Introduction
Canine cardiopulmonary resuscitation (CPR) represents an emergency procedure that, if delivered correctly, can significantly increase the chances of survival in dogs suffering from cardiopulmonary arrest (CPA).[1] In 2012, the Reassessment Campaign on Veterinary Resuscitation (RECOVER) initiative published the first evidence-based, consensus guideline for CPR in small animals.[2] This initiative provides standardized guidelines to decrease the variability in the approach to canine CPR. While this initiative offers five domains of CPR for dogs, the discussion here is primarily limited to Basic Life Support (BLS) measures. BLS includes recognizing CPA, initiating chest compressions, airway management, and providing ventilation. BLS can be provided by both lay rescuers and medical professionals.
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
Two main theories exist to describe how external chest compressions produce blood flow during canine CPR. The cardiac pump theory states that the ventricles are directly compressed during chest compressions, causing blood to be advanced through the circulatory system. The exact mechanism depends on the position of the canine. Cardiac pump theory postulates that the ventricles are compressed between the sternum and spine in the dorsal recumbent position and between the ribs in the lateral recumbent position. The thoracic pump theory suggests that pressure changes in the chest mediate flow rather than blood flowing from direct compression of the ventricles. As the chest is compressed, overall intrathoracic pressure increases, exerting that force upon the ventricles and the aorta and collapsing the vena cava, causing blood to flow out of the thorax.[3][4][5]
Allowing full recoil of the chest when performing CPR creates negative pressure in the thoracic cavity. This produces a gradient favoring blood returning from the peripheral to central circulation and into the cardiopulmonary circulation, allowing oxygen and carbon dioxide exchange. The evidence on the predominant mechanism in canine CPR is limited, but both proposed mechanisms likely contribute to blood flow in most cases.
Experimental evidence demonstrated higher left ventricular pressures and aortic blood flow when compressions were administered to canines placed in the lateral recumbent position compared to those in the dorsal recumbent position. Additionally, clinical data shows higher rates of ROSC when canines were placed in the lateral recumbent position.[5] Although there is little published evidence, profound anatomic differences between dog breeds suggest that there may be some benefit to different canine positioning and rescuer hand placement when administering chest compressions.[6]
Direct compression of the heart is difficult in most medium and large breeds, given the size of their thorax. In this case, the thoracic pump mechanism likely predominates. These dogs should be placed in either left or right lateral recumbency, and the rescuer's hands should be placed over the widest portion of the thorax to administer compressions to maximize intrathoracic pressure.[6]
Indications
Canine CPR should be initiated in cases of non-traumatic cardiopulmonary arrest. If resources and the situation allow, rescuers may consider CPR in canines with cardiac arrest secondary to traumatic causes but should understand that successful resuscitation is unlikely. Indications for CPR include a canine that is unresponsive and apneic or exhibiting agonal breathing.[1][7] Due to the difficulty of palpating a canine's pulse and obtaining an electrocardiogram (ECG) to confirm CPA, rescuers should not delay initiating CPR in an unresponsive and apneic canine to obtain these measures.[6][8]
Preparation
As for community emergency medical service (EMS) personnel, scene safety should be a top priority for rescuers attempting to intervene for a canine patient.[9] While tactical EMS personnel are prepared to operate in less secure environments than their civilian counterparts, rescuers should prepare to administer canine CPR by ensuring the scene is safe enough to do so.[10] Preparation of a canine patient, especially a law enforcement or military working dog, should include the utilization of a muzzle. Applying a muzzle before any evaluation or treatment attempts will help ensure a safe environment for rescuers and the canine.[11]
Technique or Treatment
Quick action is crucial as multiple studies in both human and animal patients have shown that early recognition of CPA and initiation of CPR is associated with increased rates of return of spontaneous circulation (ROSC), which is the primary goal of CPR.[12][13] Initial assessment of a canine that is apneic and unresponsive should begin with a rapid airway, breathing, and circulation (ABC) assessment, a mainstay of human BLS measures.[6]
Once CPA has been recognized, chest compressions should begin immediately. If doubt persists about whether the canine is experiencing CPA, CPR should be started without further delay, and the patient should be reassessed after an initial 2-minute cycle.
