Introduction
Mohs micrographic surgery stands at the forefront of dermatologic oncology, revolutionizing the treatment of cutaneous malignancies. With its meticulous microscopic margin control, Mohs surgery offers unparalleled precision in tumor removal, making it the gold standard when resecting a wide range of skin cancers.[1] Acting as both surgeon and pathologist, the Mohs surgeon navigates the complexities of tumor extirpation, guided by precise specimen mapping and rapid frozen tissue processing.[2] The Mohs map is central to the safety and accuracy of the procedure, is a critical communication tool among surgical team members, and is a key element in correlating tissue samples with the surgical site.
Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Function
The Mohs map is a crucial tool in Mohs micrographic surgery, facilitating precise correlation between the surgical site, tumor specimen, and histopathologic findings. Map accuracy is paramount, guiding the surgeon through subsequent procedural stages to ensure complete removal of the cutaneous neoplasm. As the primary means of communication among all members of the Mohs surgical team, including the Mohs surgeon, medical assistants, and Mohs histotechnician, the Mohs map plays a central role in achieving optimal outcomes and fostering collaborative care.
In the initial stage of Mohs micrographic surgery, tissue is meticulously extirpated and carefully placed on blotting paper while ensuring continuous orientation. Subsequently, the specimen is diligently measured and drawn onto the Mohs map with specific orientation markers.[3] The oriented tumor specimen is then inked with common colors such as blue, yellow, black, or green, typically at the 3-, 6-, 9-, and 12-o'clock positions.