Introduction
An arterial aneurysm is defined as a permanent localized dilatation of the vessel, enlarging by at least 150% compared to the relatively normal diameter of the adjacent artery.[1] An abdominal aortic aneurysm is an abnormal focal dilation of the abdominal aorta. This life-threatening condition requires monitoring or treatment depending on the size of the aneurysm and associated symptoms. The abdominal aortic aneurysm may be detected incidentally or at the time of rupture.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Risk factors for abdominal aortic aneurysm include atherosclerosis (the most common), smoking, advanced age, male gender, White race, family history of abdominal aortic aneurysm, hypertension, hypercholesterolemia, and prior history of aortic dissection. Other causes include cystic medial necrosis, syphilis, HIV, and connective tissue diseases (Ehlers-Danlos syndrome, Marfan syndrome, and Loeys-Dietz syndrome). Non-White race and diabetes are associated with a reduced risk for abdominal aortic aneurysm. Enlargement of the aneurysm can occur in a step-wise manner, with size remaining stable for some time before experiencing a more rapid enlargement. The enlargement rate for small abdominal aortic aneurysms (3-5 cm) is 0.2 to 0.3 cm/year, whereas it ranges from 0.3 to 0.5 cm/year for those with a diameter greater than 5 cm.[2] The pressure on the aortic wall follows the law of Laplace (wall stress is proportional to the radius of the aneurysm). Accordingly, larger aneurysms are at a higher risk of rupture, and the presence of hypertension also increases this risk.
Epidemiology
Based on autopsy studies, the frequency of these aneurysms varies from 0.5% to 3%. The incidence of abdominal aortic aneurysms increases after 60 and peaks in the seventh and eighth decades of life. White men have the highest risk of developing abdominal aortic aneurysms, whereas they are relatively uncommon in Asian, African American, and Hispanic individuals.[3] Data derived from Lifeline abdominal aortic aneurysm screening and the National Health and Nutrition Examination Survey (NHANES, 2003-2006) database reveal a prevalence of 1.4% in individuals aged 50 to 84, equivalent to 1.1 million abdominal aortic aneurysms studied.[4]
With the increased use of ultrasound, diagnosis of abdominal aortic aneurysms is quite common. They tend to be more common in smokers and older White males. Although autopsy studies may under-represent the incidence of abdominal aortic aneurysm, a study conducted in Malmo, Sweden, revealed a prevalence of 4.3% in men and 2.1% in women as detected by ultrasound.[5]
Pathophysiology
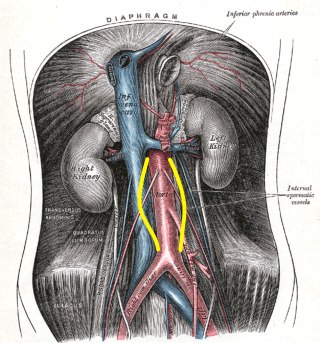
Abdominal aortic aneurysms tend to occur when there is a failure of the structural proteins of the aorta. What causes these proteins to fail is unknown, but the aortic wall gradually weakens. The decrease in structural proteins of the aortic wall, such as elastin and collagen, has been identified.[6][7][8] The aortic wall is made of collagen lamellar units. The number of lamellar units is lower in the infrarenal aorta than in the thoracic aorta.[8][9][10] This is believed to contribute to the increased incidence of aneurysmal formation in the infrarenal aorta. A chronic inflammatory process has been identified in the wall of the aorta, but its cause remains unclear.[11] Other factors that may play a role in the development of these aneurysms include genetics, marked inflammation, and proteolytic degradation of the connective tissue in the aortic wall.[12][13][14] See Image. Abdominal Aortic Aneurysm Illustration.
Histopathology
Autopsy studies of abdominal aortic aneurysms usually show significant degeneration of the media and typically reveal a state of chronic inflammation with an infiltrate of neutrophils, macrophages, and lymphocytes. The media is often thin, and there is evidence of degeneration of the connective tissue.
History and Physical
Most abdominal aortic aneurysms are incidentally identified during examinations for other unrelated pathologies, and most individuals are asymptomatic. Palpation of the abdomen usually reveals a non-tender, pulsatile abdominal mass. Enlarging aneurysms can cause symptoms such as abdominal, flank, or back pain. The compression of adjacent viscera can cause gastrointestinal or renal manifestations.
