Introduction
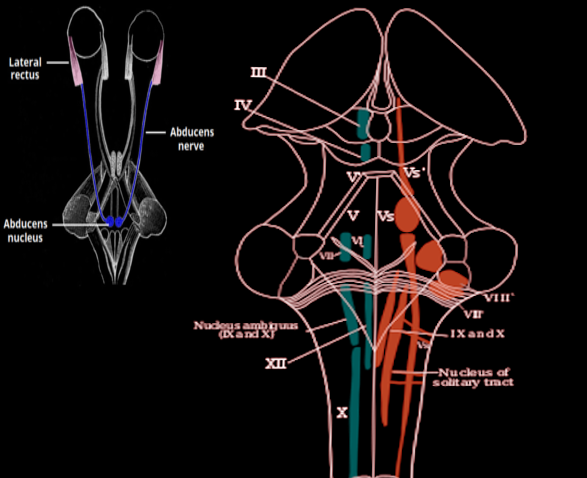
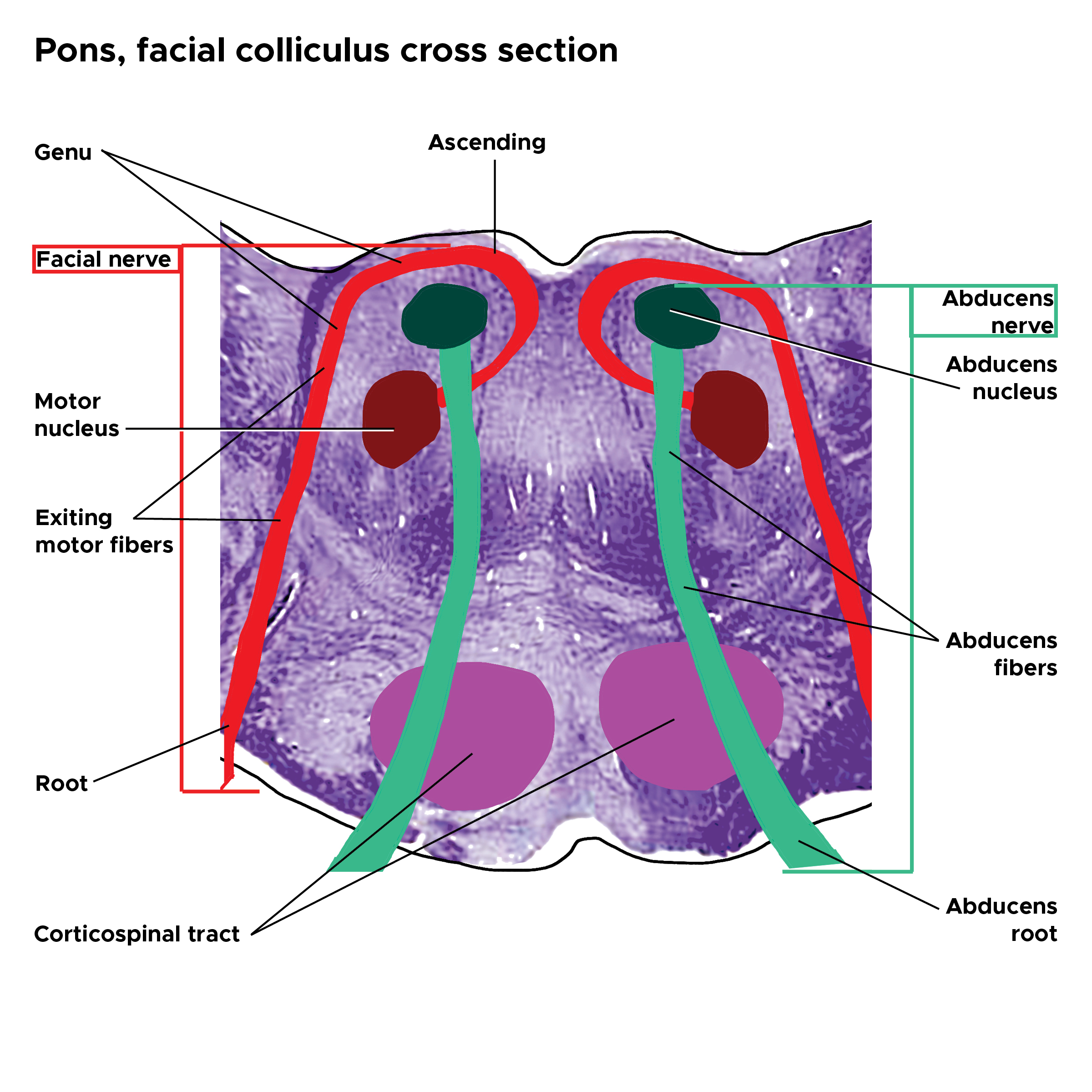
The abducens nuclei appear as paired nuclei, located within the pons at the pontomedullary junction of the brainstem, comprised primarily of motor neurons and interneurons.[1][2] Neurons from the abducens nuclei provide innervation to the lateral rectus muscles and allow for conjugate horizontal gaze by sending signals to the contralateral oculomotor nuclei that innervate the medial rectus muscles.[3] See Image. Pons Facial Colliculus Cross Section.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The paired abducens nuclei are in the medial and dorsal brainstem within the pons at the level of the pontomedullary junction, immediately lateral to the medial longitudinal fasciculus.[4][2] The nuclei are positioned beneath the floor of the fourth ventricle and separated from it by the facial nerve genu, which curves over their dorsal and lateral surfaces. About 70% of the neurons arising from each abducens nucleus are motor neurons that form the abducens nerve fascicles and innervate the ipsilateral lateral rectus muscle. Approximately 30% are internuclear neurons that are involved in the control of the conjugate gaze. A small percentage of neurons project to the cerebellar flocculus, which functions in gaze holding.[4] See Image. Abducens Nucleus.