[2][4] Red ink is avoided to prevent confusion with the marking pen used to denote positive tumor margins after histopathological evaluation by the surgeon.[2][5] Consistency and accuracy in tissue processing are imperative regardless of the inking technique employed.[6] After inking, the histotechnician rapidly processes the tissue specimen using the frozen section technique.[7][8]
After processing, the Mohs surgeon systematically evaluates the tissue, employing the same techniques as a dermatopathologist.[9] The specimen undergoing evaluation should contain the entire epidermal margin, dermis, and deeper structures. Tumor positivity is annotated on the Mohs map by the surgeon with a red marking pen highlighting areas of concern. The Mohs map may also include comments on benign tumors, perineural invasion, dense inflammation, and deposition artifacts.[2] Once tissue evaluation is completed, the map is passed to the medical assistant to prepare the patient for subsequent stages of surgical reconstruction.
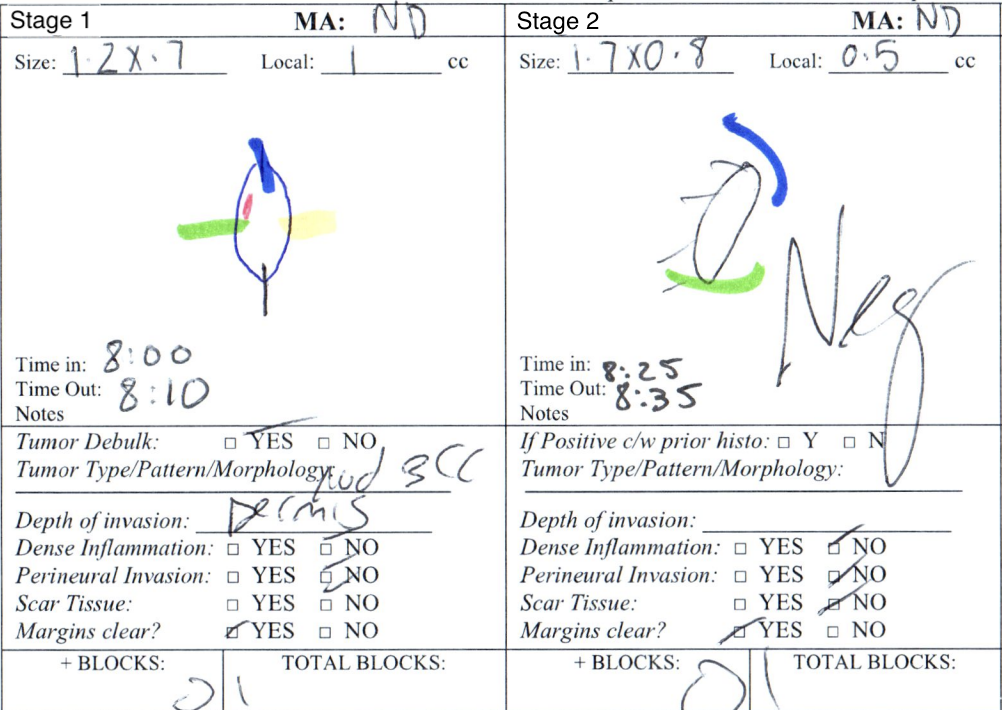
Any remaining areas of tumor positivity are removed during subsequent stages of Mohs surgery employing the same technique as described above. Tumor orientation is of particular importance during successive stages of resection.[2] If the entire circumference of the tumor was not removed during the initial resection, an explicit annotation on the Mohs map denotes the location of the epidermis on the partial layer. Typically, dashed perpendicular lines indicate the epidermal border, while the border that does not contain the dashed lines represents layers such as the dermis, subcutaneous tissue, or other deeper structures. During processing, the Mohs histotechnician understands the orientation of the specimen as well as the location of the epidermis (see Image. 