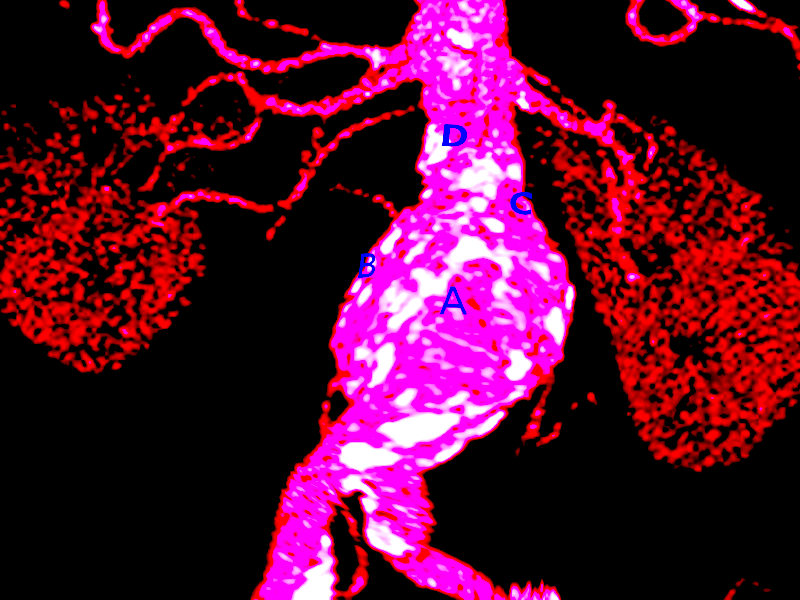
The rupture of an abdominal aortic aneurysm is life-threatening. However, the presentation of patients with this type of ruptured aneurysm can vary from subtle to quite dramatic. See Images. Abdominal Aortic Aneurysm Rupture and Ruptured Aortic Aneurysm. Most patients may present in shock, often exhibiting diffuse abdominal pain and distension. Patients with a ruptured abdominal aortic aneurysm often die even before reaching the hospital. The patient may have tenderness over the aneurysm or demonstrate signs of embolization. If the aneurysm ruptures into adjacent viscera or vessels, presenting findings may include gastrointestinal bleeding or congestive heart failure due to the aortocaval fistula. A physical examination should also include an assessment for other associated aneurysms, the most common being an iliac artery aneurysm. Peripheral aneurysms are also associated with approximately 5% of patients, with popliteal artery aneurysms being the most common.
Evaluation
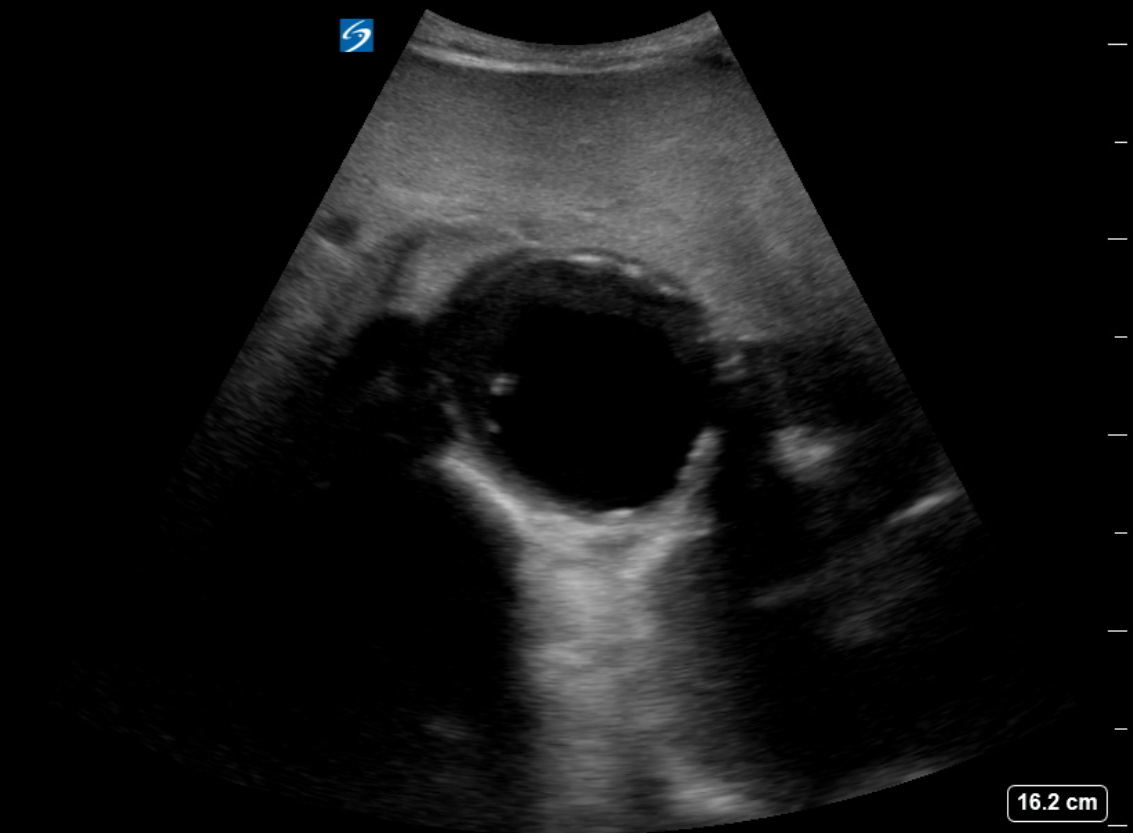
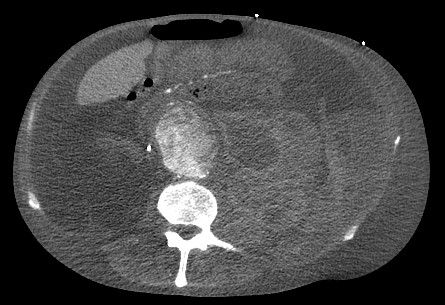
The diagnosis of an abdominal aortic aneurysm is usually made using ultrasound (see Images. Abdominal Aortic Aneurysm Ultrasound and AAA). However, a computed tomography (CT) scan remains necessary to determine the exact location, size, and involvement of other vessels and is the preferred imaging modality for symptomatic patients. The ultrasound can be used for screening purposes but is less accurate for aneurysms located above the renal arteries due to the presence of overlying air-containing lungs and viscera. CT angiography requires the use of ionizing radiation and intravenous contrast. Magnetic resonance angiography can be used to delineate the anatomy and does not require ionizing radiation.
Most of these aneurysms are located below the origin of the renal arteries and may be classified as saccular (localized) or fusiform (circumferential). More than 90% of abdominal aortic aneurysms are fusiform. Intense inflammation, a thickened peel, and adhesions to adjacent structures characterize an inflammatory abdominal aortic aneurysm. Angiography is now rarely performed for diagnostic purposes due to the superior image quality achieved with CT scans.[15]
Magnetic resonance angiography is an option for patients with allergies to contrast media. An echocardiogram is recommended as many patients also tend to have associated heart disease.
All patients require routine blood work, including a cross-match if surgery is necessary. Patients with comorbidities such as diabetes, chronic obstructive pulmonary disease, or heart disease should be diagnosed by the relevant specialist and cleared for surgery.
Treatment / Management
