EMS Canine Evaluation of Oxygen Saturation (SpO2)
EMS Canine Evaluation of Oxygen Saturation (SpO2)
Introduction
Prudent emergency medical personnel are prepared to provide canine first-aid and life-saving interventions until the canine can be transferred to the nearest veterinary treatment facility. EMS, Police, and medical providers associated with organizations utilizing "working dogs" are frequently called to assist in emergent canine care. Civilian and military medical centers operating near facilities with working dogs, police K9 units, or search and rescue operations should be prepared for the imminent threat of emergent canine injuries and illness. Well-prepared medical personnel and facilities will aim to achieve similar standards and monitoring provided for humans in their emergent canine care—including pulse oximetry.
Pulse oximetry is a noninvasive method for monitoring blood oxygen saturation (SpO2). A pulse oximeter algorithmically estimates oxygen saturation in the blood based on photoplethysmographic pulses and wavelengths of light absorption by deoxygenated and oxygenated hemoglobin.[1] Pulse oximetry is primarily used in place of arterial blood gas measurement of arterial oxygen saturation (SaO2).[2] Pulse oximetry is more convenient, safe, and inexpensive than invasive arterial blood gas collection.[3] Pulse oximetry is considered reliable and sufficiently accurate to detect a significant decline in respiratory function (approximately 2%-4% expected error in clinical studies and an accuracy of 2% in 95% of cases per the manufacturer).[1] Pulse oximetry monitoring is considered the standard of care in patients receiving anesthesia, resuscitation, and respiratory monitoring to assess blood oxygenation.
Overall, the technique and normal pulse oximetry ranges are similar to human medical care. The most significant difference is human pulse oximetry is commonly performed on the fingernail bed; other tissues must be utilized for canine care.
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
Adept medical personnel are familiar with the basics of canine anatomy and physiology. Fortunately, canines have a similar cardiorespiratory system compared to humans. Air passes through the canine nares and oropharynx to the trachea and bilateral lungs. After this, the oxygenated blood will move throughout the canine circulatory system and oxygenate the tissue and organs of the body. The blood oxygenation level measured by pulse oximetry is a quick indicator of the global status of the canine's health. The normal canine oxygenation ranges from 94% to 100%. Deviations from this range may indicate a compromised cardiorespiratory system.
Indications
Pulse oximetry is a valuable, noninvasive tool to monitor a canine's SpO2. Pulse oximetry and SpO2 are essential in the early detection of hypoxemia and titration of supplemental oxygen.[1][4][5][6][7][8] Pulse oximetry allows medical personnel to assess the canine's respiratory status and monitor the effectiveness of oxygen therapy. Pulse oximetry is the standard of care in monitoring respiratory and circulatory function. Pulse oximetry guides several categories of therapeutic interventions, including emergent resuscitation, sedation, mechanical ventilation and oxygen therapy, intraoperative procedures, and anesthetic care.[7][8][9][10][11]
If utilizing anesthesia or sedating medications, it is essential to use pulse oximetry to monitor the canine for hypoxemia and guide oxygen therapy. Clinical studies show that using pulse oximetry reduces the rate of adverse outcomes related to undiagnosed hypoxic events and decreases mortality rates when used with oxygen administration.[12][13][6][14][15]
Contraindications
While utilizing SpO2 in humans and canines is a relatively safe, quick, and noninvasive procedure, several clinical situations limit the pulse oximeter's ability to obtain an accurate reading. If the comical situation allows, do not place the pulse oximetry sensor on an injured extremity or burned skin, which could have compromised blood flow and tissue perfusion.
SpO2 measurements can be inaccurate in several situations analogous to human medical scenarios, such as critically ill patients with low perfusion, cold skin, dark skin, motion artifacts, and dyshemoglobins.[1][16][17][18] Pulse oximetry sensors can only differentiate oxygenated and deoxygenated hemoglobin; the sensor cannot detect carboxyhemoglobin or methemoglobin.[19]
Due to a canine's fur and hair, canine pulse oximetry is limited by poor sensor contact and light penetration through tissue. Canines might also require sedating medications or anxiolysis to tolerate the application of medical devices and sensors and remain still during the medical exam. Studies have shown that a canine with a chronic history of vascular disease can also have an inaccurate reading on pulse oximetry. Overall, a pulse oximeter falsely detects hypoxemia during motion and low-perfusion conditions. Medical personnel should be aware of these limitations and be prepared to use alternative methods to assess for hypoxemia.