Most dog breeds, including breeds traditionally utilized as police and military working dogs, should be placed in the lateral recumbency position (lying on their side).[14] The rescuer's hands should be placed over the broadest part of the dog's chest.
Chest compressions should be delivered at 100-120 per minute. Experimental data in dogs shows increased ROSC and 24-hour survival rates when compressions were administered at rates of 100-120 per minute.[15] There is also some evidence to suggest that higher rates of up to 150 compressions per minute may be preferable. However, the rate should not fall below 100 per minute.
Compressions should achieve a depth of approximately half the width of the canine's thorax. Veterinary literature has demonstrated a linear relationship between mean arterial pressure and depth of chest compressions. This is also reflected in human clinical trials.[16][17][18] While the depth of the compressions is important, allowing full recoil of the chest between each compression is also vital. There are reductions in coronary and cerebral perfusion when rescuers do not allow the chest to recoil after compressions fully.[6][8]
Unless an intervention is made to ventilate the patient, canines requiring CPR will become hypoxic and hypercapnic. This will reduce the chances of achieving ROSC.[19][20] Securing the canine airway early in CPA is emphasized in the RECOVER guidelines. However, canine endotracheal intubation techniques will not be reviewed here. If the necessary supplies and trained rescuers are available, intubation should be attempted early. Rescuers may also consider a bag-valve mask, but achieving a tight fit with a mask designed for human patients may prove difficult. Studies have shown that ventilating canine patients during CPR with a poorly fitting mask does not provide effective rescue breaths. If intubation or other non-invasive ventilation methods are unavailable, rescuers may utilize "mouth-to-snout" rescue breathing.[21][22] While holding the dog's mouth closed with their hands, the rescuer should place their mouth over the canine's nares, creating a seal, and blow into the nares until a normal chest rise is achieved.[6][8] It is important to note that an injured canine may act unpredictably, and mouth-to-snout ventilation places the rescuer administering breaths in a particularly vulnerable position. At a minimum, a muzzle should be placed on the canine. Additionally, it is recommended that if the canine's handler can, they assist in resuscitation efforts.[23]
Canines that have been intubated should be ventilated at a rate of 10 breaths per minute or one breath delivered every 6 seconds. Breaths should be delivered in this case without any pause in compressions. If utilizing non-invasive ventilation or mouth-to-snout ventilations, 30 chest compressions should be delivered, followed by a brief pause in compressions to allow for 2 rescue breaths to be given. Emphasis should be placed on as few interruptions in compressions as possible to increase the chance of achieving ROSC.[24][25]
CPR should be continued in cycles of 2 minutes. Switching compressors after each 2-minute cycle has decreased the overall number of interruptions in compressions.[26] Rescuer fatigue has been shown to contribute to a decrease in the depth of compressions and an increase in leaning on the patient. Rescuer leaning does not allow for full chest recoil and impairs cardiac output.[27][28] This underscores the importance of switching compressors every 2 minutes.
Automatic External Defibrillator (AED) devices have been a part of human BLS for decades and are widely available.[29] The widespread adoption of AED education for the layperson and emphasis on early application in human out-of-hospital CPA is associated with a significant improvement in survival.[30] AEDs designed for human use are effective at recognizing shockable rhythms and delivering shocks to canine patients when used with ECG gel or clipping the fur. In one study evaluating AED effectiveness in canines, 90% of canines required both shaving of their fur and the application of ECG gel.[31] Trimming fur and applying gel makes AED application in the pre-hospital setting for canines more challenging than for a human patient. An AED is still a validated tool that can increase the chances of achieving ROSC if applied appropriately.
Once CPR has been initiated, the canine patient should be transported to a veterinary hospital as quickly and safely as possible. CPR should be continued until the canine becomes responsive and begins breathing spontaneously, or a veterinarian takes over care of the patient.
If ROSC is achieved, rescuers should seek veterinary care immediately and continue assessing their patients' ABCs. These canines are at extreme risk of CPA recurrence. The proportion of canine and feline patients that survive to discharge after ROSC ranges from 2% to 10%.[14][32] This highlights the increased risk for CPA recurrence as well as the importance of post-cardiac arrest (PCA) care.
