Introduction
Noise exposure is evolving into a significant occupational hazard and environmental pollutant as the planet becomes increasingly industrialized. Noise and hearing impairment have become growing concerns over the last century. Noise pollution is intensifying worldwide due to myriad factors, including burgeoning populations, expanding industrialization, the popularization of motor vehicles, and widespread recreational activity. Noise causes auditory and systemic health problems due to the immediate adverse effect of high-amplitude acoustic trauma and cumulative adverse effects from chronic noise exposure.
A lack of awareness exists among the public of the ill effects of noise on physical and mental health. Government regulatory agencies, such as the United States Occupational Safety and Health Administration (OSHA), are tasked with preventing noise exposure and creating awareness of the impact of noise exposure among employers, employees, and the general public. Additionally, research studies are being performed in different noise environments, such as factories, military bases, and airports, to determine the exact magnitude of the problem that noise exposure presents to the public.[1]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The source of noise exposure can be occupational or environmental. Occupational noise exposure occurs in areas like mines, factories, rail yards, construction sites, or military bases. Environmental noise exposure occurs on highways, trains, airplanes, and in recreational places like nightclubs, sporting venues, or shooting ranges. Additionally, using earphones or headphones while listening to loud music has increased the risk of early sensorineural hearing loss in young adults.[2]
Noise-induced hearing loss (NIHL) may be acute or chronic. Acute noise exposure, or acoustic trauma, may, depending on the intensity of the exposure, result in reversible or irreversible hearing loss from explosions, loud music, and other short-duration, high-amplitude sounds. Chronic noise exposure, on the other hand, can cause various auditory and nonauditory health problems. Other factors that may affect the severity of acquired sensorineural hearing loss include socioeconomic status, ethnicity, age, tobacco use, exposure to ototoxic drugs, and associated comorbidities such as diabetes and hypertension.[3][4]
Epidemiology
The exact incidence of NIHL is difficult to determine due to the limited data available. The World Health Organization estimates that more than 1 billion people worldwide between the ages of 12 and 35 years are at risk of hearing loss due to recreational exposure to loud sounds. NIHL is more prevalent in males, predominantly due to greater occupational exposure, particularly in lower socioeconomic status populations.[5] Females, however, may be somewhat protected from NIHL by hormonal effects. NIHL is considered the second-most-common cause of occupational illness, affecting roughly one-fifth of American adults with hearing loss.[6][7]
Pathophysiology
The auditory apparatus comprises the outer, middle, and inner ears. The external or outer ear consists of the pinna and the external auditory canal. The pinna localizes sounds and conducts them to the external auditory meatus, the entrance to the external auditory canal. The external auditory canal acts as a resonator that amplifies sounds by 5 to 10 dB in the 2 to 5 kHz frequency range.
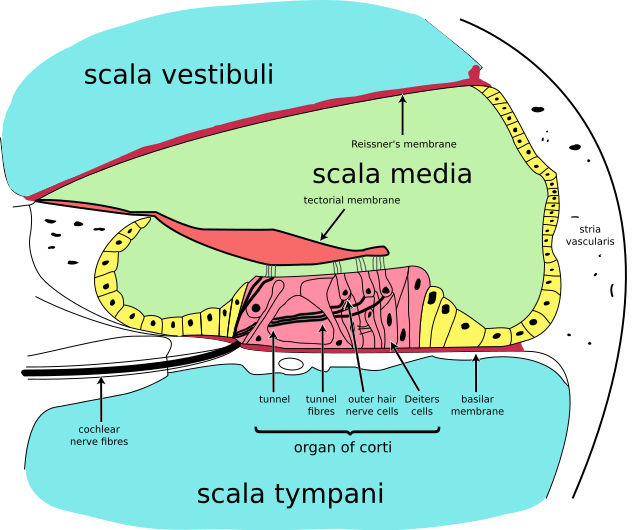
The middle ear is separated from the outer ear by the tympanic membrane. It contains the ossicular chain, which amplifies the incoming sound energy by impedance matching, ultimately vibrating the footplate of stapes. This movement is transmitted to the perilymph, causing wave-like motion of the basilar membrane, starting from the base of the cochlea and progressing toward the apex (see Image. Cochlea, Cross-Section). According to the "traveling theory of Von Békésy," the wave propagates along the basilar membrane, and different regions of the cochlea are stimulated depending on the fundamental frequency of the vibration. This forms the basis of the tonotopic or place theory of the cochlea, in which high-frequency sounds produce the greatest displacement of the basilar membrane near the basal end of the cochlea, and low-frequency sounds produce the greatest displacement at the apical end.[8]
The inner ear's tensor tympani and stapedius muscles attenuate sounds via reflex contraction, thereby protecting the cochlea from injury. The stapedius muscle plays a crucial role by attenuating low-frequency sounds greater than 80 to 90 dB through reflexive contraction, with a 100 to 200 ms latency. This delay prevents the stapedius muscle from protecting the cochlea from high-intensity impulse noises like gunshots, which can cause acoustic trauma. For this reason, providing a noise primer before a loud noise will preemptively trigger otoprotective stapedial contraction that may reduce noise-induced cochlear synaptopathy, which is characterized by inner hair cell synaptic losses and leads to tinnitus, hyperacusis, and difficulty hearing in noisy environments.[9][10]
Because of its acute and cumulative effects on the cochlea, noise may be considered a type of toxin, manifesting its effects in proportion to the total dose. The two primary presentations of NIHL are temporary and permanent threshold shifts.
