Introduction
Auditory brainstem response (ABR), also known as brainstem auditory Evoked Potentials (BAEP), is an objective measurement of auditory pathway function from the auditory nerve to the mesencephalon. ABR tests synchronous neural function and can estimate hearing sensitivity thresholds in individuals who are unable to tolerate traditional behavioral audiometry.[1]
Electrical activity from the eighth cranial nerve and neurons along the brainstem auditory pathway are recorded by surface electrodes placed on the scalp, forehead, and near the ears for 10 milliseconds after an acoustic stimulus.[2] The readings consist of a sequence of up to 7 positive wave peaks labeled I-VII with negative troughs in-between. It was first introduced into audiology in the 1970s, and its importance has increased with the contemporary guidelines of newborn hearing screening for hearing loss within 3 months of age.[3] It is now essential in the diagnosis of hearing loss, acoustic tumors, and cerebellopontine angle (CPA) tumors.[4]
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
ABR measures the synchronous neural fiber activity along the auditory pathway to determine hearing thresholds. Mechanical sound is transformed into electrical signals in the cochlea and transmitted to the brain through the auditory nerve or vestibulocochlear nerve (cranial nerve VIII). Electrical information to the auditory cortex travels along an ascending path through a series of nuclei including the cochlear nuclei, superior olivary complex, lateral lemniscus, inferior colliculi, and medial geniculate nuclei.[5]
The cochlear hair cells transform physical sound input into bioelectrical action potentials that are then transmitted to the spiral ganglion which comprise the main component of the auditory nerve. The cochlea has a unique tonotopic organization with high frequency sounds stimulating the basal component and low frequency sounds stimulating the apical component. Auditory nerve fibers from the low-frequency, apical portion of the cochlea and the high-frequency, basal portion travel along with the central and peripheral parts of the auditory nerve, respectively.[6]
The cochlear nucleus is the first relay point of the brainstem along the auditory pathway. The cochlear nucleus is located at the posterolateral portion of the brainstem and is cochleo-topically divided with low-frequency fibers on its ventral region and high-frequency fibers on its dorsal region.
After the cochlear nucleus, the majority of neural fibers decussate across the midline into the contralateral superior olivary complex.[5][6] The neural fibers from the superior olivary nuclei are then transmitted to the ipsilateral inferior colliculus via the lateral lemniscus tract.[7] The medial geniculate nucleus in the thalamus receives afferent input from the inferior colliculus and projects it to the tonotopically organized auditory cortex.[6]
Indications
Clinical applications of the ABR include identification of suspected neurological abnormalities of the cranial nerve VIII as well as the associated auditory pathways and the estimation of hearing sensitivity for those who are not able to accurately provide behavioral hearing evaluation information.
ABR has been the gold standard for assessing and confirming hearing loss in infants who fail their newborn hearing screen. Testing takes place while the infant is asleep or sedated with thresholds highly correlative with those of conventional behavioral audiometry.[8]
ABR is also indicated for young children or even adults with inconclusive audiometric thresholds or who are unable to tolerate conventional behavioral audiometry testing.[9] In children who pass their newborn hearing screen but are exposed to ototoxicity agents such as chemotherapy, aminoglycoside antibiotics, or heavy metals, ABR can be used to monitor for developing hearing loss.[10]
In addition to hearing loss, ABR can be used to diagnose vestibular schwannomas, brainstem lesions, de-myelination disease, and auditory neuropathy. ABR has a diagnostic accuracy of 92 to 98% for large acoustic tumors (> 1.5 cm),[11][12] but smaller tumors (< 1.5 cm) are missed in 30% of cases.[13][14][15][16] Wave V latency on ABR is predominately influenced by high-frequency regions in the cochlea, and small acoustic tumors may not disrupt high-frequency fibers enough to result in abnormal ABR waveforms.[16]
ABR can identify neural dysfunction in non-tumor, demyelinating diseases such as stroke, multiple sclerosis, syphilis, Wilson’s disease, and viral infections.[4] Auditory neuropathy spectrum disorder (ANSD) is a heterogeneous group of diseases in which neural signal from the inner ear to the brain is disrupted, but there are no visible changes to the nerve seen on brain MRI.[17] ANSD, also termed auditory dys-synchrony, is a clinical diagnosis that describes an auditory disorder caused by dysfunction of the synapse of the inner hair cells and auditory nerve. These patients typically present with normal cochlear outer hair cell function and abnormal auditory pathway function, beginning with the eighth nerve by evidence of absent or severely abnormal auditory brainstem response potentials. These individuals may have impaired speech understanding and show normal to severely impaired speech detection and pure tone hearing thresholds.