While a veterinarian best delivers PCA care, rescuers should understand some fundamental concepts. PCA syndrome is believed to be the cause of such high mortality in PCA patients. It is described as a combination of multiorgan failure, anoxic brain injury, cardiogenic shock, and the sequelae of preexisting diseases.[33] Optimization of hemodynamics, respiratory function, body temperature, and neuroprotective therapies are the fundamentals of PCA care in the critical care setting.
Clinical Significance
Early cardiopulmonary resuscitation significantly increases survival in CPA.[34] The vast majority of canine CPR occurs in the veterinary hospital setting. Human studies have demonstrated that early initiation of CPR in the out-of-hospital setting increases the chances of achieving ROSC and the patient's full recovery.[35] Recognition of canine CPA and knowledge of the steps in canine CPR will equip rescuers to give these patients the best chance of achieving ROSC and, ultimately, survival.[6]
Enhancing Healthcare Team Outcomes
Many healthcare workers trained to treat human patients may be called on to act as first responders to a canine patient. Canine CPR shares many similarities with human CPR, and if done correctly, can save lives. The evidence available in human patient outcomes in out-of-hospital CPA shows that teams led by non-physicians in administering CPR are non-inferior to teams led by physicians.[36][37] While no studies have been conducted to assess these dynamics in veterinary medicine, the available data suggests that the most important aspect of team dynamics impacting patient outcomes lies not in who is leading the team but in how effectively the team communicates with one another. This includes establishing clear roles, utilizing focused, clear communication to task individuals specifically, and using closed-loop communication.[38]
Media
(Click Image to Enlarge)
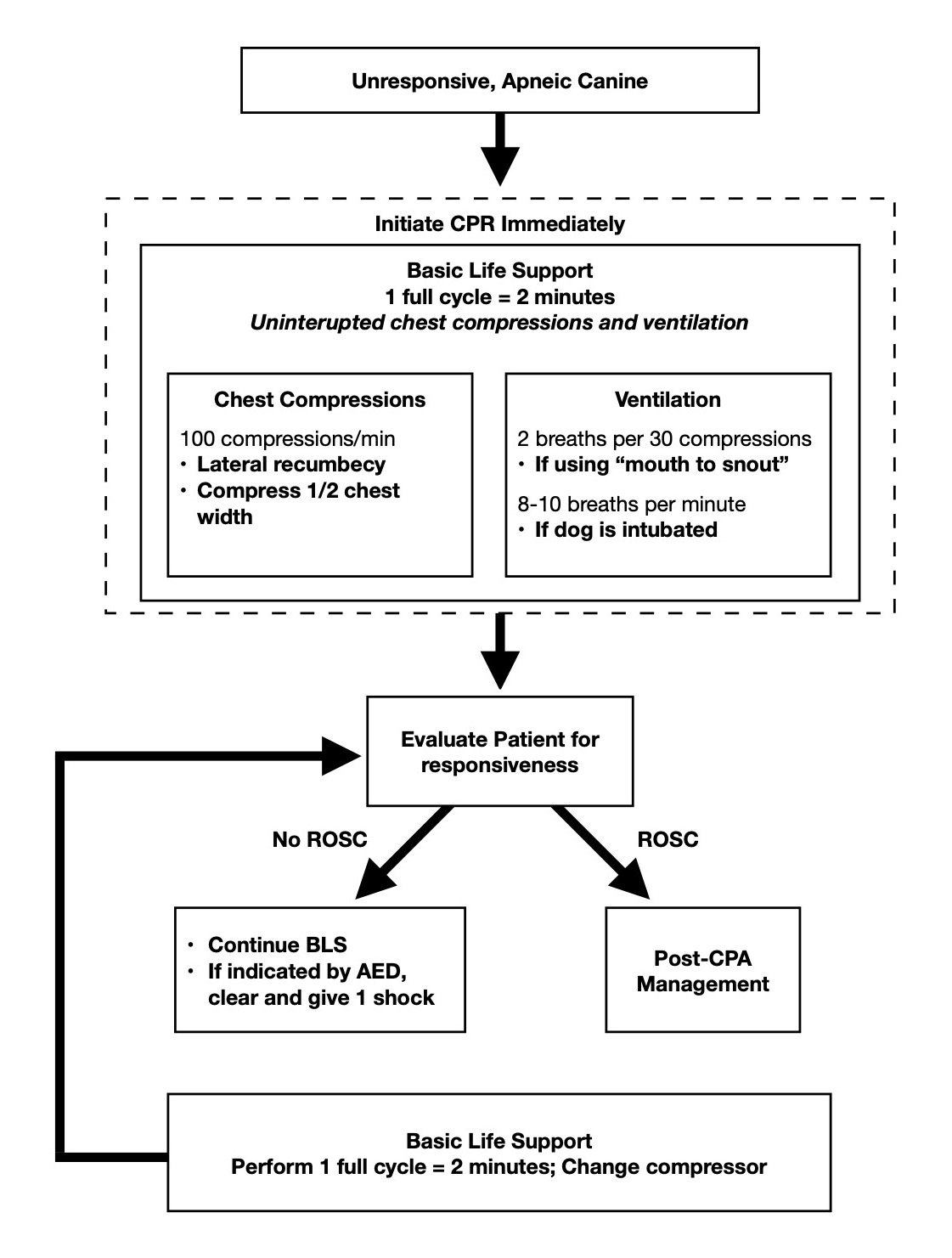
Canine CPR Algorithm
Adapted from Daniel J. Fletcher et al. RECOVER evidence and knowledge gap analysis on veterinary CPR. Part 7: Clinical guidelines. 07 June 2012.
References
Boller M, Boller EM, Oodegard S, Otto CM. Small animal cardiopulmonary resuscitation requires a continuum of care: proposal for a chain of survival for veterinary patients. Journal of the American Veterinary Medical Association. 2012 Mar 1:240(5):540-54. doi: 10.2460/javma.240.5.540. Epub [PubMed PMID: 22332623]
Level 3 (low-level) evidenceBoller M, Fletcher DJ. RECOVER evidence and knowledge gap analysis on veterinary CPR. Part 1: Evidence analysis and consensus process: collaborative path toward small animal CPR guidelines. Journal of veterinary emergency and critical care (San Antonio, Tex. : 2001). 2012 Jun:22 Suppl 1():S4-12. doi: 10.1111/j.1476-4431.2012.00758.x. Epub [PubMed PMID: 22676285]