Temporary threshold shift (TTS) occurs after short-term exposure or acoustic trauma and recovers in a few days. TTS happens primarily due to the reversible uncoupling of outer hair cell stereocilia from the tectorial membrane, although specific synaptopathic mechanisms are also believed to be involved. Permanent threshold shift (PTS) occurs after chronic noise exposure or acoustic trauma and is irreversible. PTS occurs due to the loss of outer hair cells, especially at the basal turn, followed by neuronal degeneration of the auditory nerve. The inability of mammalian sensory hair cells to regenerate causes permanent damage. Repeated TTS can also cause PTS.[11]
NIHL results from the interaction of genetic and environmental factors and is based on the equal-energy principle, which states that equal energy causes equal damage. In essence, higher levels of noise exposure over a short period or equivalent lower levels of noise exposure over a prolonged period will cause similar degrees of cochlear damage. NIHL may occur due to several pathological processes. Metabolic derangements may contribute to NIHL, such as excessive glutamate release damaging inner hair cell synapses or the accumulation of reactive oxygen species damaging DNA and causing cellular death.[12][13][14] Vascular insufficiency may cause cochlear hypoxia and outer hair cell damage depleting the sensory epithelium of the cochlea, especially of the outer hair cells and their associated neurons.[15][16]
History and Physical
A single loud noise exposure may cause acoustic trauma. Characteristics of acoustic trauma include hearing loss, tinnitus, hyperacusis, dizziness, aural fullness, and headache. Concurrent acoustic shock may occur, characterized by otalgia, nausea, anxiety, fatigue, and depression. Contrarily, clinical symptoms from chronic noise exposure are typically limited to hearing loss and tinnitus. Tinnitus, or "ringing in the ears," is the subjective sensation of sound; it is frequently bothersome and is an early indicator of auditory injury. NIHL-associated tinnitus occurs with threshold elevation in the 3 to 6 kHz region of the pure-tone audiogram.[17][18]
Noise exposure may also cause nonauditory symptoms like headache, anxiety, depression, insomnia, poor concentration with daytime sleepiness, increased risk of hypertension and cardiovascular disease in adults, and cognitive decline in children. NIHL causes a maximum reduction in hearing sensitivity in the 3 to 6 kHz range, with recovery towards the normal baseline at 8 kHz and above.[19]
The 3 factors that must be considered when arriving at a diagnosis of NIHL are the type and degree of noise exposure, the potential for age-related hearing impairment, and possible idiopathic degenerative changes in predisposed individuals.
NIHL is sensorineural in nature and almost always bilateral with symmetrical or near symmetrical loss except when caused by unilateral noise exposure, such as with firearm use, in which one ear is pointed toward the weapon's muzzle and the other ear is pointed away. Patients with typical NIHL have normal or near-normal speech discrimination scores.[20]
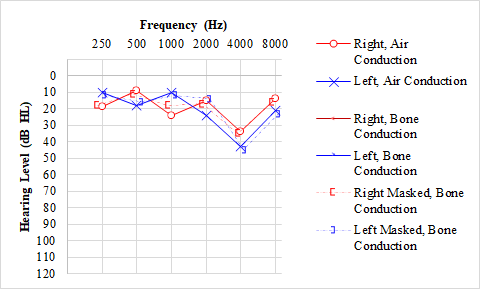
The rate of NIHL due to chronic noise exposure is greatest during the first 10 to 15 years of noise exposure, after which the loss rate decreases gradually without significant progression. Noise exposure alone does not usually cause hearing loss of more than 75 dB in higher frequencies and 40 dB in lower frequencies. Patients with NIHL demonstrate pure-tone audiogram "notching" at 3000, 4000, or 6000 Hz, with recovery at 8000 Hz.[18]
Evaluation
The diagnosis of NIHL should only be made after a comprehensive evaluation and consideration of other possibly contributing to hearing loss; some individuals with occupation-associated NIHL may claim compensation. A battery of audiological tests is required to diagnose NIHL.