2-Stage Mohs Map). Once the tumor is successfully cleared, the Mohs surgeon chooses the optimal postoperative healing approach, which may involve healing by secondary intention, surgical reconstruction utilizing layered closures, flaps, or grafts, or deferring reconstruction to a later stage.
Issues of Concern
Large Tumors
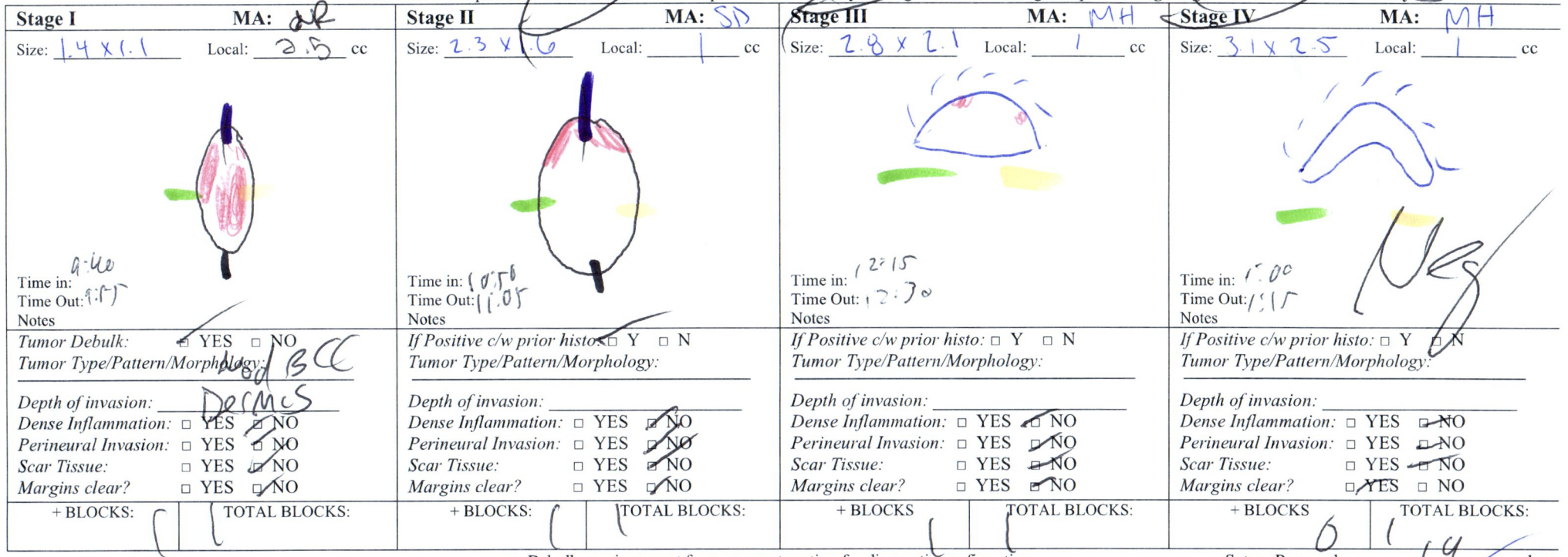
Large cutaneous tumor specimens should be divided into smaller pieces for processing onto microscope slides. Each subdivision must be labeled and documented on the Mohs map to ensure accurate tracking and correlation. However, the number of tissue subdivisions should be minimal to reduce the risk of false positive and false negative results (see Image. Subdivided Mohs Layer).[2]
Depth of Invasion
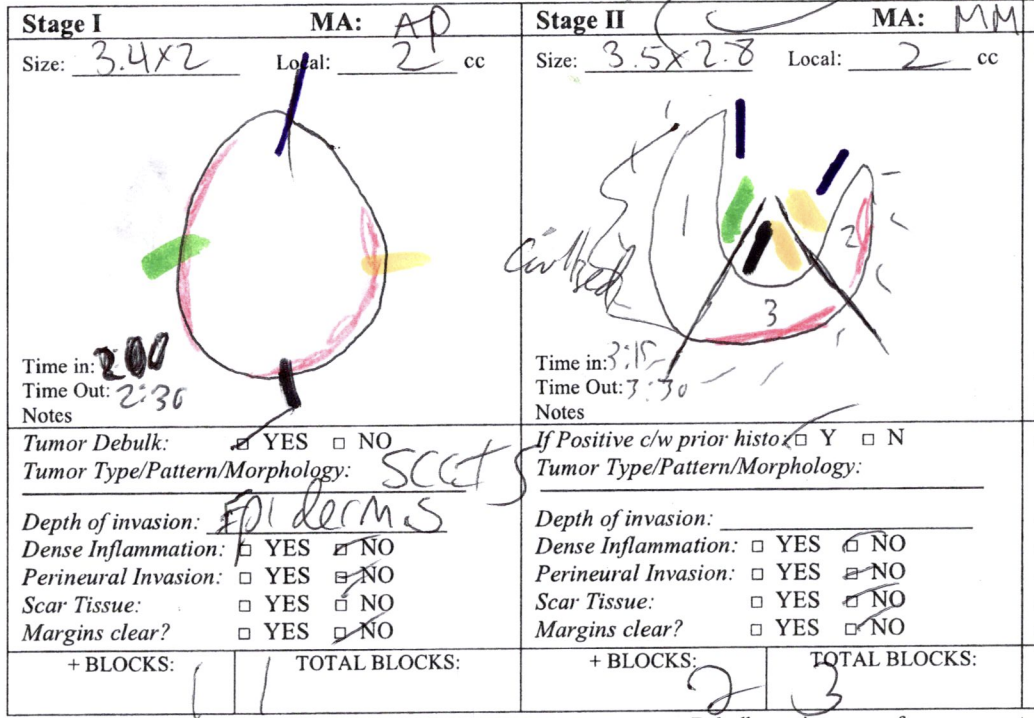
Traditionally, a red marking pen is used to denote areas of malignancy on each layer. Epidermal involvement of the malignancy is marked at the periphery of the Mohs layer. Dermal positivity of the malignancy is marked within the drawing at the precise area of involvement (see Image. 4-Stage Mohs Map).
Documentation of Nonmalignant Lesions
During the examination of each stage in Mohs micrographic surgery, the Mohs surgeon may encounter various cutaneous tumors, premalignant skin lesions, or benign skin growths.[10] When a lesion other than the primary tumor is identified, annotating its type, location, and management plan on the Mohs map is essential. Common skin growths requiring documentation include benign follicular hamartoma, syringoma, trichoepithelioma, and wart dyskeratoma. Additionally, the location of precancerous actinic keratosis should be noted, along with the planned intervention, such as curettage or field therapy with 5-fluorouracil cream.