Embryology
As early as 20 weeks of gestation, the abducens nucleus is identified as a mass of cells located lateral to the facial nerve genu and medial to the medial vestibular nucleus in an area that later becomes the mature pons.[5] The nucleus enlarges more quickly toward the end of gestation between 20 and 43 weeks in the rostrocaudal axis. Its composition is a heterogeneous group of motor neurons and interneurons that this activity describes in detail below. There is a hypothesis that during development, multiple aberrant abducens nerve roots branch out from the nucleus and eventually undergo resorption; therefore, failure to resorb these roots may lead to the development of replicated and/or branched nerves.[6]
Blood Supply and Lymphatics
The blood supply of the abducens nucleus is from the paramedian branches of the basilar artery.[7] Disruption of blood supply from the basilar artery may cause damage to the abducens nucleus along with surrounding cranial nerve nuclei and associated structures.
Nerves
The abducens nucleus consists of motor neurons, interneurons, and a small percentage of neurons projecting to the cerebellar flocculus. Signaling pathways through the nucleus allow for gaze holding and conjugate horizontal gaze during the vestibulo-ocular reflex and for generating saccades. Motor nerve fibers course ventrally through the pons after exiting the abducens nucleus and forming the abducens nerve fascicle.[1] The fibers then exit the brainstem near the midline to form the abducens nerve, emerging from the horizontal sulcus between the pons and medulla, just lateral to the bundles of the corticospinal tract. The abducens nerve fibers then course rostrally along the surface of the clivus within the subarachnoid space anterior to the basilar pons, pass under the petroclival ligament through the Dorello canal, and enter the cavernous sinus. They then pass through the cavernous sinus in close association with the internal carotid artery and penetrate the orbit via the superior orbital fissure within the annulus of Zinn to innervate the ipsilateral lateral rectus muscle.[2][1]
The abducens nucleus plays a significant role in coordinating the conjugate gaze and the generation of rapid saccades conjugate eye movements that allow the center of gaze to shift from 1 part of the visual field to another.[8] Cerebral control of saccades comes from the parietal eye fields and the frontal eye fields, which transmit signals to the superior colliculus.[9] The superior colliculus then projects to the pons' paramedian pontine reticular formation (PPRF), also known as the horizontal gaze center. The PPRF transmits signals to the ipsilateral abducens nucleus that, in turn, sends the signals via internuclear neurons that exit the abducens nucleus and ascend in the contralateral medial longitudinal fasciculus. These then synapse with neurons in the medial rectus subnucleus of the oculomotor nucleus to innervate the medial rectus muscle. This pathway produces equal innervation of the horizontal yoke muscles, the ipsilateral lateral rectus, and the contralateral medial rectus to maintain conjugate gaze via coordinated activity. This coordination of input allows for conjugate horizontal gaze during saccades via the parietal eye fields and frontal eye fields, as well as during voluntary eye movements.
Different afferent inputs control the twitch and non-twitch muscle fibers of the lateral rectus muscle.[4] Twitch motoneurons in the abducens nucleus receive premotor inputs from the burst neurons in the PPRF and the vestibular nuclei, allowing for the generation of eye movements. The non-twitch motoneurons are involved in gaze holding and receive eye position information from the nucleus prepositus hypoglossi (NPH), which lies on the floor of the fourth ventricle. During the horizontal vestibulo-ocular reflex, axons of second-order neurons in the medial vestibular nuclei (MVN) transmit velocity commands to excite the contralateral abducens nucleus and coordinate eye movement with head movement.[2] Both the twitch motoneurons and the internuclear neurons receive bilateral afferent input from secondary vestibulo-ocular neurons in the MVN, saccadic burst neurons in the caudal pontine reticular nucleus, NPH, dorsal paragigantocellular nucleus (DPGi), and internuclear neurons of the oculomotor nucleus.[4]
Muscles
The abducens nucleus sends abducens nerve fibers to innervate the lateral rectus muscle directly. More recent work by the UCLA group suggests that the lateral rectus muscle has superior and inferior compartments innervated by superior and inferior divisions of the abducens nerve.[10] The thinking is that differential injury to these divisions may account for the small vertical strabismus sometimes seen in abducens nerve palsies.