Pure-tone Audiometry
Conventional audiometry usually reveals bilateral high-frequency hearing loss with a notch between 3 and 6 kHz and recovery at 8 kHz (see Image. Audiogram, Noise-Induced Hearing Loss). In cases of asymmetrical hearing loss, magnetic resonance imaging of the brain with contrast should be performed to rule out vestibular schwannoma. Asymmetrical hearing loss is characterized by a difference of 15 dB or more in any two frequencies in the range of 2 to 8 kHz, 20 dB or more in any two contiguous frequencies, or more than a 10 dB difference in the 2 kHz frequency.[21]
Hearing in Noise Test
Sentences are repeated in quiet surroundings and with background noise. Persons with presbycusis and central auditory processing disorder have difficulty hearing in noise. This test also helps determine the signal-to-noise ratio for programming hearing aids.
Speech Audiometry
Basic speech audiometry is an assessment of the reception, discrimination, and recognition of speech. The speech recognition threshold (SRT) is the minimum hearing level at which an individual can correctly repeat 50% of the speech material. The word recognition score (WR) or speech discrimination score represents the number of words correctly repeated, expressed as a percentage. The SRT scores in quiet and noisy surroundings may be decreased in the early stages of NIHL despite normal audiometry thresholds. This occurs secondary to synaptopathic mechanisms and decreased temporal processing. If SRT scores diverge more than 10 dB from pure-tone audiometry thresholds for speech frequencies, nonorganic hearing loss should be excluded.[22]
Otoacoustic Emissions
Otoacoustic emissions (OAEs) are sounds produced by the movement of outer hair cells within a properly functioning cochlea when stimulated by external sounds. This is an objective, sensitive, and easy-to-use test. Distortion product OAEs can detect early NIHL with 82% sensitivity and 92.5% specificity even when pure-tone audiometry is normal.[23]
Brainstem-evoked Response Audiometry
Brainstem-evoked response audiometry (BERA) is an electrophysiological measurement used to detect noise-induced synaptopathy by revealing a reduction of wave I of the auditory brainstem response. This test is also helpful for identifying individuals with feigned hearing loss, especially those seeking compensation.
Evidence suggests that auditory reflex testing may help detect early noise-induced synaptopathy, but further research is required. The efficacy of high-frequency audiometry (8 to 20 kHz) to detect early NIHL is also under investigation.[24]
Calculating Hearing Loss
Calculating the percentage of hearing loss is performed in three steps and is the basis for determining the magnitude of a compensation claim.[25]
- The arithmetic mean of the hearing thresholds for each ear at 500 Hz, 1 kHz, 2 kHz, and 3 kHz determine the pure-tone audiometry threshold average.
- The monaural hearing impairment for each ear is calculated by subtracting 25 dB from the pure-tone audiometry threshold average calculated in Step 1 and multiplying the result by 1.5. This calculation assumes that hearing loss becomes a handicap beyond 25 dB and increases at a rate of 1.5% per dB after 25 dB.
- The hearing handicap is calculated by multiplying the better ear impairment percentage by 5, adding this to the worse ear impairment percentage, and dividing the total by 6.
Table. Hearing handicap calculation worksheet
|
Testing frequency |
Right ear testing results, dB |
Left ear testing results, dB |
|
500 Hz |
__ dB |
__ dB |
|
1000 Hz |
__ dB |
__ dB |
|
2000 Hz |
__ dB |
__ dB |
|
3000 Hz |
__ dB |
__ dB |
|
Calculations |
||
|
Pure-tone average (PTA) |
(∑ right ear thresholds) ÷ 4 |
(∑ left ear thresholds) ÷ 4 |
|
Monaural impairment (MI) |
(Right PTA - 25) x 1.5 |
(Left PTA - 25) x 1.5 |
|
Hearing handicap |
[(5 x MI better ear) + (MI worse ear)] ÷ 6 |
Treatment / Management
The gold-standard treatment of NIHL is amplification through the use of hearing aids. A hearing aid is recommended if the SRT is more than 25 dB or the word recognition score is less than 80% at presentation levels of 50 dB above the threshold. Noise-induced tinnitus is treated with a tinnitus masker or tinnitus retraining therapy.
Some pharmaceutical agents show promising protective effects against NIHL, including corticosteroids, antioxidants, and neurotrophins. Corticosteroids are helpful in acute acoustic trauma due to their anti-inflammatory effect when administered intravenously, orally, or intratympanically.[26][27] Intravenous corticosteroid regimens may include methylprednisolone 125 mg on the first day of treatment, 80 mg on the second day, and 40 mg on the last day.[28] Alternatively, oral prednisone may be administered at 1 mg/kg up to 60 mg daily for 1 to 2 weeks, with longer courses producing better outcomes in patients who can tolerate high-dose steroids for more than 1 week.[26][29] However, the role of corticosteroids in treating chronic occupational NIHL is unclear.