Contraindications
ABR is not indicated for patients who can undergo traditional standard audiometry. Furthermore, patients who have upper airway obstruction, central respiratory depression, epilepsy, respiratory infection, heart failure, prolonged QT syndrome, renal failure, and porphyria should not undergo sedated ABR using phenobarbital or hydroxyzine dihydrochloride as sleep agents.[18]
Equipment
The following equipment is required:
- Surface electrodes
- Earphones
- Electrode gel
- Laptop with ABR analyzing software
- Otoscopic microscope
- Myringotomy surgical tray (ear speculum, curettes, alligator forceps)
Personnel
The requisite personnel include:
- Audiologist
- Otolaryngologist
- Anesthesiologist
- Surgical technician
- Circulating nurse
Preparation
ABR testing for infants is performed when the infant is asleep and is limited to the duration of the patient’s nap. Patients are kept awake and sleep-deprived until the start of the procedure to maximize the time of sleep. For patients who are unable to maintain a sufficient duration of sleep for accurate results, sedation or general anesthesia may be required. A full sleep state is not required when ABR testing is performed on adults; however, they need to be in a quiet and relaxed state during the test to reduce muscle or movement artifact.
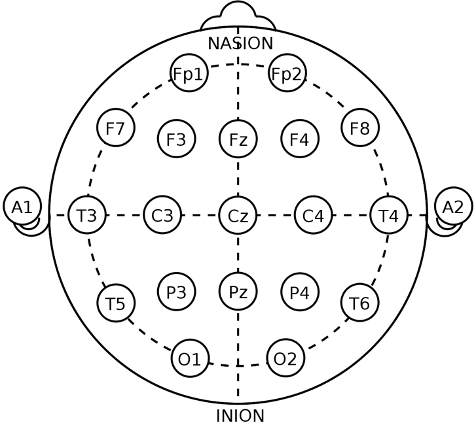
Detailed patient history is required prior to conscious sedation, including medical illnesses, medications, drug allergies, and adverse drug reactions. Oral intake is stopped 8 hours prior to sedation. Prior to placement of the surface electrodes, the external auditory canals are examined by the otolaryngologist under otomicroscopy (see Image. International 10-20 System for Surface Electrode Placement). Cerumen and debris are cleared out with care not to cause canal trauma or bleeding, which can attenuate the auditory stimulus. If middle ear effusion is present, the physician will consider a myringotomy with fluid evacuation and possible myringotomy tube placement. Testing will be inaccurate if there is fluid in the middle ear during the test.
Technique or Treatment
For electroencephalography and polysomnography exams, the scalp electrodes are placed based on the International 10-20 system. Each region is labeled, including pre-frontal (Fp), frontal (F), temporal (T), parietal (P), occipital (O), and central (C). The midline sagittal plane is labeled as Z. Even-numbered electrodes are on the right side of the scalp, and odd-numbered electrodes are on the left side of the scalp.[19]
During ABR testing, a positive electrode is placed at the vertex (Cz) or the high forehead (FPz). Two electrodes are placed on the right and left ear lobes or mastoids (A1, A2). A ground electrode is placed posteriorly at Pz or the lower forehead.
