Introduction
Pacemakers are electronic devices that stimulate the heart with electrical impulses to maintain or restore a normal heartbeat. In 1952, Zoll described an effective means of supporting the patients with intrinsic cardiac pacemaker activity and/or conducting tissue by an artificial, electric, external pacemaker. The pacing of the heart was accomplished by subcutaneous electrodes but could be maintained only for a short period. In 1957, complete heart block was treated using electrodes directly attached to the heart. These early observations instilled the idea that cardiac electrical failure can be controlled. It ultimately led to the development of totally implantable pacemaker by Chardack, Gage, and Greatbatch. Since then, there have been several advancements in the pacemakers, and the modern-day permanent pacemaker is subcutaneously placed device.[1][2][3]There are 3 types of artificial pacemakers:
- Implantable pulse generators with endocardial or myocardial electrodes
- External, miniaturized, patient portable, battery-powered, pulse generators with exteriorized electrodes for temporary transvenous endocardial or transthoracic myocardial pacing
- Console battery or AC-powered cardioverters or monitors with high-current external transcutaneous or low-current endocardial or myocardial circuits for temporary pacing in asynchronous or demand modes, with manual or triggered initiation of pacing
All cardiac pacemakers consist of 2 components: a pulse generator which provides the electrical impulse for myocardial stimulation and 1 or more electrodes or leads which deliver the electrical impulse from the generator to the myocardium. This discussion focuses on the indications of pacemaker placement.
Indications
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Indications
The most common indications for permanent pacemaker implantation are sinus node dysfunction (SND) and high-grade atrioventricular (AV) block. Guidelines for implantation of cardiac pacemakers have been established by a task force formed jointly by the American College of Cardiology (ACC), the American Heart Association (AHA), and the Heart Rhythm Society (HRS). The European Society of Cardiology has established similar guidelines. [4] ACC/AHA/HRS divides indications of pacemaker implantation into 3 specific classes:
- Class I: These are conditions where implantation of a pacemaker is considered necessary and beneficial (benefits much greater than risks).
- Class II: These are conditions where placement is indicated, but there is conflicting evidence or divergence of opinion. In Class IIa weight of evidence is in favor of efficacy (benefits greater than risk), while in class IIb, the efficacy is less well established (benefits greater than or equal to the risks).
- Class III: These are conditions in which permanent pacing is not recommended, and in some cases, it may be harmful (risks greater than the benefits).
Following conditions are included in the ACC/AHA/HRS guidelines for the pacemaker insertion.[5][6][4][7][8] We will discuss Class I and II recommendations.
- Sinus node dysfunction
- Acquired Atrioventricular(AV) block
- Chronic bifascicular block
- After acute phase of myocardial infarction
- Neurocardiogenic syncope and hypersensitive carotid sinus syndrome
- Post cardiac transplantation
- Hypertrophic cardiomyopathy
- Pacing to detect and terminate tachycardia
- Cardiac resynchronization therapy in patients with severe systolic heart failure
- Patients with congenital heart disease
Sinus Node Dysfunction
Class I indications
- Documented symptomatic sinus bradycardia including frequent sinus pauses which produce symptoms and symptomatic sinus bradycardia that results from required drug therapy for medical condition
- Symptomatic chronotropic incompetence (failure to achieve 85% of age-predicted maximal heart rate during formal or informal stress test or inability to mount age appropriate heart rate during activities of daily living)
Class II indications
- Sinus bradycardia with heart rate less than 40, but no clear association between the symptoms and bradycardia
- Unexplained syncope when clinically significant abnormalities of sinus node function are discovered or provoked in electrophysiological (EP) studies
- Minimally symptomatic patients with chronic heart rate less than 40 while awake
Acquired Atrioventricular (AV) Block
Class I indications
- Complete third-degree AV block with or without symptoms.
- Symptomatic second degree AV block, Mobitz type I and II
- Exercise-induced second or third degree AV block in the absence of myocardial infarction
- Mobitz II with widened QRS complex
Class II indications
- Asymptomatic Mobitz type II with the narrow QRS complex.
- First degree AV block when there is a hemodynamic compromise.
- Asymptomatic second degree AV block at Intra or Infra-His levels found in EP studies
Chronic Bifascicular Block
Class I indications
- Advanced second-degree AV block or intermittent third-degree AV block
- Alternating bundle-branch block
- Type II second-degree AV block.