Level 3 (low-level) evidenceCipani S, Bartolozzi C, Ballo P, Sarti A. Blood flow maintenance by cardiac massage during cardiopulmonary resuscitation: Classical theories, newer hypotheses, and clinical utility of mechanical devices. Journal of the Intensive Care Society. 2019 Feb:20(1):2-10. doi: 10.1177/1751143718778486. Epub 2018 Jun 18 [PubMed PMID: 30792756]
Criley JM. The thoracic pump provides a mechanism for coronary perfusion. Archives of internal medicine. 1995 Jun 12:155(11):1236 [PubMed PMID: 7763131]
Level 3 (low-level) evidenceMaier GW, Tyson GS Jr, Olsen CO, Kernstein KH, Davis JW, Conn EH, Sabiston DC Jr, Rankin JS. The physiology of external cardiac massage: high-impulse cardiopulmonary resuscitation. Circulation. 1984 Jul:70(1):86-101 [PubMed PMID: 6723014]
Level 3 (low-level) evidenceFletcher DJ, Boller M, Brainard BM, Haskins SC, Hopper K, McMichael MA, Rozanski EA, Rush JE, Smarick SD, American College of Veterinary Medicine, Veterinary Emergency and Critical Care Society. RECOVER evidence and knowledge gap analysis on veterinary CPR. Part 7: Clinical guidelines. Journal of veterinary emergency and critical care (San Antonio, Tex. : 2001). 2012 Jun:22 Suppl 1():S102-31. doi: 10.1111/j.1476-4431.2012.00757.x. Epub [PubMed PMID: 22676281]
Level 3 (low-level) evidenceEisenberg MS. Incidence and significance of gasping or agonal respirations in cardiac arrest patients. Current opinion in critical care. 2006 Jun:12(3):204-6 [PubMed PMID: 16672777]
Level 3 (low-level) evidenceHopper K, Epstein SE, Fletcher DJ, Boller M, RECOVER Basic Life Support Domain Worksheet Authors. RECOVER evidence and knowledge gap analysis on veterinary CPR. Part 3: Basic life support. Journal of veterinary emergency and critical care (San Antonio, Tex. : 2001). 2012 Jun:22 Suppl 1():S26-43. doi: 10.1111/j.1476-4431.2012.00753.x. Epub [PubMed PMID: 22676283]
Level 3 (low-level) evidenceKlein TA, Tadi P. EMS Scene Safety. StatPearls. 2023 Jan:(): [PubMed PMID: 32491547]
Rinnert KJ, Hall WL 2nd. Tactical emergency medical support. Emergency medicine clinics of North America. 2002 Nov:20(4):929-52 [PubMed PMID: 12476888]
Taylor WM. Canine tactical field care part three - thoracic and abdominal trauma. Journal of special operations medicine : a peer reviewed journal for SOF medical professionals. 2010 Winter:10(1):50-8 [PubMed PMID: 20306416]
Level 3 (low-level) evidenceHinchey PR, Myers JB, Lewis R, De Maio VJ, Reyer E, Licatese D, Zalkin J, Snyder G, Capital County Research Consortium. Improved out-of-hospital cardiac arrest survival after the sequential implementation of 2005 AHA guidelines for compressions, ventilations, and induced hypothermia: the Wake County experience. Annals of emergency medicine. 2010 Oct:56(4):348-57. doi: 10.1016/j.annemergmed.2010.01.036. Epub 2010 Mar 31 [PubMed PMID: 20359771]