Hyperbaric oxygen therapy has also proven useful in acoustic trauma, particularly if corticosteroid therapy fails; treatment may consist of 120-minute dives to 200 to 280 kPa daily for 10 days.[28][30][31] Based on the oxidative stress hypotheses, antioxidants like N-acetyl cysteine, D-methionine, and coenzyme Q10 are undergoing clinical trials for use as otoprotective agents.[32][33] Magnesium and vitamins A, E, C, and B12 have also demonstrated protective effects against NIHL in animal models.[34] (A1)
The cornerstone of NIHL management is prevention. Prevention of NIHL involves periodic noise monitoring by exposure assessment, reducing noise exposure in workplaces, and early detection of noise-induced auditory injury. Noise monitoring can be conducted through area noise surveys and personal noise dosimetry. During area noise surveys, a sound pressure level meter is kept in a specific location to sample the noise field. For personal noise dosimetry, the sound pressure level meter is worn on the body with a microphone on the shoulder, 5 in lateral to the ear.
Reducing occupational noise exposure can be achieved via engineering controls, administrative controls, and personal hearing protection. Engineering control measures include enclosures to isolate noise sources from personnel and other barriers to reduce acoustic energy transmission. Regulatory standards determine administrative controls in a given location or jurisdiction. Many countries follow the permissible exposure limit of 85 dBA in workplaces. The dBA is sound pressure measured with A-weighting, an adjusted measurement of noise that considers the sensitivity of the human ear to different sound frequencies. Workers should be educated regarding the necessity of personal hearing protection devices like ear plugs and ear muffs, which can attenuate noise levels by up to approximately 30 dB.
Early detection of noise-induced auditory damage may be achieved by routine audiometric examinations and health education. All employees working in noisy environments should have a baseline audiogram within 6 months of starting work. If a 10 dB or more standard threshold shift in hearing average at test frequencies of 2, 3, and 4 kHz in either ear is noted, the employee should be enrolled in a hearing conservation program.[8][35](B2)
Differential Diagnosis
The differential diagnosis of NIHL includes many common causes of sensorineural hearing loss and inorganic or functional hearing loss.
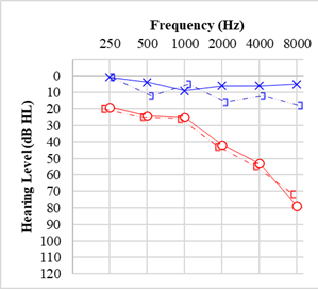
Presbycusis is age-related hearing loss, with high-frequency, down-sloping hearing loss (see Image. Audiogram, Presbycusis). Presbycusis may be sensory, where there is damage or death of cochlear sensory hair cells, or metabolic, where there is reduced functioning of the stria vascularis.[36]
Hereditary hearing impairment causing progressive degeneration traditionally manifests in childhood or early adolescence. Structural anomalies such as an enlarged vestibular aqueduct or Mondini deformity may be present.[37]
Hearing loss resulting from previous infections like labyrinthitis, meningitis, or encephalitis with cochlear ossification may mimic NIHL.
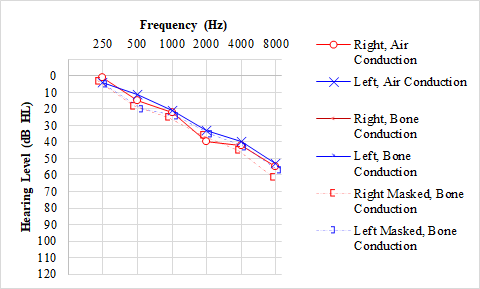
Hearing loss from central nervous system dysfunction, such as following a posterior circulation cerebrovascular accident, is typically characterized by the sudden onset of hearing loss and is frequently associated with other neurological deficits.[38] Cerebellopontine angle tumors may cause hearing loss; hearing loss is usually slowly progressive and unilateral, sometimes with associated tinnitus, vertigo, and headache (see Image. Audiogram, Vestibular Schwannoma).[39]
Auditory neuropathy and synaptopathy result in defective neural processing of auditory stimuli. The defect may be with inner hair cell activity, auditory nerve signal transmission, or dysfunction at the synapses of the inner hair cells with the auditory nerve. Patients with this disorder have difficulty hearing in noisy environments and suffer from directional hearing loss, usually bilateral. Audiological evaluation reveals abnormal BERA with the presence of OAEs.[40]
The general presentation of the person with feigned hearing loss is of exaggerated hearing difficulty but with normal vocal volume. There may be a lack of the required eye contact or observed lip movements that patients with organic hearing loss need to understand speech. An SRT better than the PTA by more than 10 to 15 dB suggests functional hearing loss, which may be confirmed with a Stenger test.[41][22]
Prognosis
The natural history of NIHL indicates that the greatest progression of hearing loss occurs in the first 10 to 15 years, following which hearing levels tend to stabilize somewhat. NIHL generally does not progress after the cessation of noise exposure.
As NIHL is a permanent and irreversible condition, prevention is critical. Noise exposure should be regulated carefully by following the maximum allowable daily noise exposure or permissible exposure limit (PEL). For an 8-hour workday, OSHA regulations require employers to use engineering controls when exposures exceed 90 dBA, and administrative controls, such as hearing protection and annual hearing monitoring, when exposures exceed 85 dBA. For exposures longer or shorter than 8 hours, the PEL is increased or decreased by 5 dB for each halving or doubling of sound exposure, respectively.