Class II indications
- In patients having syncope not demonstrated to be due to AV block when other likely causes have been excluded, specifically ventricular tachycardia (VT)
- Incidental finding at EP study of a markedly prolonged HV interval (greater than 100 ms) or pacing-induced infra-His block in asymptomatic patients. HV interval is conduction time from the His bundle which is located just below the AV node to first identifiable onset of ventricular activation
- Can be considered in patients with neuromuscular disease such as myotonic muscular dystrophy, Erb dystrophy and peroneal muscular dystrophy with bifascicular block or any fascicular block, with or without symptoms
After Acute Phase of Myocardial Infarction
Class I indications
- Permanent ventricular pacing for persistent second degree AV block in the His-Purkinje system with alternating bundle branch block or third degree AV block within or below the His-Purkinje system after the ST-segment elevation MI (STEMI)
- Permanent ventricular pacing for a transient advanced second or third-degree infranodal AV block and associated bundle branch block
- Permanent ventricular pacing for persistent and symptomatic second or third degree AV block
Class II indications
- Permanent ventricular pacing may be considered for the asymptomatic persistent second or third degree AV block at AV node level.
Neurocardiogenic Syncope and Hypersensitive Carotid Sinus Syndrome
Class I indications
- Recurrent syncope caused by spontaneously occurring carotid sinus stimulation and carotid sinus pressure that induces ventricular asystole of more than 3 seconds
Class II indications
- Reasonable in patients having syncope without clear and provocative event, and with a hypersensitive cardioinhibitory response of 3 seconds or longer
- Can be considered for significantly symptomatic neurocardiogenic syncope associated with bradycardia documented spontaneously or at the time of tilt-table testing
Post Cardiac Transplantation
Class I indications
- For persistent inappropriate or symptomatic bradycardia not expected to resolve and for other class I indications of permanent pacing.
Class II indications
- Can be considered when relative bradycardia is prolonged or recurrent, which limits rehabilitation or discharge after postoperative recovery.
- Can be considered for syncope after cardiac transplantation even when bradycardia has not been documented.
Hypertrophic Cardiomyopathy (HCM)
Class I indications
- Patients with HCM having Sinus node dysfunction and AV block
Class II indications
- Can be considered in medically refractory symptomatic patients with HCM and with significant resting or provoked left ventricular outflow tract obstruction
Pacing to Prevent Tachycardia
Class I indications
- For sustained pause dependent VT, with or without QT prolongation
Class II indications
- Reasonable for high-risk patients with congenital QT syndrome.
- Can be considered for prevention of symptomatic, drug refractory, recurrent atrial fibrillation in a patient with co-existing sinus node dysfunction
Cardiac Resynchronization Therapy (CRT) in Patients with Severe Systolic Heart Failure
Class I indications
- Patients with left ventricular ejection fraction (LVEF) of less than or equal to 35%, sinus rhythm, LBBB (left bundle branch block), New York Heart Association (NYHA) Class II, III or IV symptoms while on optimal medical therapy with a QRS duration of greater than or equal to 150 ms, CRT with or without ICD is indicated
Class II indications
- LVEF less than or equal to 35%, sinus rhythm, LBBB with NYHA Class III or IV symptoms while on optimal medical therapy and QRS duration of 120 to 149 ms, CRT with or without ICD is recommended.
- LVEF less than or equal to 35%, sinus rhythm, a non-LBBB pattern with a QRS greater than or equal to 150 ms, and NYHA class III/ambulatory class IV symptoms on GDMT
- Useful in patients with atrial fibrillation and LVEF less than or equal to 35% on GDMT if the patient requires ventricular pacing or otherwise meets CRT criteria and AV nodal ablation or pharmacologic rate control will allow near 100% ventricular pacing with CRT
- LVEF less than or equal to 35%, NYHA class III or IV while on optimal medical therapy and who have frequent dependence on ventricular pacing, CRT is reasonable
Congenital Heart Disease
Class I indications
- For advanced second or third-degree AV block associated with symptomatic bradycardia, ventricular dysfunction, or low cardiac output; also for advanced second or third-degree AV block which is not expected to resolve or persists for 7 days or longer after cardiac surgery
- For sinus node dysfunction with a correlation of symptoms during age inappropriate bradycardia
- Congenital third-degree AV block with a wide QRS escape rhythm, complex ventricular ectopy or ventricular dysfunction
- Congenital third-degree AV block in an infant with a ventricular rate of less than or equal to 55 bpm or with congenital heart disease with a ventricular rate of less than or equal to 70 bpm
Class II indications
- For patients with congenital heart disease and sinus bradycardia for the prevention of recurrent episodes of intra-atrial re-entrant tachycardia; sinus node dysfunction may be intrinsic or secondary to antiarrhythmic treatment.
