choroidal abnormalities, Lisch nodules, and age in patients with neurofibromatosis type 1. Clinical ophthalmology (Auckland, N.Z.). 2014:8():165-8. doi: 10.2147/OPTH.S56327. Epub 2013 Dec 3 [PubMed PMID: 24403820]
Saurabh K, Roy R, Mishra S, Garg B, Goel S. Multicolor imaging features of dissociated optic nerve fiber layer after internal limiting membrane peeling. Indian journal of ophthalmology. 2018 Dec:66(12):1853-1854. doi: 10.4103/ijo.IJO_783_18. Epub [PubMed PMID: 30451197]
Tan AC, Fleckenstein M, Schmitz-Valckenberg S, Holz FG. Clinical Application of Multicolor Imaging Technology. Ophthalmologica. Journal international d'ophtalmologie. International journal of ophthalmology. Zeitschrift fur Augenheilkunde. 2016:236(1):8-18. doi: 10.1159/000446857. Epub 2016 Jul 13 [PubMed PMID: 27404384]
Gupta K, Agarwal A, Arora A, Aggarwal K, Bansal R, Katoch D, Marchese A, Singh SR, Agrawal R, Gupta V. MULTICOLOR CONFOCAL SCANNING LASER OPHTHALMOSCOPE IMAGING IN POSTERIOR UVEITIS. Retina (Philadelphia, Pa.). 2022 Jul 1:42(7):1356-1363. doi: 10.1097/IAE.0000000000003444. Epub [PubMed PMID: 35723923]
Wintergerst MWM, Jansen LG, Holz FG, Finger RP. Smartphone-Based Fundus Imaging-Where Are We Now? Asia-Pacific journal of ophthalmology (Philadelphia, Pa.). 2020 Jul-Aug:9(4):308-314. doi: 10.1097/APO.0000000000000303. Epub [PubMed PMID: 32694345]
Chalam KV, Chamchikh J, Gasparian S. Optics and Utility of Low-Cost Smartphone-Based Portable Digital Fundus Camera System for Screening of Retinal Diseases. Diagnostics (Basel, Switzerland). 2022 Jun 20:12(6):. doi: 10.3390/diagnostics12061499. Epub 2022 Jun 20 [PubMed PMID: 35741312]
Gobbi JD, Braga JPR, Lucena MM, Bellanda VCF, Frasson MVS, Ferraz D, Koh V, Jorge R. Efficacy of smartphone-based retinal photography by undergraduate students in screening and early diagnosing diabetic retinopathy. International journal of retina and vitreous. 2022 Jun 7:8(1):35. doi: 10.1186/s40942-022-00388-y. Epub 2022 Jun 7 [PubMed PMID: 35672839]
Tan CH, Kyaw BM, Smith H, Tan CS, Tudor Car L. Use of Smartphones to Detect Diabetic Retinopathy: Scoping Review and Meta-Analysis of Diagnostic Test Accuracy Studies. Journal of medical Internet research. 2020 May 15:22(5):e16658. doi: 10.2196/16658. Epub 2020 May 15 [PubMed PMID: 32347810]
Level 2 (mid-level) evidenceRamasamy K, Mishra C, Kannan NB, Namperumalsamy P, Sen S. Telemedicine in diabetic retinopathy screening in India. Indian journal of ophthalmology. 2021 Nov:69(11):2977-2986. doi: 10.4103/ijo.IJO_1442_21. Epub [PubMed PMID: 34708732]
Abràmoff MD, Lavin PT, Birch M, Shah N, Folk JC. Pivotal trial of an autonomous AI-based diagnostic system for detection of diabetic retinopathy in primary care offices. NPJ digital medicine. 2018:1():39. doi: 10.1038/s41746-018-0040-6. Epub 2018 Aug 28 [PubMed PMID: 31304320]
Vloka C, Wingrove P, Ong J, Koretz Z, Yadav S, Dmitriev A, Bowers L, Miller T, Samanthapudi K, Beale O, Waxman E. A Novel Approach to Teaching Fundoscopy Using a Virtual Format. MedEdPORTAL : the journal of teaching and learning resources. 2022:18():11252. doi: 10.15766/mep_2374-8265.11252. Epub 2022 May 27 [PubMed PMID: 35692603]