Additionally, pulse oximetry measures oxygenation levels but not ventilation or carbon dioxide levels in the blood (PaO2). In conjunction with a pulse oximeter, capnography, or end-tidal CO2 (ETCO2), is used to evaluate the canine's ventilation status with a CO2 waveform and PCO2 level.[19]
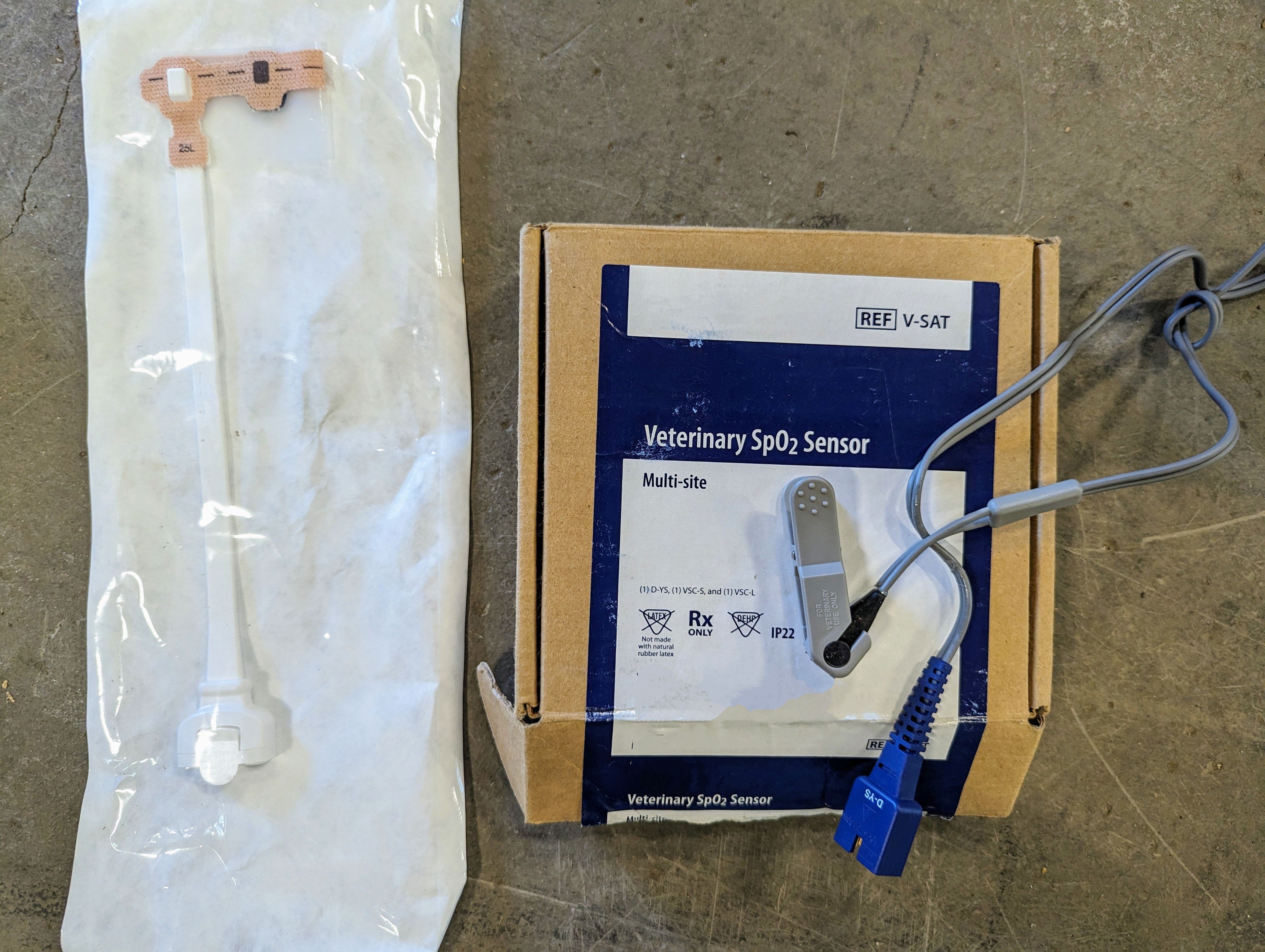
Equipment
Medical personnel should be equipped with commercial oximeters designed for canines. These devices ensure proper placement on a canine's tongue, lip, ear, and even the prepuce vulva or webbing of the toes. These mucous membranes allow light to be emitted to measure oxygen saturation levels. If it becomes a situation in which a company needs to ensure the proper equipment is purchased, an adhesive, elastic infant pulse oximeter can be used as well. Commercial human pulse oximeters provide less accurate results when used on a canine.