The United States National Institute for Occupational Safety and Health recommends that the highest permissible level of noise exposure in the workplace be an average of 85 dB over an 8-hour workday; for exposures other than 8 hours, the PEL is increased or decreased by 3 dB for each halving or doubling of sound exposure, respectively. For example, the PEL for a 4-hour workday would be 88 dB, and for a 16-hour workday, it would be 82 dB.[42][43]
The World Health Organization also recommends daily noise exposure limits, suggesting that levels should not exceed 70 dB over 24 hours or 85 dB over 1 hour to avoid hearing impairment.[44]
Complications
The effects of loud noise exposure are pathological, psychological, and sociological. Apart from the well-known auditory effects of hearing loss, tinnitus, and vertigo, noise also has systemic effects on metabolism, including increasing cortisol and norepinephrine levels, among other hormones.[45][46][47] These derangements significantly increase the risk of hypertension, ischemic heart disease, myocardial infarction, and stroke.[48]
Chronic noise exposure also impairs sleep, increasing the risk of workplace accidents. Additionally, there is an increase in the incidence of depression and generalized anxiety disorder in individuals with chronic noise exposure. Excessive noise may also affect family life, causing irritability, annoyance, confusion, and lack of concentration.[49]
NIHL can affect interpersonal communication, thereby diminishing self-esteem and interfering with relationships. It can also reduce attention and cognition, increasing the risk of dementia. Noise may affect work performance, but this seems to depend on individual predisposition. The financial burden and compensation cost for employers for hearing loss can be high.
Deterrence and Patient Education
The World Health Organization reports hearing loss is among the 20 leading causes of disease burden and the most common disability globally. NIHL is the most preventable of all causes of hearing loss. The key component of prevention efforts is education at all levels. Employees and employers must understand that hearing can be protected only if efforts are undertaken to reduce all hazardous noise exposures, not just those in the workplace.
The necessity of regular screening, wearing hearing protection devices, and training should be enforced in hearing conservation programs. Public awareness of the harmful effects of noise and safe permissible limits in social gatherings, on roads, and at music concerts is essential. Regulations should be followed at all levels to prevent the hazardous effects of noise exposure.[50][51]
Enhancing Healthcare Team Outcomes
Noise and its impact on human health are best addressed by a team of medical professionals and policymakers, including primary care providers, otolaryngologists, audiologists, occupational health nurses, and government administrators. Support from concerned employers, regulatory agencies, and the mass media is needed to create public awareness and provide screening and treatment of NIHL. Further research is required to provide additional data, which may help evolve holistic and integrated healthcare for individuals affected by NIHL.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Goines L, Hagler L. Noise pollution: a modem plague. Southern medical journal. 2007 Mar:100(3):287-94 [PubMed PMID: 17396733]
Vogel I, Brug J, Hosli EJ, van der Ploeg CP, Raat H. MP3 players and hearing loss: adolescents' perceptions of loud music and hearing conservation. The Journal of pediatrics. 2008 Mar:152(3):400-4. doi: 10.1016/j.jpeds.2007.07.009. Epub 2007 Oct 22 [PubMed PMID: 18280849]
Level 2 (mid-level) evidenceAgrawal Y, Platz EA, Niparko JK. Prevalence of hearing loss and differences by demographic characteristics among US adults: data from the National Health and Nutrition Examination Survey, 1999-2004. Archives of internal medicine. 2008 Jul 28:168(14):1522-30. doi: 10.1001/archinte.168.14.1522. Epub [PubMed PMID: 18663164]
Level 2 (mid-level) evidenceKim MB. Diabetes mellitus and the incidence of hearing loss: a cohort study. International journal of epidemiology. 2017 Apr 1:46(2):727. doi: 10.1093/ije/dyw342. Epub [PubMed PMID: 28100581]