Level 2 (mid-level) evidenceAufderheide TP, Yannopoulos D, Lick CJ, Myers B, Romig LA, Stothert JC, Barnard J, Vartanian L, Pilgrim AJ, Benditt DG. Implementing the 2005 American Heart Association Guidelines improves outcomes after out-of-hospital cardiac arrest. Heart rhythm. 2010 Oct:7(10):1357-62. doi: 10.1016/j.hrthm.2010.04.022. Epub 2010 Apr 24 [PubMed PMID: 20420938]
Hofmeister EH, Brainard BM, Egger CM, Kang S. Prognostic indicators for dogs and cats with cardiopulmonary arrest treated by cardiopulmonary cerebral resuscitation at a university teaching hospital. Journal of the American Veterinary Medical Association. 2009 Jul 1:235(1):50-7. doi: 10.2460/javma.235.1.50. Epub [PubMed PMID: 19566454]
Level 3 (low-level) evidenceFeneley MP, Maier GW, Kern KB, Gaynor JW, Gall SA Jr, Sanders AB, Raessler K, Muhlbaier LH, Rankin JS, Ewy GA. Influence of compression rate on initial success of resuscitation and 24 hour survival after prolonged manual cardiopulmonary resuscitation in dogs. Circulation. 1988 Jan:77(1):240-50 [PubMed PMID: 3335070]
Level 3 (low-level) evidenceBabbs CF, Voorhees WD, Fitzgerald KR, Holmes HR, Geddes LA. Relationship of blood pressure and flow during CPR to chest compression amplitude: evidence for an effective compression threshold. Annals of emergency medicine. 1983 Sep:12(9):527-32 [PubMed PMID: 6614604]
Level 3 (low-level) evidenceEdelson DP, Abella BS, Kramer-Johansen J, Wik L, Myklebust H, Barry AM, Merchant RM, Hoek TL, Steen PA, Becker LB. Effects of compression depth and pre-shock pauses predict defibrillation failure during cardiac arrest. Resuscitation. 2006 Nov:71(2):137-45 [PubMed PMID: 16982127]
Ristagno G, Tang W, Chang YT, Jorgenson DB, Russell JK, Huang L, Wang T, Sun S, Weil MH. The quality of chest compressions during cardiopulmonary resuscitation overrides importance of timing of defibrillation. Chest. 2007 Jul:132(1):70-5 [PubMed PMID: 17550931]
Level 3 (low-level) evidenceYeh ST, Cawley RJ, Aune SE, Angelos MG. Oxygen requirement during cardiopulmonary resuscitation (CPR) to effect return of spontaneous circulation. Resuscitation. 2009 Aug:80(8):951-5. doi: 10.1016/j.resuscitation.2009.05.001. Epub 2009 Jun 10 [PubMed PMID: 19520479]
Level 3 (low-level) evidenceIdris AH, Wenzel V, Becker LB, Banner MJ, Orban DJ. Does hypoxia or hypercarbia independently affect resuscitation from cardiac arrest? Chest. 1995 Aug:108(2):522-8 [PubMed PMID: 7634893]
Level 3 (low-level) evidenceHopper K, Rezende ML, Borchers A, Epstein SE. Efficacy of Manual Ventilation Techniques During Cardiopulmonary Resuscitation in Dogs. Frontiers in veterinary science. 2018:5():239. doi: 10.3389/fvets.2018.00239. Epub 2018 Oct 1 [PubMed PMID: 30327772]
Smarick SD, Rylander H, Burkitt JM, Scott NE, Woelz JS, Jandrey KE, Aldrich J, Sturges BK. Treatment of traumatic cervical myelopathy with surgery, prolonged positive-pressure ventilation, and physical therapy in a dog. Journal of the American Veterinary Medical Association. 2007 Feb 1:230(3):370-4 [PubMed PMID: 17269868]