When performing the ABR for a neurological assessment, acoustic stimuli are delivered through insert earphones at a high intensity of 80-90dBnHL for adults at both a standard and high repetition rate. If the patient has hearing loss, the sound intensity can be adjusted to 60-65 dB SL. Hearing Level (HL) is based on the hearing threshold of a normal control population, whereas Sensation Level (SL) is based on the hearing threshold of the tested ear. Thus, 60 to 65 dB SL would imply a stimulus that is 60-65 decibels above the test ear’s threshold of hearing. The intensity of stimulation should be increased by 10 dB increments until reproducible waveforms are obtained, allowing the analysis of thresholds.[18] The resulting waveforms are evaluated for reproducibility, morphology, and latency. The latencies are compared from the right and left sides to determine if there is abnormal neural synchrony or retrocochlear pathology. The Wave V latency should be no more than a 0.4-millisecond difference between ears.
The stimuli are given monoaurally to compare the responses between the ears as well as to prevent any cross-contamination of stimuli. However, stimuli to one ear can reach the other ear through air and bone conduction and create an evoked potential in the contralateral, non-test ear. To prevent this, the non-tested ear is masked using continuous white noise at 30-40 dB below that of the stimuli. Evoked potentials are recorded for 10 milliseconds after the stimulus and can be extended to 20 milliseconds for patients with pathologically prolonged waveform latencies.
Interpretation
The primary measurements from an ABR are the absolute wave latencies, amplitudes, and interwave intervals between waves I to III, III to V, and I to V. The final ABR result is the averaged responses to several thousand repetitions of a stimulus.[20]
Wave latency is defined by the time between the initial auditory stimulus and the peak of a wave.[18] Latencies can be affected by age and intensity of stimulation. Latencies are longer in newborns and shorten with age. As stimulus intensity increases, the latency also shortens. Decreased stimulus intensity is associated with longer absolute wave latencies, decreased wave peak amplitudes, and loss of waves I, III, and V.
Wave amplitude is defined by the height between the wave peak and the succeeding trough. The amplitude is determined by the stimulus intensity and amount of synchronized neural activity. The more fibers that are simultaneously activated, the larger the peak amplitude.[18]
The ABR may be utilized to estimate hearing levels and can determine the type and degree of hearing loss if present. The threshold of ABR is the lowest stimulus intensity at which reproducible ABR waveforms can be detected. It provides a good estimation for the hearing sensitivity threshold.[21]
Broadband click stimulus is the standard for the majority of ABR testing that can be utilized to estimate thresholds of hearing sensitivity between 2000 and 4000 Hz.[22] However, disadvantages of the click stimulus include an abrupt onset and short duration. The broad frequency spectrum can also cause a temporal delay of the traveling wave along the cochlear partition leading to an asynchronous nerve firing pattern on ABR.[23][24][25][26] Click-evoked ABR has been shown to have greater synchrony with high-frequency neural fibers at the cochlear based compared to more scattered neural activity with low-frequency fibers at the cochlear apex.