Physiologic Variants
A hypothesis exists that variations in abducens nerve morphology may result from aberrant growth from the abducens nucleus.[6] Variations include a single nerve root that bifurcates and rejoins in the cavernous sinus and duplicate nerve roots that join in the cavernous sinus.
Clinical Significance
Damage to the abducens nuclei can occur from brainstem trauma, infiltration, ischemia, inflammation, compression, demyelination, or metabolic insult.[11] Congenital syndromes affecting the abducens nucleus are rare, but some cases have been documented. Abducens nerve paresis may serve as a non-localizing sign of increased intracranial pressure due to the long subarachnoid course of the nerve between the brainstem and clivus, where it can get stretched at the sharp edge of the petrous bone or compressed between the pons and the basilar artery.[12] Sever and or persistent abducens nerve palsy may raise concern for an occult neoplasm and prompt neuroradiologic investigation. Paresis of the abducens nerve produces an isolated ipsilateral abduction deficit. However, because of the intranuclear connections, lesions that damage the abducens nucleus produce a conjugate gaze palsy toward the side of the lesion rather than just an ipsilateral abduction weakness that would occur from isolated damage to the abducens nerve.[11] Lesions affecting both abducens nuclei eliminate the horizontal conjugate gaze.[3]
In many cases of injury to the abducens nuclei or fascicles, an ipsilateral facial nerve palsy is also present since the genu of the facial nerve fascicle passes around the abducens nucleus before exiting the brainstem.[13] Patients with presumed abducens nucleus lesions may also present with gaze-evoked nystagmus on the contralateral gaze from damage to adjacent vestibular nuclei or nucleus prepositus hypoglossi pathways involved in the neural integration for gaze holding. Nystagmus can also occur from damage to the cells or tracts of the abducens nucleus that have reciprocal connections with the cerebellar flocculus, which is also involved in gaze holding.[4] The one-and-a-half syndrome consists of an ipsilateral horizontal gaze palsy combined with an ipsilateral internuclear ophthalmoplegia (INO).[11] This condition occurs from damage to either the abducens nerve nucleus or the PPRF, with concomitant injury to the ipsilateral medial longitudinal fasciculus, which originates from the contralateral abducens nucleus and has crossed the midline. Therefore, the only preserved horizontal eye movement is the abduction of the contralateral eye (hence the term “one-and-a-half syndrome”). This syndrome may result from brainstem ischemia, MS, tumor, hemorrhage, trauma, infection, or another cause.
Congenital absence or hypoplasia of the abducens nucleus may occur with Mobius syndrome and Duane retraction syndrome.[14] Mobius syndrome is a rare neurological disorder involving weakness or paralysis of multiple cranial nerves, often CN VI and CN VII.[14] Patients present with facial diplegia and absent abduction or horizontal gaze bilaterally. Hypoplasia or atrophy of cranial nerve nuclei may be visible on neuroimaging, and most cases appear to be due to a prenatal vascular insult to the brainstem. Duane retraction syndrome is a congenital eye movement disorder characterized by limitation or absence of abduction, variable limitation of adduction, and globe retraction, causing palpebral fissure narrowing on attempted adduction.[15] All patients have abnormal horizontal eye movements, which appear to result from congenital agenesis of the abducens nucleus on the ipsilateral side. In some cases, patients have been found to have absent abducens nuclei and nerves on neuroimaging. Innervation of the lateral rectus in these cases is provided by the ipsilateral CN III, which produces globe retraction due to concomitant contraction of the medial and lateral rectus muscles on attempted adduction.
Electromyography may assist in distinguishing nuclear or infranuclear involvement from other causes of abduction defect due to a pathology of the lateral rectus muscle.[16] If the resting lateral rectus muscle shows normal electrical activity, significant nuclear involvement is unlikely to be the source of the abduction defect. Decreased electrical activity, fibrillation potentials, or polyphasic potentials may indicate nuclear or infranuclear involvement, which can present following axonal injury and degeneration.