The treatment of unruptured abdominal aortic aneurysms is recommended when the aneurysm diameter reaches 5.5 cm in men[16], shows a rapid enlargement of greater than 0.5 cm over 6 months, or if it becomes symptomatic. Thus, according to recent guidelines from the European Society for Vascular Surgery (ESVS), abdominal aortic aneurysm repair is recommended if the aneurysm is symptomatic and greater than 4 cm, and has increased in size by greater than 1 cm/year, as measured by the inner-to-inner maximum anterior-posterior aortic diameter on ultrasound.[16] For women, the ESVS recommends elective repair for asymptomatic abdominal aortic aneurysm when the diameter exceeds 5.0 cm, although this recommendation is based on weak evidence.[16](A1)
Open surgical repair using the transabdominal or retroperitoneal approach has been the gold standard. Endovascular repair from a femoral arterial approach is now applied for most repairs, especially in older and higher-risk patients. Endovascular therapy is recommended for patients who are not suitable candidates for open surgery. This includes patients with severe heart disease or other comorbidities that preclude open repair. A ruptured abdominal aortic aneurysm warrants emergency repair. If the anatomy is suitable, the endovascular approach for ruptured abdominal aortic aneurysm has shown superior results and survival rates compared to open repair, but the mortality rates remain high. The risk of surgery is influenced by the patient's age, the presence of renal failure, and the status of the cardiopulmonary system.[17][18]
Data show that endovascular repair has no long-term differences in outcomes for unruptured abdominal aortic aneurysms compared to open repair. However, data indicate that expansion of the neck of the aorta continues despite endovascular therapy, which is concerning. The need to take beta blockers cannot be understated in these patients. For many decades, open repair has been the gold standard for abdominal aortic aneurysm repair, which involves a long midline incision followed by replacing the diseased aorta with a graft. Postoperatively, these patients need close monitoring in the intensive care unit for 24 to 48 hours.
All patients with small abdominal aortic aneurysms who do not undergo repair need periodic follow-ups with an ultrasound every 6 to 12 months to ensure that the aneurysm is not expanding.[19]
Traditionally, the anatomic eligibility for endovascular aortic aneurysm repair was mainly based on 3 major indexes—the proximal aortic neck, common iliac arteries, and external iliac and common femoral arteries. The mentioned index areas characterize the proximal and distal landing zones. An endovascular approach is not indicated in the proximal aortic neck of less than 15 mm.[20] However, the endovascular approach to managing complex aortic aneurysms has been widely approved. The endovascular approach might be utilized in managing thoracoabdominal, pararenal, and juxtarenal aneurysms.[21](A1)
Fenestrated and branched endovascular aneurysm repair application in managing aortic aneurysms elucidated obvious advantages, including fewer perioperative complications, specifically significant in high-volume vascular centers.