Level 3 (low-level) evidenceLagutchik M, Baker J, Balser J, Burghardt W, Enroth M, Flournoy S, Giles J, Grimm P, Hiniker J, Johnson J, Mann K, Takara M, Thomas T. Trauma Management of Military Working Dogs. Military medicine. 2018 Sep 1:183(suppl_2):180-189. doi: 10.1093/milmed/usy119. Epub [PubMed PMID: 30189081]
Morgan RW, Landis WP, Marquez A, Graham K, Roberts AL, Lauridsen KG, Wolfe HA, Nadkarni VM, Topjian AA, Berg RA, Kilbaugh TJ, Sutton RM. Hemodynamic effects of chest compression interruptions during pediatric in-hospital cardiopulmonary resuscitation. Resuscitation. 2019 Jun:139():1-8. doi: 10.1016/j.resuscitation.2019.03.032. Epub 2019 Apr 1 [PubMed PMID: 30946924]
Christenson J, Andrusiek D, Everson-Stewart S, Kudenchuk P, Hostler D, Powell J, Callaway CW, Bishop D, Vaillancourt C, Davis D, Aufderheide TP, Idris A, Stouffer JA, Stiell I, Berg R, Resuscitation Outcomes Consortium Investigators. Chest compression fraction determines survival in patients with out-of-hospital ventricular fibrillation. Circulation. 2009 Sep 29:120(13):1241-7. doi: 10.1161/CIRCULATIONAHA.109.852202. Epub 2009 Sep 14 [PubMed PMID: 19752324]
Level 2 (mid-level) evidenceSavatmongkorngul S, Yuksen C, Chumkot S, Atiksawedparit P, Jenpanitpong C, Watcharakitpaisan S, Kaninworapan P, Maijan K. Comparison of chest compression quality between 2-minute switch and rescuer fatigue switch: A randomized controlled trial. International journal of critical illness and injury science. 2022 Jan-Mar:12(1):22-27. doi: 10.4103/ijciis.ijciis_56_21. Epub 2022 Mar 24 [PubMed PMID: 35433400]
Level 1 (high-level) evidenceFried DA, Leary M, Smith DA, Sutton RM, Niles D, Herzberg DL, Becker LB, Abella BS. The prevalence of chest compression leaning during in-hospital cardiopulmonary resuscitation. Resuscitation. 2011 Aug:82(8):1019-24. doi: 10.1016/j.resuscitation.2011.02.032. Epub 2011 Apr 8 [PubMed PMID: 21482010]
Zuercher M, Hilwig RW, Ranger-Moore J, Nysaether J, Nadkarni VM, Berg MD, Kern KB, Sutton R, Berg RA. Leaning during chest compressions impairs cardiac output and left ventricular myocardial blood flow in piglet cardiac arrest. Critical care medicine. 2010 Apr:38(4):1141-6. doi: 10.1097/CCM.0b013e3181ce1fe2. Epub [PubMed PMID: 20081529]
Level 3 (low-level) evidenceCraig-Brangan KJ, Day MP. AHA update: BLS, ACLS, and PALS. Nursing. 2021 Jun 1:51(6):24-30. doi: 10.1097/01.NURSE.0000751340.92329.ae. Epub [PubMed PMID: 34014872]
Rao P, Kern KB. Improving Community Survival Rates from Out-of-Hospital Cardiac Arrest. Current cardiology reviews. 2018:14(2):79-84. doi: 10.2174/1573403X14666180507160555. Epub [PubMed PMID: 29737258]
LeSueur MC, Rozanski EA, Karlin ET, LaMastro J, Rush JE. Evaluation of automated external defibrillator designed for people in dogs. Journal of veterinary emergency and critical care (San Antonio, Tex. : 2001). 2023 Mar:33(2):173-179. doi: 10.1111/vec.13285. Epub 2023 Feb 23 [PubMed PMID: 36815755]