By spectrophotometry and the Beer-Lambert Law, a pulse oximeter measures peripheral functional hemoglobin or arterial blood oxygen saturation (SpO2).[2][20] The oxygen saturation from this noninvasive monitor estimates tissue oxygenation. Modern pulse oximeters are lightweight, portable, inexpensive, and provide rapid measurements [2]. The probes are adhesive single-use probes or multi-use clips.[5] Canine pulse oximetry probes are optimized for canine anatomy and hair and should be used when available. The pulse oximeter emits 2 lights and detects light wavelengths on the opposite side of the tissue bed with one sensor.[20][21]
Personnel
Emergent canine care requires a team of 2 or more medical personnel. Best practice integrates the working dog's handler and telemedicine consults for veterinary assistance. The canine’s handler should assist the medical team by placing a breathable muzzle and restraining the canine to ensure the safety of medical personnel and the dog.
Technique or Treatment
The first step in canine assessment is to apply a muzzle. The canine's handler should be asked to place a muzzle and restrain the dog to protect care providers and other team members assisting.
Appropriate sites for canine pulse oximetry probe placement (in order of preference) are the tongue, nonpigmented area of lip, ear pinna, prepuce (male), or vulva (female). In reality, accurate pulse oximetry probes placed on the tongue are only achievable on an unconscious or sedated/anesthetized canine. Human commercial neonatal pulse oximetry adhesive sensors attached to the base of a canine's tail may provide an alternative site.
The pulse oximeter probe should be placed so the light penetrates through tissue directly to the detector. The probe should be adequately secured to the tissue to provide a stable connection and accurate reading. The probe should fit well but not constrict or restrict circulation [8]. Ambient light and excessive movement can interfere with readings. Manufacturer guidelines for all probes should be used to ensure an appropriate probe placement and reading accuracy.
Clinical Significance
Normal canine oxygen saturation levels at sea level are 94% to 100% on room air, similar to humans.[20] Critical levels of 80% correlate to a partial pressure of 60 mm Hg and would prompt interventions for hypoxemia.[20]
Pulse oximeters are generally reliable and accurate; however, they are not calibrated to assess critically low blood oxygen saturation levels. Pulse oximeter readings of less than 70% are not considered accurate.[1][20] At critically low oxygen saturation levels, arterial blood gas measurements are considered more accurate, and the gold standard of determining oxygen saturation is clinically warranted.[3]
Enhancing Healthcare Team Outcomes
Proper training, quality equipment, and adherence to technique and treatment protocols are essential for accurate and effective SpO2 monitoring. While there are challenges and limitations associated with canine SPO2 monitoring, it remains a valuable tool in emergent canine care. SpO2 monitoring in canine casualties can significantly improve patient outcomes and survival rates. Further research and clinical studies are needed to explore the accuracy and efficacy of canine pulse oximetry in different clinical scenarios and to establish standardized protocols and guidelines for its use in emergency canine care. Medical personnel should stay updated on the latest techniques and guidelines related to canine pulse oximetry.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Nitzan M, Romem A, Koppel R. Pulse oximetry: fundamentals and technology update. Medical devices (Auckland, N.Z.). 2014:7():231-9. doi: 10.2147/MDER.S47319. Epub 2014 Jul 8 [PubMed PMID: 25031547]
Pesola GR, Sankari A. Oxygenation Status and Pulse Oximeter Analysis. StatPearls. 2023 Jan:(): [PubMed PMID: 37276303]
Castro D, Patil SM, Keenaghan M. Arterial Blood Gas. StatPearls. 2023 Jan:(): [PubMed PMID: 30725604]