Stent graft selection and the durability characteristics of the stent determine the long-term efficacy of the fenestrated and branched endovascular aneurysm repair procedures. Fenestrated and branched endovascular aneurysm repair procedures are frequently reported together, and the separate effects of the procedures have not been discussed thoroughly. However, the selection of either balloon-expandable or self-expandable stent graft is mainly affected by the surgeon's preferences.[22]
Institutional algorithms for juxtarenal aortic aneurysm repair have addressed the factors affecting decision-making for the fenestrated and branched endovascular aneurysm repair procedures. However, there is a lack of absolute indications or contraindications criteria in the patient selection.[23] Accordingly, high surgical risk and appropriate morphology would mainly affect the decision-making towards the fenestrated endovascular repair. The aneurysm morphology characteristics to be reviewed include the localization of visceral and renal arteries, number of arteries, iliac access, and shaggy aorta.[23]
Considering the complications with fenestrated endovascular graft and fenestration stent repair, in-stent stenosis of bare metal renal stents is considered the most common indication for secondary intervention. The low rate of type IA endoleak, sac enlargement, and device migration favors fenestrated endovascular repair in patients with juxtarenal abdominal aortic aneurysms.[24](B2)
SVS Guidelines on Management of abdominal aortic aneurysms
Updated guidelines on the care of patients with abdominal aortic aneurysms were issued by the Society for Vascular Surgery (SVS) in 2020. These guidelines include the following:
- Yearly surveillance imaging in patients with an abdominal aortic aneurysm diameter ranging from 4.0 to 4.9 cm.
- Assessment of distal leg pulses at each clinic visit.
- For unruptured abdominal aortic aneurysm, endovascular aneurysm repair is recommended.
- The endovascular procedure should only be performed in a hospital that conducts at least 10 cases yearly and has a conversion rate to open repair of less than 2%.
- Elective abdominal aortic aneurysm open surgery should be performed in hospitals with a mortality of less than 5% and at least 10 open cases conducted annually.
- For a ruptured abdominal aortic aneurysm, a facility with a door-to-intervention time of less than 90 minutes is preferred.
- Recommend treatment of types I and III endoleaks and type II endoleaks with aneurysm expansion.
- Antibiotic prophylaxis is not recommended before respiratory tract, genitourinary, dermatologic, gastrointestinal, or orthopedic procedures unless there is a potential for infection in an immunocompromised patient.
- Color duplex ultrasonography should be used for postoperative surveillance after endovascular surgery.
- A preoperative 12-lead electrocardiogram is recommended for all patients undergoing endovascular aneurysm repair or open surgical repair within 4 weeks of the elective surgery.
- If the patient has recently undergone placement of a drug-eluting stent, open aneurysm surgery should be delayed for at least 6 months, or endovascular surgery can be performed while the patient is still on dual antiplatelet therapy.
- Transfuse blood perioperatively only if the hemoglobin level is less than 7 g/dL.
- Elective repair should be recommended for low-risk patients when the abdominal aortic aneurysm reaches 5.5 cm in diameter.
Differential Diagnosis
The differential diagnosis for abdominal aortic aneurysm includes mesenteric ischemia, peptic ulcer disease, diverticulitis, pyelonephritis, myocardial infarction, and ureteric colic.[26]
Prognosis
Once an abdominal aortic aneurysm ruptures, the prognosis is grim. More than 50% of patients die before they reach the emergency room. Those who survive have very high morbidity. Predictors of mortality include preoperative cardiac arrest, age greater than 80, female gender, massive blood loss, and ongoing transfusion.[27] In a patient with a ruptured abdominal aortic aneurysm, the one factor determining mortality is the ability to achieve proximal control. For those undergoing elective repair, the prognosis is good to excellent. However, long-term survival depends on other comorbidities such as chronic obstructive pulmonary disease, heart disease, and peripheral vascular disease. An estimated 70% of patients survive for 5 years after repair.
Complications
The complications associated with abdominal aortic aneurysm include bleeding, limb ischemia, delayed rupture secondary to endoleak, abdominal compartment syndrome, myocardial infarction, pneumonia, graft infection, colon ischemia, renal failure, bowel obstruction, blue toe syndrome, amputation, impotence, lymphocele, and death.
Postoperative and Rehabilitation Care
After repair, it is essential that the patient discontinue smoking, eat a healthy diet, and maintain a healthy weight. Physical or occupational therapy may be necessary. Follow-up CT imaging 5 years after open repair management is recommended to exclude late aortic dilation or pseudoaneurysm.
