Introduction
Ambulatory electrocardiogram (ECG) monitoring is an invaluable tool to assess and establish a diagnosis of a patient’s symptoms. There are a variety of possible ambulatory ECG monitors to choose from. Holter monitors are used to record 24 to 48 hours of activity. Event monitors can record 2 to 4 hours of activity. Implantable loop recorders can record for up to 3 years. The choice among these technologies is usually based on the suspected monitoring duration that will be required to capture a spontaneous event. Thus, if symptoms occur daily, a Holter monitor may be adequate. If symptoms occur weekly or monthly, an event monitor may be best. If symptoms occur less than monthly or even a few times per year, then an implantable loop recorder is likely the best option. Typical event recorders may not be useful at all if the patient collapses and cannot activate the device. Because of such, a device that can activate on its own and/or has memory to retain information for later download is preferred. This article will cover implantable loop recorders.[1][2][3]
The implantable loop recorder (ILR) is a subcutaneous monitoring device used to monitor electrical activity of the heart over an extended period, compared to the fixed picture of electrical activity that is seen with ECGs.[4]
Indications
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Indications
An implantable loop recorder is most commonly used for the evaluation of recurrent palpitations, syncope of unknown etiology or when other ambulatory monitoring devices of shorter duration are unrevealing.[5][6][7] It may also be useful for the following:
- Identifying asymptomatic occult episodes of atrial fibrillation following a stroke
- Assessing the average heart rate and adequacy of rate control in a patient with atrial fibrillation
- Assessing bradycardic episodes before implanting a permanent pacemaker
- Screening for asymptomatic ventricular premature beats or nonsustained ventricular tachycardia in patients with congenital or acquired cardiac syndromes
- Evaluating prognosis following an acute coronary event
Contraindications
An absolute contraindication to implanting a loop recorder is when there is no indication for its use. Relative contraindications include active infection or a bleeding diathesis which may preclude its implantation for a certain period.
Equipment
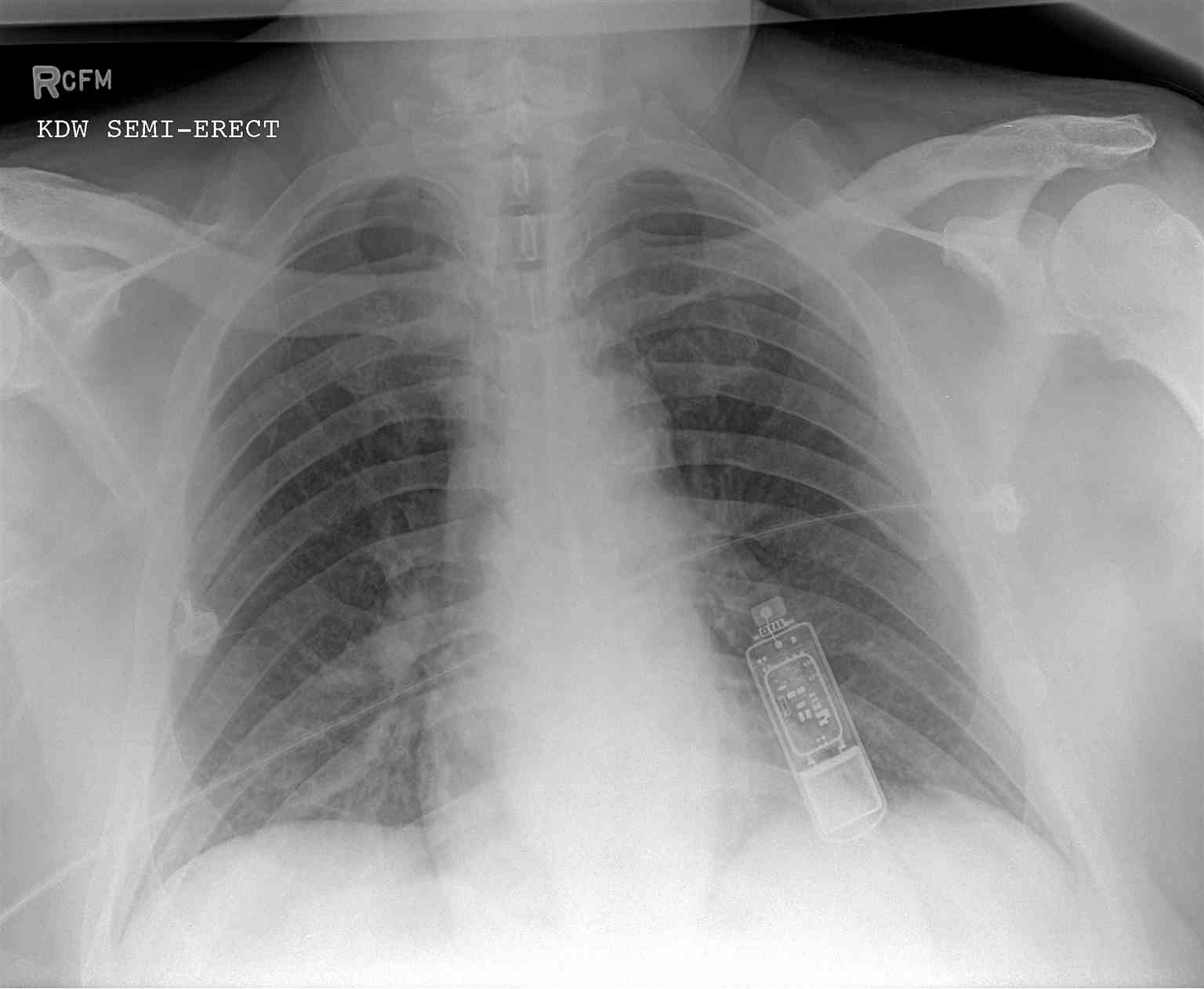
The implantable loop recorder is a small leadless box, about the size of a USB memory stick, with two self-contained electrodes. As stated previously, current implantable loop recorder devices have a battery life of up to 3 years.[8][4]
Technique or Treatment
A small incision is made on the left side at about the level of the second or third rib. A pocket is created under the skin, and the device is inserted in that pocket, and then the incision is closed. The device is usually implanted by an electrophysiologist as an outpatient procedure using local anesthesia. Conscious sedation can be used but is generally not required. Once implanted, the device is activated by passing a magnet over it.