- For congenital third-degree AV block beyond the first year of life with an average heart rate less than 50 bpm, abrupt pauses in ventricular rate which are 2 or 3 times the basic cycle length, or associated with symptoms due to chronotropic incompetence.
- May be considered for transient postoperative third-degree AV block that reverts to sinus rhythm with the residual bifascicular block.
- Considered for asymptomatic sinus bradycardia after biventricular repair of congenital heart disease in patients with a resting heart rate less than 40 bpm or with pauses in ventricular rate longer than 3 seconds
Contraindications
Like in any procedure, the insertion of pacemaker insertion should be chosen wisely for a particular patient. There are situations in which pacemaker insertion is not beneficial or is not enough data to support its use. These are sometimes also called class III indications in ACC/AHA/HRS guidelines or European Society of Cardiology guidelines.
- Sinus bradycardia without significant symptoms; asymptomatic first-degree AV block. [9]
- AV block that is expected to resolve and unlikely to recur example drug toxicity, Lyme disease, or transient increase in vagal tone
- A pacemaker is not indicated for sinus node dysfunction in patients with symptoms suggestive of bradycardia that have been documented to occur even in the absence of bradycardia.
- Asymptomatic second-degree Mobitz, type-I block
- Asymptomatic prolonged RR interval with atrial fibrillation or other causes of transient ventricular pauses
- Hypersensitive cardioinhibitory response to carotid sinus stimulation in the absence of symptoms or in the presence of vague symptoms such as dizziness, lightheadedness
- Asymptomatic bradycardia during the sleep
- CRT is not indicated in patients whose functional status and life expectancy are limited predominantly by non-cardiac conditions
- Right bundle branch block with left axis deviation without syncope or other symptoms compatible with intermittent AV block
- Long QT syndrome or Torsade de pointes due to reversible causes
- In the presence of an accessory pathway that has the capacity for rapid anterograde conduction
- Patients with NYHA class I or II symptoms and non-LBBB pattern with QRS duration less than 150 ms
Complications
The pacing and CRT are associated with complications. The majority of complications occur in the hospital or during first 6 months. Lead complications are the main reason for the re-implantation of the pacemaker and CRT devices. Other complications include, but are not limited to infections, hematoma formation, pericardial effusion or tamponade, pneumothorax, coronary sinus dissection, or perforation. Some old pacemakers are not MRI safe. [10]
Clinical Significance
Pacemaker implantation has shown a mortality benefit. The CARE-HF (Cardiac Resynchronization in Heart Failure) trial limited subjects to the QRS duration greater than 150 ms (89% of patients) or QRS duration 120 to 150 ms with echocardiographic evidence of dys-synchrony (11% of patients). It was the first study to show a significant (36%) reduction in the death rate for resynchronization therapy unaccompanied by backup defibrillation compared with guideline-directed medical therapy (GDMT). There has been evidence from the multiple randomized trials of CRT-D in patients with reduced LVEF and NYHA class II shows that CRT can provide functional improvement and decrease the risk of HF events and composite outcomes. In clinical trials, CRT-D has not shown improvement in NYHA class I Heart failure. The ACC/AHA/HRS guidelines from 2012 thoroughly reviewed the conditions of hypertrophic cardiomyopathy, arrhythmogenic right ventricular dysplasia/cardiomyopathy, genetic arrhythmia syndrome, terminal care, and congenital heart disease, and no changes were made as compared to 2008 guidelines in these conditions. There was a change in guidelines for indications of CRT insertion in the 2012 ACC/AHA/HRS guidelines as compared to 2008 guidelines. These are incorporated in the indications for pacemaker section mentioned above.
New guidelines recommend CRT in a patient with QRS duration greater than or equal to 150 ms instead of 120 ms based on multiple analysis/studies (class I indication). An additional difference in CRT recommendations includes patients with QRS duration greater than or equal to 150 ms with LBBB as class I indication. Newer guidelines based on multiple studies suggest that in patients who have QRS greater than or equal to 120 ms but does not have complete LBBB, the evidence of benefit from CRT is less compelling. The European Society of Cardiology guidelines are similar to the ACC/AHA/HRS guidelines, but there are few differences. One major difference noted is ESC guidelines have CRT indication for QRS less than or equal to 120 ms in patients with atrial fibrillation (in whom we have inadequate rate control requiring AV node ablation) and heart failure with EF less than or equal to 35%. The ACC/AHA/HRS guidelines have no such indication.