Consultations
Once an abdominal aortic aneurysm is diagnosed, the patient should be referred to a vascular surgeon. Surveillance imaging at 12-month intervals is recommended for patients with an abdominal aortic aneurysm diameter ranging from 4.0 to 4.9 cm.[28] As indicated, cardiology and pulmonary evaluations are recommended to ensure that the patient is fit for surgery.
Deterrence and Patient Education
Many patients with abdominal aortic aneurysms can lead healthy, symptom-free lives. The decision to undergo surgery involves weighing the risk of aneurysmal rupture against the risks and benefits associated with the surgical procedure. Although the size of the aneurysm and its enlargement rate are included in some general guidelines, each treatment decision should be made individually. Clinicians should discuss the surgical risks with their patients so they can make informed decisions.
Pearls and Other Issues
Key insights and recommendations concerning the management of abdominal aortic aneurysms are provided below.
- Patients with abdominal aortic aneurysms should quit smoking to reduce the risk of enlargement.
- Assessment of medical optimization of hypertension, hyperlipidemia, diabetes, and other atherosclerotic should be performed.
- Moderate exercise does not cause a rupture of abdominal aortic aneurysm expansion.[29]
- The SVS guidelines recommend ultrasound screening for all men and women aged 65 or older who have smoked or have a family history of abdominal aortic aneurysm.[20]
- Surveillance guidelines for abdominal aortic aneurysm per the SVS using duplex ultrasonography are the following:
- 3-year intervals for patients with an abdominal aortic aneurysm diameter ranging between 3.0 and 3.9 cm
- 12-month intervals for patients with an abdominal aortic aneurysm diameter ranging from 4.0 to 4.9 cm
- 6-month intervals for patients with an abdominal aortic aneurysm diameter ranging between 5.0 and 5.4 cm
- Patients with an initial aortic diameter <3 cm have a low risk of rupture. At this time, there are no recommendations for surveillance; however, it should be noted that gradual expansion has been observed in these patients over time.
- Patients presenting with symptomatic abdominal aortic aneurysm should be considered for urgent repair.
- Asymptomatic patients with abdominal aortic aneurysm demonstrating an aortic diameter >5.4 cm or those with the rapid expansion of small abdominal aortic aneurysm should be evaluated for repair.
- The objective of abdominal aortic aneurysm repair is to increase survival rates. Consideration of the quality of life after the repair is essential, particularly in those with a shortened life expectancy due to medical comorbidities or cancer.
- Endovascular repair may offer fewer complications and a better quality of life in those at high risk for open repair up to 1-year post-intervention.[30]
The factors that increase the operative risk for abdominal aortic aneurysm repair include severe heart disease, severe chronic obstructive pulmonary disease, poor renal function, and comorbidities such as stroke, diabetes, hypertension, and advanced age, which can increase the risk of open surgical procedures. If the aortic anatomy permits, these individuals should be considered for endovascular aneurysm stenting.
Infrarenal Aortic Aneurysm Repair
Consideration for repair is appropriate for all symptomatic aneurysms. Aortic anatomy and device availability can dictate the approach. Open aneurysm repair had been the gold standard but carried increased risk and potential complications, which may be acceptable in a younger, good surgical-risk patient. This is still a more durable procedure. Endovascular repair is now an established technique for repairing an abdominal aortic aneurysm. This minimally invasive procedure can also be offered but has better outcomes and durability when the anatomy meets device-specific recommendations. This is the preferred approach in rupture cases and patients with multiple risk factors or a shortened life expectancy. Intervention or surgical treatment risks versus benefits of repair in patients at an increased risk for open surgery should be considered, and no intervention may be appropriate in some cases.
Patients should be well-informed regarding their options, risks of repair, and potential postoperative complications. Endovascular repair requires lifelong follow-up with imaging as early or late endoleaks may develop, causing aortic sac pressurization and rupture. Secondary interventions, the majority of which are minimally invasive, may be necessary. Still, there is a small chance that an open conversation with the stent-graft removal may be required when these secondary endovascular interventions fail.
Enhancing Healthcare Team Outcomes
Infrarenal abdominal aortic aneurysms are the most common aneurysms of the aorta. Screening ultrasound has helped in the detection of abdominal aortic aneurysms and allows for surveillance in asymptomatic patients with a diameter of less than 5 cm. In females, the repair should be considered at 5 cm, and in males, at 5.5 cm. If rapid enlargement is demonstrated (>5 mm over 6 months), repair should be considered. Educating first responders, including the nurse practitioner, triage nurse, primary care physicians, physician assistants, and emergency department physicians, can facilitate diagnosis and reduce delays in treatment.