Marking Techniques for Tissue Orientation
Maintaining proper orientation is paramount in Mohs micrographic surgery to ensure the accurate transfer of tumor positivity from the map to the patient. Improper orientation risks a false negative result and compromises tumor clearance. The most common orientation technique involves tissue nicking on the patient, although other methods like sutures, staples, gentian violet, or methylene blue may be used.[11] The chosen marking method is transferred from the patient to the Mohs map. Consistent and accurate orientation techniques are integral to achieving superior cure rates in Mohs micrographic surgery.[12]
Potential Sources of Error in Mohs Mapping
A precise Mohs map is essential to the safety and efficacy of Mohs micrographic surgery. Various sources of error in Mohs mapping can compromise accuracy, including incorrect orientation, sectioning, inking by the histotechnician, miscommunication between the surgeon and histotechnician, and specimen mislabeling in the cryostat. These errors can result in false negative and false positive results. Moreover, with increased cases and subsequent stages, the likelihood of mapping errors rises, underscoring the importance of stringent quality control measures in Mohs micrographic surgery.[13][14][15]
Other Issues
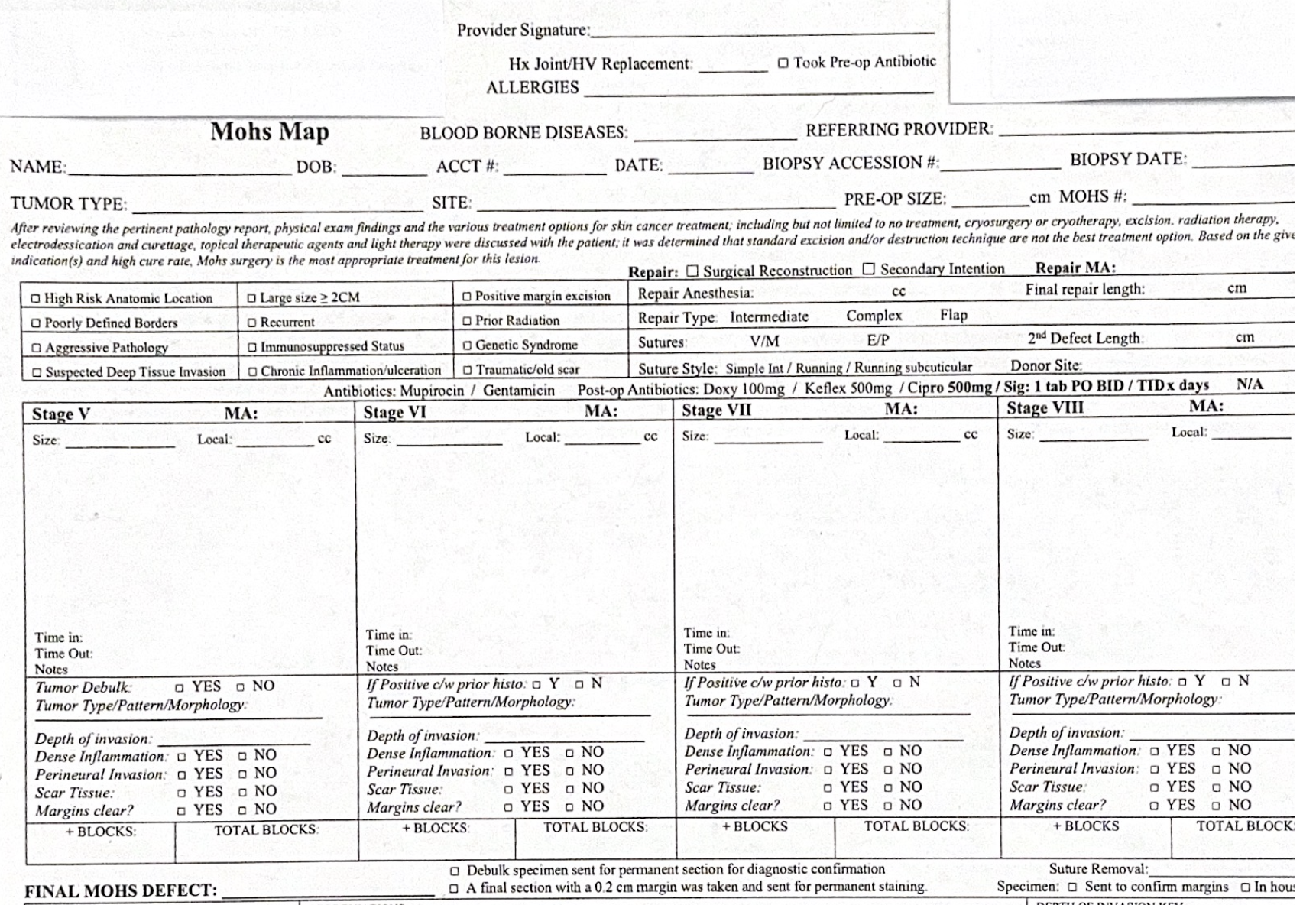
Sample Mohs Map
An effective Mohs map comprises preoperative, surgical, and postoperative reconstruction sections (see Image. Blank Mohs Map). A preoperative checklist is usually included in a comprehensive map. The checklist contains patient information, the type of cancer, the site, the accession number of the original biopsy, and pertinent preoperative questions. The preoperative questions may be surgeon-specific, including but not limited to a history of joint or heart valve replacement, medication allergies, history of bloodborne illnesses, and medications that may increase bleeding risk.