Enhancing Healthcare Team Outcomes
There are some areas where the indications for a pacemaker are clear, but there are few areas where clinical judgment and expertise plays a greater role. Although the guidelines attempt to define practices that meet the needs of most patients, the ultimate decision for the patient should be based on particular patient presenting scenario, clinician judgment, and discussion with the patient about risks and benefits of the procedure. There are specific pacemaker generators that are used for patients with AV block and sinus node dysfunction depending upon presentation. The different types of generators include a single chamber, dual chamber, and biventricular. A cardiology consult is highly recommended prior to the insertion of a pacemaker.
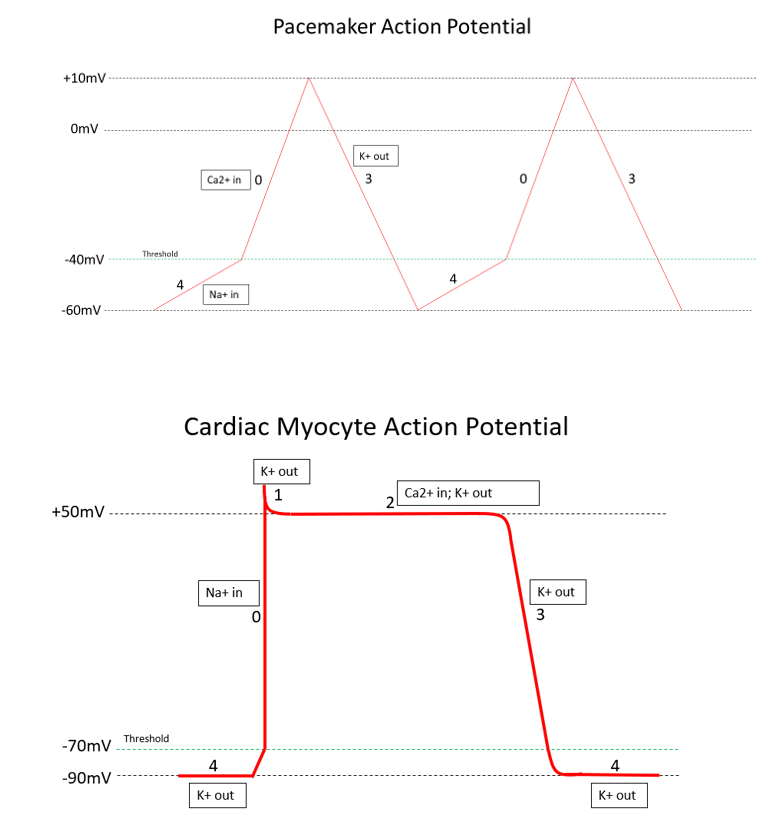
Media
(Click Image to Enlarge)
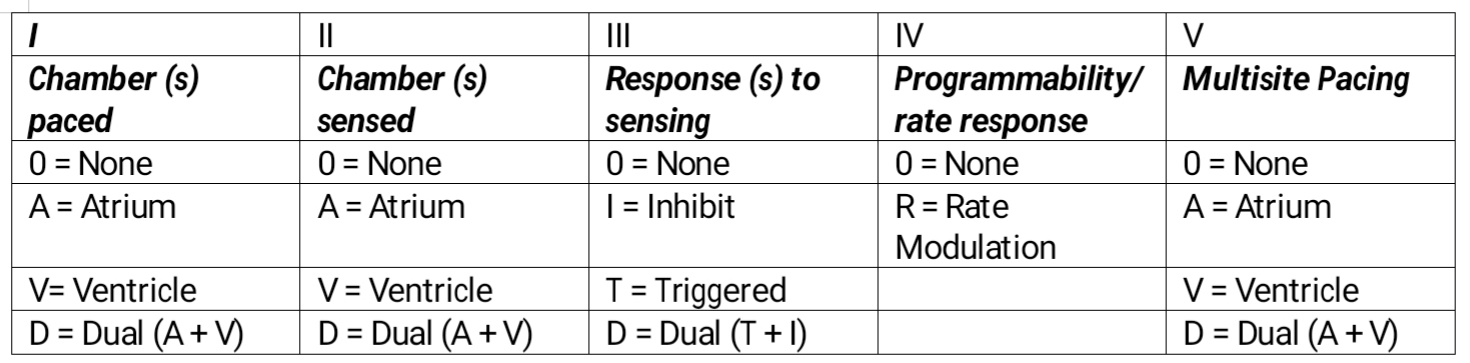
Pacemaker Table. External pacing is the fastest available method to synchronize cardiac rhythm in all the bradyarrhythmias indicated by the American Heart Association. This temporary method is used to maintain cardiac output in all those irreversible conditions where there is a need for a permanent pacemaker or those reversible situations where permanent pacing is contraindicated.