Kawase K, Ujiie H, Takaki M, Yamashita K. Clinical outcome of canine cardiopulmonary resuscitation following the RECOVER clinical guidelines at a Japanese nighttime animal hospital. The Journal of veterinary medical science. 2018 Mar 30:80(3):518-525. doi: 10.1292/jvms.17-0107. Epub 2018 Jan 29 [PubMed PMID: 29375087]
Level 2 (mid-level) evidenceNeumar RW, Nolan JP, Adrie C, Aibiki M, Berg RA, Böttiger BW, Callaway C, Clark RS, Geocadin RG, Jauch EC, Kern KB, Laurent I, Longstreth WT Jr, Merchant RM, Morley P, Morrison LJ, Nadkarni V, Peberdy MA, Rivers EP, Rodriguez-Nunez A, Sellke FW, Spaulding C, Sunde K, Vanden Hoek T. Post-cardiac arrest syndrome: epidemiology, pathophysiology, treatment, and prognostication. A consensus statement from the International Liaison Committee on Resuscitation (American Heart Association, Australian and New Zealand Council on Resuscitation, European Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Asia, and the Resuscitation Council of Southern Africa); the American Heart Association Emergency Cardiovascular Care Committee; the Council on Cardiovascular Surgery and Anesthesia; the Council on Cardiopulmonary, Perioperative, and Critical Care; the Council on Clinical Cardiology; and the Stroke Council. Circulation. 2008 Dec 2:118(23):2452-83. doi: 10.1161/CIRCULATIONAHA.108.190652. Epub 2008 Oct 23 [PubMed PMID: 18948368]
Level 3 (low-level) evidenceHolmberg M, Holmberg S, Herlitz J. Effect of bystander cardiopulmonary resuscitation in out-of-hospital cardiac arrest patients in Sweden. Resuscitation. 2000 Sep:47(1):59-70 [PubMed PMID: 11004382]
Yan S, Gan Y, Jiang N, Wang R, Chen Y, Luo Z, Zong Q, Chen S, Lv C. The global survival rate among adult out-of-hospital cardiac arrest patients who received cardiopulmonary resuscitation: a systematic review and meta-analysis. Critical care (London, England). 2020 Feb 22:24(1):61. doi: 10.1186/s13054-020-2773-2. Epub 2020 Feb 22 [PubMed PMID: 32087741]
Level 1 (high-level) evidenceDickinson ET, Schneider RM, Verdile VP. The impact of prehospital physicians on out-of-hospital nonasystolic cardiac arrest. Prehospital emergency care. 1997 Jul-Sep:1(3):132-5 [PubMed PMID: 9709354]
Level 2 (mid-level) evidenceOlasveengen TM, Lund-Kordahl I, Steen PA, Sunde K. Out-of hospital advanced life support with or without a physician: effects on quality of CPR and outcome. Resuscitation. 2009 Nov:80(11):1248-52. doi: 10.1016/j.resuscitation.2009.07.018. Epub 2009 Aug 26 [PubMed PMID: 19709795]
Level 1 (high-level) evidenceHunziker S, Johansson AC, Tschan F, Semmer NK, Rock L, Howell MD, Marsch S. Teamwork and leadership in cardiopulmonary resuscitation. Journal of the American College of Cardiology. 2011 Jun 14:57(24):2381-8. doi: 10.1016/j.jacc.2011.03.017. Epub [PubMed PMID: 21658557]