The chirp stimulus addresses the temporal delay of the click stimulus by delaying the high-frequency component to give time for the lower frequency stimulus to reach the cochlear apex.[25][27] This leads to improved synchrony and reproducibility of waveforms with larger amplitudes.[1][24][26]
Another option is to perform frequency-specific, tone burst-evoked ABR to assess for hearing thresholds beyond the 1000 to 4000 Hz range. Frequency stimuli utilized most commonly include 500, 1000, 2000, and 4000 Hz to mimic the standard in-clinic pure-tone audiogram. This method has shown an accurate correlation with the pure-tone audiogram and in predicting the magnitude and pattern of hearing loss.[28][29]
Anatomical Generators
There is controversy regarding the exact anatomical attributions for each wave. Historically, each waveform was thought to correspond to a single anatomical site but is now established that each wave draws contributions from multiple anatomic sources.[2][30][31]
- Wave I is generated at the distal portion of the auditory nerve with an absolute latency of 1.5 msec.[18][30][32][30][18]
- Wave II is associated with the proximal portion of the auditory nerve and cochlear nucleus with an absolute latency of 2.5 msec.[18])[30]
- Wave III is associated with the cochlear nucleus and superior olivary complex with an absolute latency of 3.5 msec. As the superior olivary complex receives bilateral contributions, wave III anomalies are more pronounced on the stimulated ear ipsilateral to the lesion.[6][18][32]
- Wave IV corresponds to the superior olivary complex and ascending auditory fibers of the lateral lemniscus with an absolute latency of 4.5 msec.[6][18]
- Wave V corresponds to the lateral lemniscus and inferior colliculus with an absolute latency of 5.5 msec.[6][18][33][34][35][34][33][18] Wave IV and V are usually affected by brainstem lesions.[18]
Hearing loss is first assessed to be attributed to the peripheral or central auditory pathway. Peripheral hearing loss presents with delayed latency of wave I or absence of all waveforms. Etiology can be conductive or cochlear pathology. A central hearing loss presents with a prolonged interwave peak between wave I to V.
For patients with increased waveform latencies, increasing the intensity of sound stimulus can differentiate between conductive hearing loss versus slowed neural conduction. For patients with conductive hearing loss, increasing the intensity can overcome the conductive loss and results in normally evoked potentials. Patients who fail to have normalized evoked potentials after increasing stimulus intensity likely have neural conduction pathology.
Increased interwave latency of the I-III interval can indicate auditory nerve and cochlear pathology. Increased latency of the III-V interval can indicate a central pathology above the cochlear nerve such as neuromas, hydrocephalus, anoxic encephalopathy, corpus callosum anomalies, bilirubin encephalopathy, or Charcot’s disease. [18] Absent IV or V waves are seen in pathologies involving the mid-upper pons.[31] Differences in interaural latency in wave V can represent vestibular schwannomas. Patients with auditory neuropathy have altered temporal synchrony of their auditory brainstem pathway and can present with an absent or significantly abnormal ABR.[31]
Abnormal ABR was found in more than 95% of patients with vestibular schwannomas.[36][37] The probability of abnormal BAEP is less in patients with smaller (<1 cm) tumors.[38] Enlargement of vestibular schwannoma compresses the auditory nerve leading to prolongation of the wave I-III interpeak interval and eventual eradication of wave III and subsequent components. Wave I anomalies may be from compression of the internal auditory artery causing cochlear ischemia and dysfunction. Further internal artery compression can cause cochlear infarction resulting in loss of all waveforms, which is common in patients with large tumors who are deaf preoperatively. As the mass enlarges into the posterior fossa, it can compress the brainstem and create prolongation of the III-V interpeak interval for the contralateral ear to the tumor.[39]
Postoperatively, the patient can resume normal activities immediately after the procedure. If the patient required sedation, they would be monitored in the recovery room until the anesthesia wears off.