Contributed by M Ellison, MD, FASA
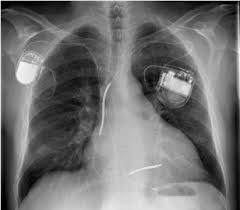
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Carrión-Camacho MR, Marín-León I, Molina-Doñoro JM, González-López JR. Safety of Permanent Pacemaker Implantation: A Prospective Study. Journal of clinical medicine. 2019 Jan 1:8(1):. doi: 10.3390/jcm8010035. Epub 2019 Jan 1 [PubMed PMID: 30609668]
Parkash R, Sapp J, Gardner M, Gray C, Abdelwahab A, Cox J. Use of Administrative Data to Monitor Cardiac Implantable Electronic Device Complications. The Canadian journal of cardiology. 2019 Jan:35(1):100-103. doi: 10.1016/j.cjca.2018.10.018. Epub 2018 Nov 13 [PubMed PMID: 30595171]
Polimenakos AC, Mathis L, Shafer B, Kamath MV. Selective Use of Temporary Epicardial Pacing Leads in Early Infancy Following Cardiac Surgery: Feasibility and Determinants of Clinical Application. Pediatric cardiology. 2019 Mar:40(3):630-637. doi: 10.1007/s00246-018-2037-y. Epub 2018 Dec 18 [PubMed PMID: 30564866]
Level 2 (mid-level) evidenceBob-Manuel T, Nanda A, Latham S, Pour-Ghaz I, Skelton WP 4th, Khouzam RN. Permanent pacemaker insertion in patients with conduction abnormalities post transcatheter aortic valve replacement: a review and proposed guidelines. Annals of translational medicine. 2018 Jan:6(1):11. doi: 10.21037/atm.2017.10.21. Epub [PubMed PMID: 29404357]
Kosztin A, Boros AM, Geller L, Merkely B. Cardiac resynchronisation therapy: current benefits and pitfalls. Kardiologia polska. 2018:76(10):1420-1425. doi: 10.5603/KP.a2018.0160. Epub 2018 Aug 9 [PubMed PMID: 30091132]
Proclemer A, Zecchin M, D'Onofrio A, Boriani G, Facchin D, Rebellato L, Ghidina M, Bianco G, Bernardelli E, Pucher E, Gregori D. [The Pacemaker and Implantable Cardioverter-Defibrillator Registry of the Italian Association of Arrhythmology and Cardiac Pacing - Annual report 2016]. Giornale italiano di cardiologia (2006). 2018 Feb:19(2):119-131. doi: 10.1714/2868.28944. Epub [PubMed PMID: 29531385]
Proclemer A, Zecchin M, D'Onofrio A, Botto GL, Facchin D, Rebellato L, Ghidina M, Bianco G, Bernardelli E, Pucher E, Gregori D. [The Pacemaker and Implantable Cardioverter-Defibrillator Registry of the Italian Association of Arrhythmology and Cardiac Pacing--Annual report 2014]. Giornale italiano di cardiologia (2006). 2016 Feb:17(2):95-107. doi: 10.1714/2174.23494. Epub [PubMed PMID: 27029759]
Samii SM. Indications for pacemakers, implantable cardioverter-defibrillator and cardiac resynchronization devices. The Medical clinics of North America. 2015 Jul:99(4):795-804. doi: 10.1016/j.mcna.2015.02.008. Epub [PubMed PMID: 26042883]
Zartner P. [Antibradycardia therapy : Indication and implementation]. Herzschrittmachertherapie & Elektrophysiologie. 2016 Jun:27(2):88-94. doi: 10.1007/s00399-016-0426-6. Epub 2016 May 24 [PubMed PMID: 27221084]
Poh PG, Liew C, Yeo C, Chong LR, Tan A, Poh A. Cardiovascular implantable electronic devices: a review of the dangers and difficulties in MR scanning and attempts to improve safety. Insights into imaging. 2017 Aug:8(4):405-418. doi: 10.1007/s13244-017-0556-3. Epub 2017 Jun 17 [PubMed PMID: 28624970]