Complications
The most common complication is a pain at the implant site. Risks of the procedure include a local pocket infection that may require removal of the implanted device or a local skin reaction to the device. Poor R-wave sensing is a rare complication that may require moving the device to another location.
Clinical Significance
An implantable loop recorder can store patient activated episodes, automatically activated episodes or a combination of the two. A typical loop recorder report includes information about the captured ECG tracings, the technician’s interpretation of the ECG tracing and any reported symptoms and their respective duration, which can assist the physician in diagnosing the underlying problem.
Implantable loop recorders have the best yield (up to a 75% detection rate for the cause of syncope at 3 years). They do not need to be removed during certain activities such as showering or swimming and may identify significant cardiac rhythm abnormalities when the patient is sleeping. Patients can continue with their normal activity of everyday living and exercise freely. An identification card is usually given to the patient with the make and model of their implantable loop recorder device. This information is valuable should the patient with recurrent symptoms present to the emergency department and need to have their device checked. The main purpose of the device is to record electrical activity and is therefore safe to travel with and it is not affected by other electrical devices. Event recorders are the next most productive and Holter monitors are the least effective unless events occur daily, which is not the case for most patients.
Following the monitoring period, there are three possible combinations of patient symptoms and ECG findings. The first possibility is that the patient had symptoms with corresponding ECG abnormalities, in which case appropriate therapy should be initiated. Possible recommendations include implantation of a permanent pacemaker, implantation of an implantable cardiac defibrillator, or a diagnostic electric study of the heart that may or may not be followed by a therapeutic procedure. If an arrhythmia is detected, such as atrial fibrillation, the patient may need to start a blood thinning medication to decrease the risk of a cerebral vascular accident. The second possibility is that the patient had symptoms without corresponding ECG abnormalities, in which case the diagnosis is unlikely cardiac in nature, and other etiologies for the patient’s symptoms should be investigated. The patient can be referred to other more appropriate specialist if necessary. The third possibility is that the patient had no symptoms and no ECG abnormalities during the monitoring period and a cardiac etiology is unlikely, and no further ECG monitoring is required. If a diagnosis is made or no abnormalities were discovered during the monitoring period, the patient can have the device removed in a similar fashion that it was implanted.