The surgical area of the Mohs map contains critical components, including justification based on acceptable use criteria, division into stages, and detailed documentation of findings. Surgeons delineate the surgical stages, each accommodating a representative depiction of the layer taken, drawn to scale. Comprehensive descriptions of positive findings, encompassing tumor morphology, depth of invasion, and perineural invasion, are documented. In the postoperative reconstruction section, details such as closure type, sutures, antibiotic usage, and suture removal date are recorded, ensuring thorough postoperative care documentation.
Enhancing Healthcare Team Outcomes
In Mohs micrographic surgery, effective interprofessional collaboration is essential to ensure patient-centered care, optimize outcomes, and promote patient safety. The interdisciplinary team comprises physicians, advanced practitioners, nurses, and other health professionals, including medical assistants and histotechnicians. Central to this collaboration is an accurate and concise Mohs map, serving as a common reference point for all team members.
Physicians and advanced practitioners collaborate closely with the Mohs surgeon to assess patient suitability for surgery, provide preoperative counseling, and manage postoperative care. Nurses assist in patient preparation, monitoring, and wound care, ensuring patient comfort and safety throughout the procedure. Pharmacists manage medication, ensure appropriate drug therapy, and minimize adverse reactions.
Interprofessional communication is critical in Mohs micrographic surgery to coordinate care and mitigate potential errors. Medical assistants utilize the Mohs map for patient intake, site preparation, and documentation, while the Mohs surgeon communicates with the team regarding additional layers or tumor clearance. The histotechnician relies on the map to orient tissue accurately for processing, facilitating optimal histopathological evaluation.
By fostering open communication and collaboration among all team members, including physicians, advanced practitioners, nurses, pharmacists, and others, errors such as incorrect orientation, sectioning, inking, miscommunication, and mislabeling can be minimized. A precise Mohs map is the cornerstone for a safe and efficient Mohs surgery procedure, ensuring optimal patient outcomes and enhancing team performance.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
Subdivided Mohs Layer. This image illustrates a scenario where a large tumor has been divided into multiple sections for microscopic examination. While the first stage of the case fits onto one microscope slide, layer 2 requires division into 3 separate pieces and blocks to fit. Tissue pieces 2 and 3 from layer 2 are both positive for tumor involvement.
