Introduction
The acromioclavicular (AC) joint is a common pain generator in patients presenting with shoulder pain. The incidence of AC joint pain is reported to be roughly 0.5 per 1000/year in primary care.[1] Pain in the AC joint can be traumatic or non-traumatic. Traumatic AC joint pain is typically the result of a direct blow to the superior or lateral aspect of the shoulder.[2] The impact results in a partial or complete tear of the ligamentous structures within the joint, more commonly known as a separated shoulder, and frequently occurs in contact sports such as football and hockey. Patients with separated shoulder often present with a notable deformity over their superior shoulder and pain directly over the AC joint. Traumatic AC joint pain is treated either conservatively with a sling and relative rest or with surgery if the injury is high-grade or severe.[3]
Patients with non-traumatic AC joint pain are usually older than 40 years of age and will typically present with focal shoulder pain located over the superior aspect of the shoulder.[4] The pain is usually insidious and made worse with cross-body adduction of the shoulder. Patients may also describe a grinding sensation in their shoulder. On physical exam, patients will typically have tenderness directly over the AC joint. Bringing the patient’s affected arm into adduction by having them reach across their body often reproduces the pain.
The most common non-traumatic causes of pain in the AC joint are overuse, degenerative changes, and distal clavicle osteolysis. Conservative management, including physical therapy, activity modification, and NSAIDs, are the first line of treatment.
In patients with chronic AC joint pain refractory to initial management, AC joint injections can be both diagnostic and therapeutic, resulting in significant relief. Providers must remain up to date on the indications, possible complications, and most effective methods of performing this procedure to benefit patients suffering from this condition maximally. This article reviews acromioclavicular (AC) joint injections and highlights the role of the healthcare team in performing this procedure.
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
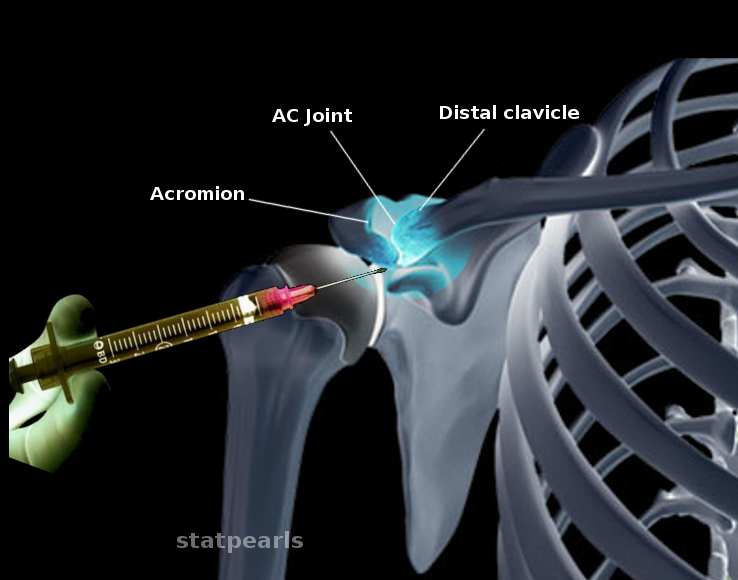
The acromioclavicular (AC) joint is part of the shoulder girdle and connects the distal clavicle to the acromion of the scapula.[5] A fibrocartilaginous disk and synovial membrane are within the joint. The acromioclavicular (AC) ligament provides horizontal stability to the joint, whereas the coracoclavicular (CC) ligament, consisting of the trapezoid and coronoid ligaments, provides vertical stability. The coracoacromial ligament, as well as the attachments of the deltoid and trapezius muscles, provide additional stabilization.[6]
Indications
Like most joint injections, AC joint injections can be performed after or concomitantly with other conservative measures, including physical therapy, NSAIDs, and activity modifications. For patients with suspected AC joint osteoarthritis, an AC joint injection is possible for diagnostic purposes. Other indications include known AC joint osteoarthritis and distal clavicle osteolysis refractory to initial treatment modalities. Distal clavicle osteolysis usually results from prior trauma to the shoulder or from repetitive heavy lifting.[7] A separated shoulder is not a standard indication for injection, although post-traumatic degenerative conditions are a relative indication in specific clinical settings.[8]
Contraindications
Contraindications to AC joint injections include infection in or around the joint (septic arthritis), hypersensitivity or known allergy to the injected solution, skin breakdown at the injection site and a fracture at the proposed injection site. Caution is advisable in patients on anticoagulation or with known bleeding disorders.
Equipment
Equipment needed for this procedure includes:
- 3 to 5 mm syringe
- 1 to 1.5 inch 25 gauge needle
- 0.5 ml of anesthetic agent, lidocaine or bupivacaine
- 0.25 to 0.5 ml of a corticosteroid solution - methylprednisone is the preferred agent due to less risk of fat atrophy[9].
- Gloves
- Skin cleaning solution such as chlorhexidine
Personnel
Medical providers to include physicians, nurse practitioners, or physician assistants can perform AC joint injections. It is helpful to have a nurse present to assist with preparing the patient.
Preparation
The clinician should discuss the risks/benefits of the procedure with the patient and the patient, provider, and witness should sign a consent form. A time-out should be performed before starting the procedure.