Scholes S, Biddulph J, Davis A, Mindell JS. Socioeconomic differences in hearing among middle-aged and older adults: cross-sectional analyses using the Health Survey for England. BMJ open. 2018 Feb 1:8(2):e019615. doi: 10.1136/bmjopen-2017-019615. Epub 2018 Feb 1 [PubMed PMID: 29391384]
Level 2 (mid-level) evidenceChadha S, Kamenov K, Cieza A. The world report on hearing, 2021. Bulletin of the World Health Organization. 2021 Apr 1:99(4):242-242A. doi: 10.2471/BLT.21.285643. Epub [PubMed PMID: 33953438]
Silva VARD, Mitre EI, Crespo AN. Is noise-induced hearing loss still a public health problem after decades of legislation? Brazilian journal of otorhinolaryngology. 2020 Nov-Dec:86(6):665-666. doi: 10.1016/j.bjorl.2020.04.001. Epub 2020 Apr 10 [PubMed PMID: 32417151]
Chen KH, Su SB, Chen KT. An overview of occupational noise-induced hearing loss among workers: epidemiology, pathogenesis, and preventive measures. Environmental health and preventive medicine. 2020 Oct 31:25(1):65. doi: 10.1186/s12199-020-00906-0. Epub 2020 Oct 31 [PubMed PMID: 33129267]
Level 3 (low-level) evidenceTrevino M, Zang A, Lobarinas E. The middle ear muscle reflex: Current and future role in assessing noise-induced cochlear damage. The Journal of the Acoustical Society of America. 2023 Jan:153(1):436. doi: 10.1121/10.0016853. Epub [PubMed PMID: 36732247]
Vasudevamurthy S, Kumar AU. Middle Ear Muscle Reflex in Normal-Hearing Individuals with Occupational Noise Exposure. Noise & health. 2023 Jan-Mar:25(116):1-7. doi: 10.4103/nah.nah_3_22. Epub [PubMed PMID: 37006113]
Quaranta A, Portalatini P, Henderson D. Temporary and permanent threshold shift: an overview. Scandinavian audiology. Supplementum. 1998:48():75-86 [PubMed PMID: 9505300]
Level 3 (low-level) evidenceHu N, Rutherford MA, Green SH. Protection of cochlear synapses from noise-induced excitotoxic trauma by blockade of Ca(2+)-permeable AMPA receptors. Proceedings of the National Academy of Sciences of the United States of America. 2020 Feb 18:117(7):3828-3838. doi: 10.1073/pnas.1914247117. Epub 2020 Feb 3 [PubMed PMID: 32015128]
Nyilo P, Serafika Permoni Putri M. The Association of Reactive Oxygen Species Levels on Noise Induced Hearing Loss of High Risk Workers in Dr. Soetomo General Hospital Surabaya, Indonesia. Indian journal of otolaryngology and head and neck surgery : official publication of the Association of Otolaryngologists of India. 2019 Mar:71(1):86-89. doi: 10.1007/s12070-018-1460-y. Epub 2018 Jul 28 [PubMed PMID: 30906720]
Henderson D, Bielefeld EC, Harris KC, Hu BH. The role of oxidative stress in noise-induced hearing loss. Ear and hearing. 2006 Feb:27(1):1-19 [PubMed PMID: 16446561]
Level 3 (low-level) evidenceLamm K, Arnold W. Noise-induced cochlear hypoxia is intensity dependent, correlates with hearing loss and precedes reduction of cochlear blood flow. Audiology & neuro-otology. 1996 May-Jun:1(3):148-60 [PubMed PMID: 9390798]
Level 3 (low-level) evidenceNuttall AL. Sound-Induced Cochlear Ischemia/Hypoxia as a Mechanism of Hearing Loss. Noise & health. 1999:2(5):17-32 [PubMed PMID: 12689482]
Carl AC, Hohman MH, Cornejo J. Audiology Pure Tone Evaluation. StatPearls. 2023 Jan:(): [PubMed PMID: 35593838]
Salmon MK, Brant J, Hohman MH, Leibowitz D. Audiogram Interpretation. StatPearls. 2024 Jan:(): [PubMed PMID: 35201707]
Basner M, Babisch W, Davis A, Brink M, Clark C, Janssen S, Stansfeld S. Auditory and non-auditory effects of noise on health. Lancet (London, England). 2014 Apr 12:383(9925):1325-1332. doi: 10.1016/S0140-6736(13)61613-X. Epub 2013 Oct 30 [PubMed PMID: 24183105]
Level 3 (low-level) evidenceMirza R, Kirchner DB, Dobie RA, Crawford J, ACOEM Task Force on Occupational Hearing Loss. Occupational Noise-Induced Hearing Loss. Journal of occupational and environmental medicine. 2018 Sep:60(9):e498-e501. doi: 10.1097/JOM.0000000000001423. Epub [PubMed PMID: 30095587]
Durakovic N, Valente M, Goebel JA, Wick CC. What defines asymmetric sensorineural hearing loss? The Laryngoscope. 2019 May:129(5):1023-1024. doi: 10.1002/lary.27504. Epub 2018 Nov 8 [PubMed PMID: 30408187]
Hussain SAS, Hohman MH. Nonorganic Functional Hearing Loss. StatPearls. 2023 Jan:(): [PubMed PMID: 35593862]