An interprofessional team approach involving emergency nurses, emergency physicians, intensivists, radiologists, and a vascular surgeon will facilitate rapid evaluation and treatment and improve outcomes. The vast majority of patients with abdominal aortic aneurysm initially present to the emergency department with vague abdominal pain or a pulsatile mass. Thus, the triage nurse must be familiar with the presentation of an abdominal aortic aneurysm and initiate a rapid admission with direct communication to the emergency department physician and the rest of the interprofessional team about the patient. Once admitted, if stable, these patients require an urgent ultrasound; therefore, the radiologist should be notified. If the patient is unstable, the nurse should obtain vital signs, attach monitoring equipment, and assist with resuscitation if the patient is hemodynamically unstable.
Referral to a vascular center capable of providing a standard-of-care management is appropriate. Once the decision for repair has been made, conducting a cardiology workup, obtaining clearance, and optimizing other medical comorbidities can improve outcomes. If the aneurysm is small, the interprofessional team should educate the patient and family about the importance of blood pressure control, a healthy diet, regular exercise, smoking cessation, and follow-up appointment adherence..
During postoperative care, the nurse must be familiar with potential complications of the surgery and notify the interprofessional team if the patient has abdominal or back pain, wound discharge, fever, oliguria, or hypotension. The nurse should also ensure the patient has prophylaxis to prevent deep vein thrombosis. The respiratory therapist should encourage deep breathing and coughing, and the physical therapist should encourage ambulation. The nurse should also auscultate for bowel sounds and convey the results to the interprofessional team to initiate feeding. Before discharge, the pharmacist and nurse should educate the patient on the importance of medication compliance, blood pressure control, and tobacco avoidance. The nurse should also ensure that the appropriate consulting physician, dietitian, or social workers have seen the patient and that the surgeon has been notified before discharge. Open communication among the interprofessional team is vital to ensure good outcomes.
Outcomes
For elective abdominal aortic aneurysm repair, the outcomes are good, with minimal morbidity. However, if a rupture has occurred, the mortality rates can exceed 50%. Current guidelines suggest that patients with abdominal aortic aneurysm should undergo surgery in hospitals with an interprofessional team approach to dealing with this pathology. To improve outcomes, patients must stop smoking, maintain a healthy body weight, control their blood pressure, and remain compliant with medications.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Video to Play)
AAA. Large abdominal aortic aneurysm (AAA) shown with vertebral bone shadow and intramural thrombus.
Contributed by Meghan Herbst, MD
References
Johnston KW, Rutherford RB, Tilson MD, Shah DM, Hollier L, Stanley JC. Suggested standards for reporting on arterial aneurysms. Subcommittee on Reporting Standards for Arterial Aneurysms, Ad Hoc Committee on Reporting Standards, Society for Vascular Surgery and North American Chapter, International Society for Cardiovascular Surgery. Journal of vascular surgery. 1991 Mar:13(3):452-8 [PubMed PMID: 1999868]
Level 1 (high-level) evidencePowell JT, Sweeting MJ, Brown LC, Gotensparre SM, Fowkes FG, Thompson SG. Systematic review and meta-analysis of growth rates of small abdominal aortic aneurysms. The British journal of surgery. 2011 May:98(5):609-18. doi: 10.1002/bjs.7465. Epub 2011 Mar 17 [PubMed PMID: 21412998]
Level 1 (high-level) evidenceZommorodi S, Leander K, Roy J, Steuer J, Hultgren R. Understanding abdominal aortic aneurysm epidemiology: socioeconomic position affects outcome. Journal of epidemiology and community health. 2018 Oct:72(10):904-910. doi: 10.1136/jech-2018-210644. Epub 2018 Jul 2 [PubMed PMID: 29967003]