Silva PS, Cavallerano JD, Haddad NM, Kwak H, Dyer KH, Omar AF, Shikari H, Aiello LM, Sun JK, Aiello LP. Peripheral Lesions Identified on Ultrawide Field Imaging Predict Increased Risk of Diabetic Retinopathy Progression over 4 Years. Ophthalmology. 2015 May:122(5):949-56. doi: 10.1016/j.ophtha.2015.01.008. Epub 2015 Feb 19 [PubMed PMID: 25704318]
Level 2 (mid-level) evidenceKumar N, Sharma A, Tripathy K. Commentary: Big data in Ophthalmology: A big game changer on horizon. Indian journal of ophthalmology. 2021 Nov:69(11):3188-3189. doi: 10.4103/ijo.IJO_2566_21. Epub [PubMed PMID: 34708769]
Level 3 (low-level) evidenceKim J, Ryu IH, Kim JK, Lee IS, Kim HK, Han E, Yoo TK. Machine learning predicting myopic regression after corneal refractive surgery using preoperative data and fundus photography. Graefe's archive for clinical and experimental ophthalmology = Albrecht von Graefes Archiv fur klinische und experimentelle Ophthalmologie. 2022 Nov:260(11):3701-3710. doi: 10.1007/s00417-022-05738-y. Epub 2022 Jun 24 [PubMed PMID: 35748936]
Cho BJ, Lee M, Han J, Kwon S, Oh MS, Yu KH, Lee BC, Kim JH, Kim C. Prediction of White Matter Hyperintensity in Brain MRI Using Fundus Photographs via Deep Learning. Journal of clinical medicine. 2022 Jun 9:11(12):. doi: 10.3390/jcm11123309. Epub 2022 Jun 9 [PubMed PMID: 35743380]
Gunasekaran K, Pitchai R, Chaitanya GK, Selvaraj D, Annie Sheryl S, Almoallim HS, Alharbi SA, Raghavan SS, Tesemma BG. A Deep Learning Framework for Earlier Prediction of Diabetic Retinopathy from Fundus Photographs. BioMed research international. 2022:2022():3163496. doi: 10.1155/2022/3163496. Epub 2022 Jun 7 [PubMed PMID: 35711528]
Betzler BK, Rim TH, Sabanayagam C, Cheng CY. Artificial Intelligence in Predicting Systemic Parameters and Diseases From Ophthalmic Imaging. Frontiers in digital health. 2022:4():889445. doi: 10.3389/fdgth.2022.889445. Epub 2022 May 26 [PubMed PMID: 35706971]
Grauslund J. Diabetic retinopathy screening in the emerging era of artificial intelligence. Diabetologia. 2022 Sep:65(9):1415-1423. doi: 10.1007/s00125-022-05727-0. Epub 2022 May 31 [PubMed PMID: 35639120]
Watanabe T, Hiratsuka Y, Kita Y, Tamura H, Kawasaki R, Yokoyama T, Kawashima M, Nakano T, Yamada M. Combining Optical Coherence Tomography and Fundus Photography to Improve Glaucoma Screening. Diagnostics (Basel, Switzerland). 2022 Apr 27:12(5):. doi: 10.3390/diagnostics12051100. Epub 2022 Apr 27 [PubMed PMID: 35626256]
Hao Y, Liu S, Yu Z. Value of Combining Optical Coherence Tomography with Fundus Photography in Screening Retinopathy in Patients with High Myopia. Journal of healthcare engineering. 2022:2022():6556867. doi: 10.1155/2022/6556867. Epub 2022 Apr 11 [PubMed PMID: 35449843]
Midena E, Zennaro L, Lapo C, Torresin T, Midena G, Pilotto E, Frizziero L. Handheld Fundus Camera for Diabetic Retinopathy Screening: A Comparison Study with Table-Top Fundus Camera in Real-Life Setting. Journal of clinical medicine. 2022 Apr 22:11(9):. doi: 10.3390/jcm11092352. Epub 2022 Apr 22 [PubMed PMID: 35566478]
Level 3 (low-level) evidenceLin JY, Kang EY, Banker AS, Chen KJ, Hwang YS, Lai CC, Huang JL, Wu WC. Comparison of RetCam and Smartphone-Based Photography for Retinopathy of Prematurity Screening. Diagnostics (Basel, Switzerland). 2022 Apr 10:12(4):. doi: 10.3390/diagnostics12040945. Epub 2022 Apr 10 [PubMed PMID: 35453993]