Job A, Raynal M, Kossowski M, Studler M, Ghernaouti C, Baffioni-Venturi A, Roux A, Darolles C, Guelorget A. Otoacoustic detection of risk of early hearing loss in ears with normal audiograms: a 3-year follow-up study. Hearing research. 2009 May:251(1-2):10-6. doi: 10.1016/j.heares.2009.02.008. Epub 2009 Feb 26 [PubMed PMID: 19249340]
Škerková M, Kovalová M, Mrázková E. High-Frequency Audiometry for Early Detection of Hearing Loss: A Narrative Review. International journal of environmental research and public health. 2021 Apr 28:18(9):. doi: 10.3390/ijerph18094702. Epub 2021 Apr 28 [PubMed PMID: 33925120]
Level 3 (low-level) evidenceNandi SS, Dhatrak SV. Occupational noise-induced hearing loss in India. Indian journal of occupational and environmental medicine. 2008 Aug:12(2):53-6. doi: 10.4103/0019-5278.43260. Epub [PubMed PMID: 20040978]
Zloczower E, Tsur N, Hershkovich S, Fink N, Marom T. Efficacy of Oral Steroids for Acute Acoustic Trauma. Audiology & neuro-otology. 2022:27(4):312-320. doi: 10.1159/000522051. Epub 2022 Mar 1 [PubMed PMID: 35231916]
Chang YS, Bang K, Choi N, Kim JS, Lee GG. Factors Associated With the Benefits of Concurrent Administration of Intratympanic Steroid Injection With Oral Steroids in Patients With Acute Acoustic Trauma. Otology & neurotology : official publication of the American Otological Society, American Neurotology Society [and] European Academy of Otology and Neurotology. 2018 Jun:39(5):565-570. doi: 10.1097/MAO.0000000000001784. Epub [PubMed PMID: 29649042]
Holy R, Zavazalova S, Prochazkova K, Kalfert D, Younus T, Dosel P, Kovar D, Janouskova K, Oniscenko B, Fik Z, Astl J. The Use of Hyperbaric Oxygen Therapy and Corticosteroid Therapy in Acute Acoustic Trauma: 15 Years' Experience at the Czech Military Health Service. International journal of environmental research and public health. 2021 Apr 22:18(9):. doi: 10.3390/ijerph18094460. Epub 2021 Apr 22 [PubMed PMID: 33922296]
Singh K, Gude A, Kour A, Guthikonda MR, Mishra AK, Gupta A. A Prospective Study to Elucidate the Efficacy of 4 Oral Prednisolone Regimens in Acute Acoustic Trauma. Indian journal of otolaryngology and head and neck surgery : official publication of the Association of Otolaryngologists of India. 2022 Dec:74(Suppl 3):3692-3699. doi: 10.1007/s12070-021-02437-8. Epub 2021 Feb 14 [PubMed PMID: 36742739]
Oya M, Tadano Y, Takihata Y, Ikomi F, Tokunaga T. Utility of Hyperbaric Oxygen Therapy for Acute Acoustic Trauma: 20 years' Experience at the Japan Maritime Self-Defense Force Undersea Medical Center. International archives of otorhinolaryngology. 2019 Oct:23(4):e408-e414. doi: 10.1055/s-0039-1688433. Epub 2019 May 28 [PubMed PMID: 31649760]
Bayoumy AB, Weenink RP, van der Veen EL, Besseling-Hansen FS, Hoedemaeker ADM, de Jong FJM, van der Laan MH, Swenker R, van Hulst RA, de Ru JA. It's all about timing, early treatment with hyperbaric oxygen therapy and corticosteroids is essential in acute acoustic trauma. Journal of otology. 2021 Oct:16(4):237-241. doi: 10.1016/j.joto.2021.05.001. Epub 2021 May 11 [PubMed PMID: 34548870]
Chang PH, Liu CW, Hung SH, Kang YN. Effect of N-acetyl-cysteine in prevention of noise-induced hearing loss: a systematic review and meta-analysis of randomized controlled trials. Archives of medical science : AMS. 2022:18(6):1535-1541. doi: 10.5114/aoms/109126. Epub 2021 Mar 21 [PubMed PMID: 36457967]
Level 1 (high-level) evidenceFetoni AR, Ralli M, Sergi B, Parrilla C, Troiani D, Paludetti G. Protective effects of N-acetylcysteine on noise-induced hearing loss in guinea pigs. Acta otorhinolaryngologica Italica : organo ufficiale della Societa italiana di otorinolaringologia e chirurgia cervico-facciale. 2009 Apr:29(2):70-5 [PubMed PMID: 20111615]
Level 3 (low-level) evidenceLe TN, Straatman LV, Lea J, Westerberg B. Current insights in noise-induced hearing loss: a literature review of the underlying mechanism, pathophysiology, asymmetry, and management options. Journal of otolaryngology - head & neck surgery = Le Journal d'oto-rhino-laryngologie et de chirurgie cervico-faciale. 2017 May 23:46(1):41. doi: 10.1186/s40463-017-0219-x. Epub 2017 May 23 [PubMed PMID: 28535812]