Level 3 (low-level) evidenceKent KC, Zwolak RM, Egorova NN, Riles TS, Manganaro A, Moskowitz AJ, Gelijns AC, Greco G. Analysis of risk factors for abdominal aortic aneurysm in a cohort of more than 3 million individuals. Journal of vascular surgery. 2010 Sep:52(3):539-48. doi: 10.1016/j.jvs.2010.05.090. Epub 2010 Jul 13 [PubMed PMID: 20630687]
Level 2 (mid-level) evidenceBengtsson H, Bergqvist D, Ekberg O, Janzon L. A population based screening of abdominal aortic aneurysms (AAA). European journal of vascular surgery. 1991 Feb:5(1):53-7 [PubMed PMID: 2009986]
Level 2 (mid-level) evidenceXu C, Zarins CK, Glagov S. Aneurysmal and occlusive atherosclerosis of the human abdominal aorta. Journal of vascular surgery. 2001 Jan:33(1):91-6 [PubMed PMID: 11137928]
Busuttil RW, Abou-Zamzam AM, Machleder HI. Collagenase activity of the human aorta. A comparison of patients with and without abdominal aortic aneurysms. Archives of surgery (Chicago, Ill. : 1960). 1980 Nov:115(11):1373-8 [PubMed PMID: 6254469]
Busuttil RW, Rinderbriecht H, Flesher A, Carmack C. Elastase activity: the role of elastase in aortic aneurysm formation. The Journal of surgical research. 1982 Mar:32(3):214-7 [PubMed PMID: 6917898]
Dobrin PB, Baumgartner N, Anidjar S, Chejfec G, Mrkvicka R. Inflammatory aspects of experimental aneurysms. Effect of methylprednisolone and cyclosporine. Annals of the New York Academy of Sciences. 1996 Nov 18:800():74-88 [PubMed PMID: 8958984]
Level 3 (low-level) evidenceCohen JR, Mandell C, Chang JB, Wise L. Elastin metabolism of the infrarenal aorta. Journal of vascular surgery. 1988 Feb:7(2):210-4 [PubMed PMID: 3123716]
Parry DJ, Al-Barjas HS, Chappell L, Rashid ST, Ariëns RA, Scott DJ. Markers of inflammation in men with small abdominal aortic aneurysm. Journal of vascular surgery. 2010 Jul:52(1):145-51. doi: 10.1016/j.jvs.2010.02.279. Epub [PubMed PMID: 20620767]
Level 2 (mid-level) evidenceJiang H, Sasaki T, Jin E, Kuzuya M, Cheng XW. Inflammatory Cells and Proteases in Abdominal Aortic Aneurysm and its Complications. Current drug targets. 2018:19(11):1289-1296. doi: 10.2174/1389450119666180531103458. Epub [PubMed PMID: 29848273]
Majumder PP, St Jean PL, Ferrell RE, Webster MW, Steed DL. On the inheritance of abdominal aortic aneurysm. American journal of human genetics. 1991 Jan:48(1):164-70 [PubMed PMID: 1985458]
Tilson MD, Seashore MR. Human genetics of the abdominal aortic aneurysm. Surgery, gynecology & obstetrics. 1984 Feb:158(2):129-32 [PubMed PMID: 6695305]
Gibbons RC, Singh G, Donuru A, Young M. Abdominal Aortic Aneurysm Imaging. StatPearls. 2024 Jan:(): [PubMed PMID: 29261904]
Wanhainen A, Verzini F, Van Herzeele I, Allaire E, Bown M, Cohnert T, Dick F, van Herwaarden J, Karkos C, Koelemay M, Kölbel T, Loftus I, Mani K, Melissano G, Powell J, Szeberin Z, Esvs Guidelines Committee, de Borst GJ, Chakfe N, Debus S, Hinchliffe R, Kakkos S, Koncar I, Kolh P, Lindholt JS, de Vega M, Vermassen F, Document Reviewers, Björck M, Cheng S, Dalman R, Davidovic L, Donas K, Earnshaw J, Eckstein HH, Golledge J, Haulon S, Mastracci T, Naylor R, Ricco JB, Verhagen H. Editor's Choice - European Society for Vascular Surgery (ESVS) 2019 Clinical Practice Guidelines on the Management of Abdominal Aorto-iliac Artery Aneurysms. European journal of vascular and endovascular surgery : the official journal of the European Society for Vascular Surgery. 2019 Jan:57(1):8-93. doi: 10.1016/j.ejvs.2018.09.020. Epub 2018 Dec 5 [PubMed PMID: 30528142]
Jonker LT, de Niet A, Reijnen MMPJ, Tielliu IFJ, Zeebregts CJ. Mid- and Long-Term Outcome of Currently Available Endografts for the Treatment of Infrarenal Abdominal Aortic Aneurysm. Surgical technology international. 2018 Nov 11:33():239-250 [PubMed PMID: 30117134]
Wang LJ, Prabhakar AM, Kwolek CJ. Current status of the treatment of infrarenal abdominal aortic aneurysms. Cardiovascular diagnosis and therapy. 2018 Apr:8(Suppl 1):S191-S199. doi: 10.21037/cdt.2017.10.01. Epub [PubMed PMID: 29850431]