Complications
For patients that need general anesthesia or sedation for ABR testing, parents should be educated on the risk of neurotoxicity on the developing brain. Studies have shown that only a few hours of anesthesia exposure can result in neuronal loss in young animals, with adverse effects persisting in later life.[40] Prolonged anesthetic exposure in children has been associated with learning disabilities.[41]
The US Food and Drug Administration (FDA) has issued warnings that general anesthesia and sedation should be minimized for children under 3 years old and limited to 3 cumulative hours.[20]
Clinical Significance
The primary clinical goals of ABR are to diagnose hearing loss in newborns, vestibular schwannomas, and brainstem lesions.[6]
ABR is critical to diagnose hearing loss in newborns and young children who are unable to undergo traditional behavioral auditory testing. Early diagnosis can establish prompt auditory rehabilitation such as hearing aids, cochlear implants, or hearing/speech therapy programs. Early intervention has been shown to promote improved speech and language development in children.[42][43][44]
Vestibular schwannomas compress the auditory nerve, resulting in delayed ABR waveforms and non-synchronous activity along the auditory pathway. The interaural difference in the latencies of wave V and interweave form latencies are analyzed. The ABR is abnormal and suggestive of vestibular schwannoma when the interaural latency difference is longer than 0.3 milliseconds and the I-V interwave latency is longer than 4.4 milliseconds. ABR can also be utilized intraoperatively during intracranial cerebral pontine angle (CPA) tumor resections to help preserve auditory function.[45] Brainstem lesions from a demyelinating disease such as multiple sclerosis can also be diagnosed on ABR with non-synchronous neural activity and an absent wave V.[46]
Enhancing Healthcare Team Outcomes
Patients diagnosed with hearing loss, vestibular schwannoma, or brainstem lesions on ABR should be managed by a multidisciplinary team of otolaryngologists, neurosurgeons, neurologists, audiologists, speech-language pathologists, pediatricians, and primary care physicians. Children with hearing loss should be immediately referred for hearing augmentation with hearing aids, cochlear implants, and/or speech rehabilitation to promote long-term speech and language outcomes. Long-term monitoring of childhood development should be monitored by the pediatrician with regular follow-ups with audiology for routine hearing aid and audiogram assessments. Formal peer support groups with hearing loss can aid children and parents in addressing their concerns. The school system should also be involved to provide an optimal learning environment for children with hearing impairments.
Patients with vestibular schwannoma or brainstem lesions will need a referral to otolaryngology, neurosurgery, and neurology to determine management. If resection of the brainstem lesion is recommended, intraoperative ABR by an audiologist can help preserve auditory function. If resection is not recommended, long-term monitoring by the primary care physician, neurologist, neurosurgery, and otolaryngologist is recommended.
Media
(Click Image to Enlarge)
References
Bargen GA. Chirp-Evoked Auditory Brainstem Response in Children: A Review. American journal of audiology. 2015 Dec:24(4):573-83. doi: 10.1044/2015_AJA-15-0016. Epub [PubMed PMID: 26649461]
Jewett DL, Williston JS. Auditory-evoked far fields averaged from the scalp of humans. Brain : a journal of neurology. 1971:94(4):681-96 [PubMed PMID: 5132966]
American Academy of Pediatrics, Joint Committee on Infant Hearing. Year 2007 position statement: Principles and guidelines for early hearing detection and intervention programs. Pediatrics. 2007 Oct:120(4):898-921 [PubMed PMID: 17908777]
Peterein JL,Neely JG, Auditory brainstem response testing in neurodiagnosis: structure versus function. Journal of the American Academy of Audiology. 2012 Apr; [PubMed PMID: 22463940]