Contributed by K Pennycook, DO
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Cernea SS, Gontijo G, Pimentel ER, Tarlé RG, Tassara G, Ferreira JA, Fernandes VM, Bernardo WM. Indication guidelines for Mohs micrographic surgery in skin tumors. Anais brasileiros de dermatologia. 2016 Sep-Oct:91(5):621-627. doi: 10.1590/abd1806-4841.20164808. Epub [PubMed PMID: 27828636]
Wong E, Axibal E, Brown M. Mohs Micrographic Surgery. Facial plastic surgery clinics of North America. 2019 Feb:27(1):15-34. doi: 10.1016/j.fsc.2018.08.002. Epub [PubMed PMID: 30420068]
Silapunt S, Peterson SR, Alcalay J, Goldberg LH. Mohs tissue mapping and processing: a survey study. Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al.]. 2004 Jun:30(6):961 [PubMed PMID: 15171782]
Level 3 (low-level) evidenceAboul-Fettouh N, Croley JA, Joseph AK. 3-Color Mohs Mapping Method to Uniquely Stain up to 6 Specimens. Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al.]. 2021 Aug 1:47(8):1107-1108. doi: 10.1097/DSS.0000000000002951. Epub [PubMed PMID: 33625142]
Neill BC, Seger EW, Roberts EE, Tolkachjov SN. Assessment of Mohs micrographic surgery mapping concordance between surgeon and trainee using transparent writing boards. Journal of the American Academy of Dermatology. 2023 Jul:89(1):e25-e26. doi: 10.1016/j.jaad.2021.02.052. Epub 2021 Feb 22 [PubMed PMID: 33631217]
Jibbe A, Donnelly H. A Novel Technique to Improve Accuracy of Mohs Mapping for Large Stages with a Small Tumor Burden. Journal of cutaneous and aesthetic surgery. 2020 Apr-Jun:13(2):160-162. doi: 10.4103/JCAS.JCAS_75_19. Epub [PubMed PMID: 32792779]
Govas P, Ha MV, Wessel CB, Hurst A, Gordon BR, Carroll BT. Reported Outcome Measures in Mohs Micrographic Surgery in Studies With Defined Techniques for Embedding and Processing of Tissue: A Systematic Review. Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al.]. 2023 Dec 1:49(12):1116-1121. doi: 10.1097/DSS.0000000000004013. Epub 2023 Nov 9 [PubMed PMID: 37962132]
Level 1 (high-level) evidenceAslam A, Aasi SZ. Frozen-Section Tissue Processing in Mohs Surgery. Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al.]. 2019 Dec:45 Suppl 2():S57-S69. doi: 10.1097/DSS.0000000000002260. Epub [PubMed PMID: 31764292]
Highsmith JT, Highsmith MJ, Monheit GD. Histologic Accuracy of Mohs Micrographic Surgery. Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al.]. 2018 Mar:44(3):350-353. doi: 10.1097/DSS.0000000000001352. Epub [PubMed PMID: 29016546]
Darsha AK, Pousti BT, Loh TY, Hau JT, Brian Jiang SI. Removal of Incidental Skin Cancer During Mohs Micrographic Surgery Indicated for a Different Primary Tumor. Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al.]. 2024 Apr 1:50(4):327-330. doi: 10.1097/DSS.0000000000004081. Epub 2024 Jan 23 [PubMed PMID: 38261759]
Hardin CA, Neiner JR. How We Do It: 3-Nick Technique for Mohs Tissue Mapping. Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al.]. 2018 Aug:44(8):1142-1144. doi: 10.1097/DSS.0000000000001444. Epub [PubMed PMID: 29293105]
Li JY, Silapunt S, Migden MR, McGinness JL, Nguyen TH. Mohs Mapping Fidelity: Optimizing Orientation, Accuracy, and Tissue Identification in Mohs Surgery. Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al.]. 2018 Jan:44(1):1-9. doi: 10.1097/DSS.0000000000001215. Epub [PubMed PMID: 28654580]
Dietert JB, MacFarlane DF. A Survey of Mohs Tissue Tracking Practices. Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al.]. 2019 Apr:45(4):514-518. doi: 10.1097/DSS.0000000000001723. Epub [PubMed PMID: 30550521]
Level 3 (low-level) evidenceZabielinski M, Leithauser L, Godsey T, Gloster HM Jr. Laboratory errors leading to nonmelanoma skin cancer recurrence after Mohs micrographic surgery. Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al.]. 2015 Aug:41(8):913-6. doi: 10.1097/DSS.0000000000000428. Epub [PubMed PMID: 26218725]
Geers T, Humeda J, Brown TS. The Slide Review Protocol: Improving Patient Safety Outcomes in Mohs Micrographic Surgery. Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al.]. 2024 Apr 1:50(4):383-384. doi: 10.1097/DSS.0000000000004079. Epub 2024 Jan 30 [PubMed PMID: 38288961]