Media
(Click Image to Enlarge)
References
Park HS, Chung MS, Shin DS, Jung YW, Park JS. Whole courses of the oculomotor, trochlear, and abducens nerves, identified in sectioned images and surface models. Anatomical record (Hoboken, N.J. : 2007). 2015 Feb:298(2):436-43. doi: 10.1002/ar.23048. Epub 2014 Sep 22 [PubMed PMID: 25212480]
Büttner-Ennever JA. The extraocular motor nuclei: organization and functional neuroanatomy. Progress in brain research. 2006:151():95-125 [PubMed PMID: 16221587]
Level 3 (low-level) evidenceKunchok A, Todd MJ, Halmagyi GM. Selective total conjugate horizontal gaze paralysis due to bilateral abducens nucleus lesions. Journal of neurology. 2016 Dec:263(12):2538-2539 [PubMed PMID: 27730375]
Horn AKE, Horng A, Buresch N, Messoudi A, Härtig W. Identification of Functional Cell Groups in the Abducens Nucleus of Monkey and Human by Perineuronal Nets and Choline Acetyltransferase Immunolabeling. Frontiers in neuroanatomy. 2018:12():45. doi: 10.3389/fnana.2018.00045. Epub 2018 Jun 19 [PubMed PMID: 29970992]
Yamaguchi K, Honma K. Development of the human abducens nucleus: a morphometric study. Brain & development. 2012 Oct:34(9):712-8. doi: 10.1016/j.braindev.2011.12.009. Epub 2012 Jan 24 [PubMed PMID: 22269150]
Wang JMH, Edwards BA, Loukas M, Oskouian RJ, Tubbs RS. Supernumerary Abducens Nerves: A Comprehensive Review. World neurosurgery. 2018 Apr:112():39-45. doi: 10.1016/j.wneu.2017.11.052. Epub 2017 Nov 20 [PubMed PMID: 29158094]
Gates P. The rule of 4 of the brainstem: a simplified method for understanding brainstem anatomy and brainstem vascular syndromes for the non-neurologist. Internal medicine journal. 2005 Apr:35(4):263-6 [PubMed PMID: 15836511]
Level 3 (low-level) evidenceBüttner-Ennever JA, Büttner U. Neuroanatomy of the ocular motor pathways. Bailliere's clinical neurology. 1992 Aug:1(2):263-87 [PubMed PMID: 1344070]
Level 3 (low-level) evidenceKeating EG, Gooley SG, Pratt SE, Kelsey JE. Removing the superior colliculus silences eye movements normally evoked from stimulation of the parietal and occipital eye fields. Brain research. 1983 Jun 13:269(1):145-8 [PubMed PMID: 6871695]
Level 3 (low-level) evidenceDemer JL. Compartmentalization of extraocular muscle function. Eye (London, England). 2015 Feb:29(2):157-62. doi: 10.1038/eye.2014.246. Epub 2014 Oct 24 [PubMed PMID: 25341434]
Level 3 (low-level) evidenceBae YJ, Kim JH, Choi BS, Jung C, Kim E. Brainstem pathways for horizontal eye movement: pathologic correlation with MR imaging. Radiographics : a review publication of the Radiological Society of North America, Inc. 2013 Jan-Feb:33(1):47-59. doi: 10.1148/rg.331125033. Epub [PubMed PMID: 23322826]
Parr M, Carminucci A, Al-Mufti F, Roychowdhury S, Gupta G. Isolated Abducens Nerve Palsy Associated with Ruptured Posterior Inferior Cerebellar Artery Aneurysm: Rare Neurologic Finding. World neurosurgery. 2019 Jan:121():97-99. doi: 10.1016/j.wneu.2018.09.096. Epub 2018 Sep 26 [PubMed PMID: 30266698]
Myckatyn TM, Mackinnon SE. A review of facial nerve anatomy. Seminars in plastic surgery. 2004 Feb:18(1):5-12. doi: 10.1055/s-2004-823118. Epub [PubMed PMID: 20574465]
Picciolini O, Porro M, Cattaneo E, Castelletti S, Masera G, Mosca F, Bedeschi MF. Moebius syndrome: clinical features, diagnosis, management and early intervention. Italian journal of pediatrics. 2016 Jun 3:42(1):56. doi: 10.1186/s13052-016-0256-5. Epub 2016 Jun 3 [PubMed PMID: 27260152]
Kalevar A, Ong Tone S, Flanders M. Duane syndrome: Clinical features and surgical management. Canadian journal of ophthalmology. Journal canadien d'ophtalmologie. 2015 Aug:50(4):310-3. doi: 10.1016/j.jcjo.2015.05.005. Epub [PubMed PMID: 26257226]
Feinberg J. EMG: myths and facts. HSS journal : the musculoskeletal journal of Hospital for Special Surgery. 2006 Feb:2(1):19-21. doi: 10.1007/s11420-005-0124-0. Epub [PubMed PMID: 18751841]