Implantable loop recorders are a safe and effective way to identify arrhythmias and other cardiac abnormalities. It should be considered only after a thorough history and physical examination are performed. Family history and medication use should also be discussed with the patient. Initial imaging should include ECG and echocardiogram which may reveal structural heart disease. Other testing such as a stress test or a tilt table test, may be beneficial if indicated. If the patient continues to have symptoms and all workup is unrevealing, then electrophysiology testing and an implantable loop recorder is the best approach in select patients.[1][5]
Enhancing Healthcare Team Outcomes
Healthcare workers including the nurse practitioner who deal with patients with syncope and arrhythmias should be familiar with the implantable loop recorder. Unlike the traditional holter monitor, the implantable loop recorder is far more efficient and reliable at identifying abnormal rhythms. However, they should be considered only after a thorough history and physical examination are performed. Family history and medication use should also be discussed with the patient. Initial imaging should include ECG and echocardiogram which may reveal structural heart disease. Other testing such as a stress test or a tilt table test, may be beneficial if indicated. If the patient continues to have symptoms and all workup is unrevealing, then electrophysiology testing and an implantable loop recorder is the best approach in select patients.
Media
(Click Image to Enlarge)
References
Arcinas LA, McIntyre WF, Hayes CJ, Ibrahim OA, Baranchuk AM, Seifer CM. Atrial fibrillation in elderly patients with implantable loop recorders for unexplained syncope. Annals of noninvasive electrocardiology : the official journal of the International Society for Holter and Noninvasive Electrocardiology, Inc. 2019 May:24(3):e12630. doi: 10.1111/anec.12630. Epub 2019 Jan 7 [PubMed PMID: 30615233]
Roca-Luque I, Francisco-Pascual J, Oristrell G, Rodríguez-García J, Santos-Ortega A, Martin-Sanchez G, Rivas-Gandara N, Perez-Rodon J, Ferreira-Gonzalez I, García-Dorado D, Moya-Mitjans A. Syncope, conduction disturbance, and negative electrophysiological test: Predictive factors and risk score to predict pacemaker implantation during follow-up. Heart rhythm. 2019 Jun:16(6):905-912. doi: 10.1016/j.hrthm.2018.12.015. Epub 2018 Dec 18 [PubMed PMID: 30576876]
Sakhi R, Theuns DAMJ, Szili-Torok T, Yap SC. Insertable cardiac monitors: current indications and devices. Expert review of medical devices. 2019 Jan:16(1):45-55. doi: 10.1080/17434440.2018.1557046. Epub 2018 Dec 11 [PubMed PMID: 30522350]
Santini M, Santini L, Di Fusco SA. Update on cardiac implantable electronic devices: from the injectable loop recorder to the leadless pacemaker, to the subcutaneous defibrillator. Minerva cardioangiologica. 2018 Dec:66(6):762-769. doi: 10.23736/S0026-4725.18.04693-5. Epub [PubMed PMID: 30468062]
Dwivedi A, Joza J, Malkani K, Mendelson TB, Priori SG, Chinitz LA, Fowler SJ, Cerrone M. Implantable Loop Recorder in Inherited Arrhythmia Diseases: A Critical Tool for Symptom Diagnosis and Advanced Risk Stratification. JACC. Clinical electrophysiology. 2018 Oct:4(10):1372-1374. doi: 10.1016/j.jacep.2018.07.008. Epub [PubMed PMID: 30336885]
Yeung C, Drew D, Hammond S, Hopman WM, Redfearn D, Simpson C, Abdollah H, Baranchuk A. Extended Cardiac Monitoring in Patients With Severe Sleep Apnea and No History of Atrial Fibrillation (The Reveal XT-SA Study). The American journal of cardiology. 2018 Dec 1:122(11):1885-1889. doi: 10.1016/j.amjcard.2018.08.032. Epub 2018 Sep 7 [PubMed PMID: 30274768]
Padmanabhan D, Kancharla K, El-Harasis MA, Isath A, Makkar N, Noseworthy PA, Friedman PA, Cha YM, Kapa S. Diagnostic and therapeutic value of implantable loop recorder: A tertiary care center experience. Pacing and clinical electrophysiology : PACE. 2019 Jan:42(1):38-45. doi: 10.1111/pace.13533. Epub 2018 Dec 4 [PubMed PMID: 30357866]
Kanjwal K, Qadir R, Ruzieh M, Grubb BP. Role of implantable loop recorders in patients with postural orthostatic tachycardia syndrome. Pacing and clinical electrophysiology : PACE. 2018 Sep:41(9):1201-1203. doi: 10.1111/pace.13441. Epub 2018 Jul 26 [PubMed PMID: 29989177]