Rabinowitz PM, Galusha D, Kirsche SR, Cullen MR, Slade MD, Dixon-Ernst C. Effect of daily noise exposure monitoring on annual rates of hearing loss in industrial workers. Occupational and environmental medicine. 2011 Jun:68(6):414-8. doi: 10.1136/oem.2010.055905. Epub 2010 Dec 30 [PubMed PMID: 21193566]
Level 2 (mid-level) evidenceCunningham LL, Tucci DL. Hearing Loss in Adults. The New England journal of medicine. 2017 Dec 21:377(25):2465-2473. doi: 10.1056/NEJMra1616601. Epub [PubMed PMID: 29262274]
Lasak JM, Allen P, McVay T, Lewis D. Hearing loss: diagnosis and management. Primary care. 2014 Mar:41(1):19-31. doi: 10.1016/j.pop.2013.10.003. Epub 2013 Nov 18 [PubMed PMID: 24439878]
Michels TC, Duffy MT, Rogers DJ. Hearing Loss in Adults: Differential Diagnosis and Treatment. American family physician. 2019 Jul 15:100(2):98-108 [PubMed PMID: 31305044]
Sheikh MM, De Jesus O. Vestibular Schwannoma. StatPearls. 2023 Jan:(): [PubMed PMID: 32965983]
Hood LJ. Auditory Neuropathy/Auditory Synaptopathy. Otolaryngologic clinics of North America. 2021 Dec:54(6):1093-1100. doi: 10.1016/j.otc.2021.07.004. Epub 2021 Sep 15 [PubMed PMID: 34535280]
Mehta AK, Singh VK. SCREENING TESTS FOR NONORGANIC HEARING LOSS. Medical journal, Armed Forces India. 2000 Jan:56(1):79-81. doi: 10.1016/S0377-1237(17)30105-3. Epub 2017 Jun 8 [PubMed PMID: 28790658]
Davis R. Long-term noise exposures: A brief review. Hearing research. 2017 Jun:349():31-33. doi: 10.1016/j.heares.2016.10.006. Epub 2016 Oct 22 [PubMed PMID: 27780746]
Sriwattanatamma P, Breysse P. Comparison of NIOSH noise criteria and OSHA hearing conservation criteria. American journal of industrial medicine. 2000 Apr:37(4):334-8 [PubMed PMID: 10706744]
Śliwińska-Kowalska M, Zaborowski K. WHO Environmental Noise Guidelines for the European Region: A Systematic Review on Environmental Noise and Permanent Hearing Loss and Tinnitus. International journal of environmental research and public health. 2017 Sep 27:14(10):. doi: 10.3390/ijerph14101139. Epub 2017 Sep 27 [PubMed PMID: 28953238]
Level 1 (high-level) evidenceSpreng M. Possible health effects of noise induced cortisol increase. Noise & health. 2000:2(7):59-64 [PubMed PMID: 12689472]
Turner JG, Parrish JL, Hughes LF, Toth LA, Caspary DM. Hearing in laboratory animals: strain differences and nonauditory effects of noise. Comparative medicine. 2005 Feb:55(1):12-23 [PubMed PMID: 15766204]
Level 3 (low-level) evidenceSaid MA, El-Gohary OA. Effect of noise stress on cardiovascular system in adult male albino rat: implication of stress hormones, endothelial dysfunction and oxidative stress. General physiology and biophysics. 2016 Jul:35(3):371-7. doi: 10.4149/gpb_2016003. Epub 2016 May 13 [PubMed PMID: 27174896]
Skogstad M, Johannessen HA, Tynes T, Mehlum IS, Nordby KC, Lie A. Systematic review of the cardiovascular effects of occupational noise. Occupational medicine (Oxford, England). 2016 Jan:66(1):10-6. doi: 10.1093/occmed/kqv148. Epub [PubMed PMID: 26732793]
Level 1 (high-level) evidenceHahad O, Prochaska JH, Daiber A, Muenzel T. Environmental Noise-Induced Effects on Stress Hormones, Oxidative Stress, and Vascular Dysfunction: Key Factors in the Relationship between Cerebrocardiovascular and Psychological Disorders. Oxidative medicine and cellular longevity. 2019:2019():4623109. doi: 10.1155/2019/4623109. Epub 2019 Nov 11 [PubMed PMID: 31814877]
Gilani TA, Mir MS. A study on the assessment of traffic noise induced annoyance and awareness levels about the potential health effects among residents living around a noise-sensitive area. Environmental science and pollution research international. 2021 Nov:28(44):63045-63064. doi: 10.1007/s11356-021-15208-3. Epub 2021 Jul 3 [PubMed PMID: 34218377]
Di Berardino F, Forti S, Iacona E, Orlandi GP, Ambrosetti U, Cesarani A. Public awareness of ear and hearing management as measured using a specific questionnaire. European archives of oto-rhino-laryngology : official journal of the European Federation of Oto-Rhino-Laryngological Societies (EUFOS) : affiliated with the German Society for Oto-Rhino-Laryngology - Head and Neck Surgery. 2013 Feb:270(2):449-53. doi: 10.1007/s00405-012-1961-3. Epub 2012 Feb 17 [PubMed PMID: 22350429]