Technique or Treatment
The patient should be in a seated position with his/her arm hanging to the side. To identify the AC joint, palpate the clavicle distally until its endpoint. Palpate the small depression just lateral to termination of the clavicle; this is the joint space. After identifying the AC joint, prepare the site with a cleaning solution such as chlorhexidine, and following preparation, insert the needle from the superior anterior approach and aim the needle inferiorly. If meeting resistance, redirect the needle slightly until it enters the joint space. Once in the joint, inject the solution slowly. Ultrasound, if available, can significantly improve the accuracy of AC joint injections[10]. The patient should remain seated for a few minutes following the injection in case they have a vasovagal response.
Upon completion of the injection, reevaluate patient and have them passively range the shoulder to determine whether there is clinical improvement. Inform the patient that pain can get worse over the next 48 hours if a steroid flare occurs. If the pain does worsen, instruct the patient to treat with ice and NSAIDs.
Complications
Complications of this procedure are not common but include infection, lack of improvement in pain or worsening of pain, hypopigmentation of the overlying skin, and fat atrophy.
Clinical Significance
If performed correctly, AC joint injections can be both diagnostic and therapeutic, resulting in significant pain relief for affected patients. The duration of relief varies from patient to patient and can last weeks to months[11]. Steroid injections can be repeated, but clinicians should be pursued with caution as multiple injections can result in degradation of joint cartilage over time.[12]
Enhancing Healthcare Team Outcomes
An AC joint injection is a minor procedure that can provide patients significant pain relief. As is the case with all procedures, it is not without risk. The importance of communication and coordination of care amongst the provider, nurse, acting as an interprofessional team, and the patient cannot be understated. Pharmacists may be involved in the preparation of the anesthetic and need to have clear communication with the rest of the team, although, in the outpatient setting, nurses will more likely perform this task. Providers should clearly communicate expectations and precautions to the healthcare team and the patient to drive excellent outcomes. Nurses should also be aware of these return precautions as they are often the first ones on the healthcare team to communicate with the patient and family. They should work with the surgeon to keep the family informed and contact the team if unexpected complications arise. Interprofessional teamwork is crucial to obtaining the best outcomes in AC joint injection therapy. [Level V]
Nursing, Allied Health, and Interprofessional Team Interventions
- Set up instrument tray
- Ensure the patient has given informed consent
- Educate the patient on the procedure
- Prep the patient
Nursing, Allied Health, and Interprofessional Team Monitoring
- Patient monitoring both during and after the procedure
- Ensure no hematoma formation
- Ensure that the patient has no pain or arm weakness
Media
References
van der Windt DA,Koes BW,de Jong BA,Bouter LM, Shoulder disorders in general practice: incidence, patient characteristics, and management. Annals of the rheumatic diseases. 1995 Dec; [PubMed PMID: 8546527]
Saccomanno MF,DE Ieso C,Milano G, Acromioclavicular joint instability: anatomy, biomechanics and evaluation. Joints. 2014 Apr-Jun; [PubMed PMID: 25606549]
Monica J,Vredenburgh Z,Korsh J,Gatt C, Acute Shoulder Injuries in Adults. American family physician. 2016 Jul 15; [PubMed PMID: 27419328]
Walton J,Mahajan S,Paxinos A,Marshall J,Bryant C,Shnier R,Quinn R,Murrell GA, Diagnostic values of tests for acromioclavicular joint pain. The Journal of bone and joint surgery. American volume. 2004 Apr; [PubMed PMID: 15069148]
Hyland S,Varacallo M, Anatomy, Shoulder and Upper Limb, Clavicle . 2019 Jan [PubMed PMID: 30252246]
Chang KV,Mezian K,Na?ka O,Wu WT,Lin CP,�z�akar L, Ultrasound-guided interventions for painful shoulder: from anatomy to evidence. Journal of pain research. 2018; [PubMed PMID: 30349357]
DeFroda SF,Nacca C,Waryasz GR,Owens BD, Diagnosis and Management of Distal Clavicle Osteolysis. Orthopedics. 2017 Mar 1; [PubMed PMID: 27925640]
Gultekin S,Chaker Jomaa M,Jenkin R,Orchard JW, Use and Outcome of Local Anesthetic Painkilling Injections in Athletes: A Systematic Review. Clinical journal of sport medicine : official journal of the Canadian Academy of Sport Medicine. 2019 Feb 13 [PubMed PMID: 30789366]
Level 1 (high-level) evidenceAllen GM, The diagnosis and management of shoulder pain. Journal of ultrasonography. 2018; [PubMed PMID: 30451406]
Javed S,Sadozai Z,Javed A,Din A,Schmitgen G, Should all acromioclavicular joint injections be performed under image guidance? Journal of orthopaedic surgery (Hong Kong). 2017 Sep-Dec; [PubMed PMID: 28933229]
Chaudhury S,Bavan L,Rupani N,Mouyis K,Kulkarni R,Rangan A,Rees J, Managing acromio-clavicular joint pain: a scoping review. Shoulder [PubMed PMID: 29276532]
Level 2 (mid-level) evidenceMcAlindon TE,LaValley MP,Harvey WF,Price LL,Driban JB,Zhang M,Ward RJ, Effect of Intra-articular Triamcinolone vs Saline on Knee Cartilage Volume and Pain in Patients With Knee Osteoarthritis: A Randomized Clinical Trial. JAMA. 2017 May 16; [PubMed PMID: 28510679]
Level 1 (high-level) evidence