Jubran A. Pulse oximetry. Critical care (London, England). 2015 Jul 16:19(1):272. doi: 10.1186/s13054-015-0984-8. Epub 2015 Jul 16 [PubMed PMID: 26179876]
Rackley CR. Monitoring During Mechanical Ventilation. Respiratory care. 2020 Jun:65(6):832-846. doi: 10.4187/respcare.07812. Epub [PubMed PMID: 32457174]
Jubran A. Pulse oximetry. Critical care (London, England). 1999:3(2):R11-R17 [PubMed PMID: 11094477]
Nielsen JR, Lim KS. Airway plans and capnography. Anaesthesia. 2019 Mar:74(3):397. doi: 10.1111/anae.14590. Epub [PubMed PMID: 30734942]
Hafen BB, Sharma S. Oxygen Saturation. StatPearls. 2023 Jan:(): [PubMed PMID: 30247849]
Tusman G, Bohm SH, Suarez-Sipmann F. Advanced Uses of Pulse Oximetry for Monitoring Mechanically Ventilated Patients. Anesthesia and analgesia. 2017 Jan:124(1):62-71 [PubMed PMID: 27183375]
Hasanin A, Mohamed SAR, El-Adawy A. Evaluation of perfusion index as a tool for pain assessment in critically ill patients. Journal of clinical monitoring and computing. 2017 Oct:31(5):961-965. doi: 10.1007/s10877-016-9936-3. Epub 2016 Sep 24 [PubMed PMID: 27665572]
Gelb AW, Morriss WW, Johnson W, Merry AF, Abayadeera A, Belîi N, Brull SJ, Chibana A, Evans F, Goddia C, Haylock-Loor C, Khan F, Leal S, Lin N, Merchant R, Newton MW, Rowles JS, Sanusi A, Wilson I, Velazquez Berumen A, International Standards for a Safe Practice of Anesthesia Workgroup. World Health Organization-World Federation of Societies of Anaesthesiologists (WHO-WFSA) International Standards for a Safe Practice of Anesthesia. Anesthesia and analgesia. 2018 Jun:126(6):2047-2055. doi: 10.1213/ANE.0000000000002927. Epub [PubMed PMID: 29734240]
Callahan JM. Pulse oximetry in emergency medicine. Emergency medicine clinics of North America. 2008 Nov:26(4):869-79, vii. doi: 10.1016/j.emc.2008.08.006. Epub [PubMed PMID: 19059087]
Enoch AJ, English M, Shepperd S. Does pulse oximeter use impact health outcomes? A systematic review. Archives of disease in childhood. 2016 Aug:101(8):694-700. doi: 10.1136/archdischild-2015-309638. Epub 2015 Dec 23 [PubMed PMID: 26699537]
Level 1 (high-level) evidenceMoller JT, Johannessen NW, Espersen K, Ravlo O, Pedersen BD, Jensen PF, Rasmussen NH, Rasmussen LS, Pedersen T, Cooper JB. Randomized evaluation of pulse oximetry in 20,802 patients: II. Perioperative events and postoperative complications. Anesthesiology. 1993 Mar:78(3):445-53 [PubMed PMID: 8457045]
Level 1 (high-level) evidenceTobin MJ, Laghi F, Jubran A. Why COVID-19 Silent Hypoxemia Is Baffling to Physicians. American journal of respiratory and critical care medicine. 2020 Aug 1:202(3):356-360. doi: 10.1164/rccm.202006-2157CP. Epub [PubMed PMID: 32539537]
Jamali H, Castillo LT, Morgan CC, Coult J, Muhammad JL, Osobamiro OO, Parsons EC, Adamson R. Racial Disparity in Oxygen Saturation Measurements by Pulse Oximetry: Evidence and Implications. Annals of the American Thoracic Society. 2022 Dec:19(12):1951-1964. doi: 10.1513/AnnalsATS.202203-270CME. Epub [PubMed PMID: 36166259]
Poorzargar K, Pham C, Ariaratnam J, Lee K, Parotto M, Englesakis M, Chung F, Nagappa M. Accuracy of pulse oximeters in measuring oxygen saturation in patients with poor peripheral perfusion: a systematic review. Journal of clinical monitoring and computing. 2022 Aug:36(4):961-973. doi: 10.1007/s10877-021-00797-8. Epub 2022 Feb 4 [PubMed PMID: 35119597]
Level 1 (high-level) evidenceBickler P, Tremper KK. The Pulse Oximeter Is Amazing, but Not Perfect. Anesthesiology. 2022 May 1:136(5):670-671. doi: 10.1097/ALN.0000000000004171. Epub [PubMed PMID: 35303063]
Pandya NK, Sharma S. Capnography and Pulse Oximetry. StatPearls. 2023 Jan:(): [PubMed PMID: 30969576]
Torp KD, Modi P, Pollard EJ, Simon LV. Pulse Oximetry. StatPearls. 2023 Jan:(): [PubMed PMID: 29262014]
Chan ED, Chan MM, Chan MM. Pulse oximetry: understanding its basic principles facilitates appreciation of its limitations. Respiratory medicine. 2013 Jun:107(6):789-99. doi: 10.1016/j.rmed.2013.02.004. Epub 2013 Mar 13 [PubMed PMID: 23490227]
Level 3 (low-level) evidence