Amin S, Schnabel J, Eldergash O, Chavan A. [Endovascular aneurysm repair (EVAR) : Complication management]. Der Radiologe. 2018 Sep:58(9):841-849. doi: 10.1007/s00117-018-0437-x. Epub [PubMed PMID: 30083939]
Calero A, Illig KA. Overview of aortic aneurysm management in the endovascular era. Seminars in vascular surgery. 2016 Mar:29(1-2):3-17. doi: 10.1053/j.semvascsurg.2016.07.003. Epub 2016 Jul 15 [PubMed PMID: 27823587]
Level 3 (low-level) evidenceMezzetto L, Scorsone L, Silingardi R, Gennai S, Piffaretti G, Mantovani A, Bush RL, Haulon S, Veraldi GF. Bridging Stents in Fenestrated and Branched Endovascular Aneurysm Repair: A Systematic REVIEW. Annals of vascular surgery. 2021 May:73():454-462. doi: 10.1016/j.avsg.2020.10.052. Epub 2021 Jan 5 [PubMed PMID: 33359330]
Level 1 (high-level) evidenceTenorio ER, Oderich GS, Kölbel T, Gargiulo M, Timaran CH, Bertoglio L, Modarai B, Jama K, Eleshra A, Lima GBB, Scott C, Chiesa R, Jakimowicz T, Trans-Atlantic Aortic Research Consortium. Outcomes of off-the-shelf multibranched stent grafts with intentional occlusion of directional branches using endovascular plugs during endovascular repair of complex aortic aneurysms. Journal of vascular surgery. 2022 Apr:75(4):1142-1150.e4. doi: 10.1016/j.jvs.2021.09.050. Epub 2021 Nov 5 [PubMed PMID: 34748899]
Soler R, Bartoli MA, Faries C, Mancini J, Sarlon-Bartoli G, Haulon S, Magnan PE. Fenestrated endovascular aneurysm repair and open surgical repair for the treatment of juxtarenal aortic aneurysms. Journal of vascular surgery. 2019 Sep:70(3):683-690. doi: 10.1016/j.jvs.2018.11.041. Epub 2019 Mar 6 [PubMed PMID: 30850294]
Oderich GS, Farber MA, Schneider D, Makaroun M, Sanchez LA, Schanzer A, Beck AW, Starnes BW, Fillinger M, Tenorio ER, Chen M, Zhou Q, Zenith Fenestrated Study Investigators. Final 5-year results of the United States Zenith Fenestrated prospective multicenter study for juxtarenal abdominal aortic aneurysms. Journal of vascular surgery. 2021 Apr:73(4):1128-1138.e2. doi: 10.1016/j.jvs.2020.08.128. Epub 2020 Sep 3 [PubMed PMID: 32891806]
Level 2 (mid-level) evidenceEldrup-Jorgensen J, Kraiss LW, Chaikof EL, Neal D, Forbes TL. Vascular Quality Initiative assessment of compliance with Society for Vascular Surgery clinical practice guidelines on the care of patients with abdominal aortic aneurysm. Journal of vascular surgery. 2020 Sep:72(3):874-885. doi: 10.1016/j.jvs.2019.10.097. Epub 2020 Jan 20 [PubMed PMID: 31973949]
Level 2 (mid-level) evidenceAzhar B, Patel SR, Holt PJ, Hinchliffe RJ, Thompson MM, Karthikesalingam A. Misdiagnosis of ruptured abdominal aortic aneurysm: systematic review and meta-analysis. Journal of endovascular therapy : an official journal of the International Society of Endovascular Specialists. 2014 Aug:21(4):568-75. doi: 10.1583/13-4626MR.1. Epub [PubMed PMID: 25101588]
Level 1 (high-level) evidenceJohansen K, Kohler TR, Nicholls SC, Zierler RE, Clowes AW, Kazmers A. Ruptured abdominal aortic aneurysm: the Harborview experience. Journal of vascular surgery. 1991 Feb:13(2):240-5; discussion 245-7 [PubMed PMID: 1990165]
Chaikof EL, Dalman RL, Eskandari MK, Jackson BM, Lee WA, Mansour MA, Mastracci TM, Mell M, Murad MH, Nguyen LL, Oderich GS, Patel MS, Schermerhorn ML, Starnes BW. The Society for Vascular Surgery practice guidelines on the care of patients with an abdominal aortic aneurysm. Journal of vascular surgery. 2018 Jan:67(1):2-77.e2. doi: 10.1016/j.jvs.2017.10.044. Epub [PubMed PMID: 29268916]
Level 1 (high-level) evidenceMyers J, McElrath M, Jaffe A, Smith K, Fonda H, Vu A, Hill B, Dalman R. A randomized trial of exercise training in abdominal aortic aneurysm disease. Medicine and science in sports and exercise. 2014 Jan:46(1):2-9. doi: 10.1249/MSS.0b013e3182a088b8. Epub [PubMed PMID: 23793234]
Level 1 (high-level) evidenceKayssi A, DeBord Smith A, Roche-Nagle G, Nguyen LL. Health-related quality-of-life outcomes after open versus endovascular abdominal aortic aneurysm repair. Journal of vascular surgery. 2015 Aug:62(2):491-8. doi: 10.1016/j.jvs.2015.05.032. Epub [PubMed PMID: 26211382]
Level 2 (mid-level) evidence