Level 3 (low-level) evidenceFelix RA 2nd, Gourévitch B, Portfors CV. Subcortical pathways: Towards a better understanding of auditory disorders. Hearing research. 2018 May:362():48-60. doi: 10.1016/j.heares.2018.01.008. Epub 2018 Jan 31 [PubMed PMID: 29395615]
Level 3 (low-level) evidenceBiacabe B, Chevallier JM, Avan P, Bonfils P. Functional anatomy of auditory brainstem nuclei: application to the anatomical basis of brainstem auditory evoked potentials. Auris, nasus, larynx. 2001 Jan:28(1):85-94 [PubMed PMID: 11137368]
Pecka M, Siveke I, Grothe B, Lesica NA. Enhancement of ITD coding within the initial stages of the auditory pathway. Journal of neurophysiology. 2010 Jan:103(1):38-46. doi: 10.1152/jn.00628.2009. Epub 2009 Oct 21 [PubMed PMID: 19846624]
Level 3 (low-level) evidenceGorga MP,Kaminski JR,Beauchaine KL,Jesteadt W,Neely ST, Auditory brainstem responses from children three months to three years of age: normal patterns of response. II. Journal of speech and hearing research. 1989 Jun; [PubMed PMID: 2739379]
Kanji A, Khoza-Shangase K, Moroe N. Newborn hearing screening protocols and their outcomes: A systematic review. International journal of pediatric otorhinolaryngology. 2018 Dec:115():104-109. doi: 10.1016/j.ijporl.2018.09.026. Epub 2018 Sep 25 [PubMed PMID: 30368368]
Level 1 (high-level) evidenceDille MF, Ellingson RM, McMillan GP, Konrad-Martin D. ABR obtained from time-efficient train stimuli for cisplatin ototoxicity monitoring. Journal of the American Academy of Audiology. 2013 Oct:24(9):769-81. doi: 10.3766/jaaa.24.9.2. Epub [PubMed PMID: 24224985]
Glasscock ME 3rd, Jackson CG, Josey AF, Dickins JR, Wiet RJ. Brain stem evoked response audiometry in a clinical practice. The Laryngoscope. 1979 Jul:89(7 Pt 1):1021-35 [PubMed PMID: 449545]
Bauch CD,Rose DE,Harner SG, Auditory brain stem response results from 255 patients with suspected retrocochlear involvement. Ear and hearing. 1982 Mar-Apr; [PubMed PMID: 7075874]
Gordon ML, Cohen NL. Efficacy of auditory brainstem response as a screening test for small acoustic neuromas. The American journal of otology. 1995 Mar:16(2):136-9 [PubMed PMID: 8572110]
Gosepath K, Maurer J, Mann W. [Diagnostic intra-meatal acoustic neurinoma--the role of acoustically evoked brain stem potentials and other otoneurologic studies]. Laryngo- rhino- otologie. 1995 Dec:74(12):728-32 [PubMed PMID: 8579671]
Godey B, Morandi X, Beust L, Brassier G, Bourdinière J. Sensitivity of auditory brainstem response in acoustic neuroma screening. Acta oto-laryngologica. 1998 Jul:118(4):501-4 [PubMed PMID: 9726673]
Level 2 (mid-level) evidenceDon M,Kwong B,Tanaka C,Brackmann D,Nelson R, The stacked ABR: a sensitive and specific screening tool for detecting small acoustic tumors. Audiology [PubMed PMID: 15925862]
Level 1 (high-level) evidenceStarr A, Rance G. Auditory neuropathy. Handbook of clinical neurology. 2015:129():495-508. doi: 10.1016/B978-0-444-62630-1.00028-7. Epub [PubMed PMID: 25726287]
Rouillon I, Parodi M, Denoyelle F, Loundon N. How to perform ABR in young children. European annals of otorhinolaryngology, head and neck diseases. 2016 Dec:133(6):431-435. doi: 10.1016/j.anorl.2016.05.004. Epub 2016 Jul 21 [PubMed PMID: 27453092]
. American Electroencephalographic Society guidelines for standard electrode position nomenclature. Journal of clinical neurophysiology : official publication of the American Electroencephalographic Society. 1991 Apr:8(2):200-2 [PubMed PMID: 2050819]
Level 1 (high-level) evidencePolonenko MJ, Maddox RK. The Parallel Auditory Brainstem Response. Trends in hearing. 2019 Jan-Dec:23():2331216519871395. doi: 10.1177/2331216519871395. Epub [PubMed PMID: 31516096]
Sininger YS, Auditory brain stem response for objective measures of hearing. Ear and hearing. 1993 Feb; [PubMed PMID: 8444334]
Coats AC, Martin JL. Human auditory nerve action potentials and brain stem evoked responses: effects of audiogram shape and lesion location. Otolaryngology. 1978 Jan-Feb:86(1):ORL-110 [PubMed PMID: 114907]
Pantev C, Lagidze S, Pantev M, Kevanishvili Z. Frequency-specific contributions to the auditory brain stem response derived by means of pure-tone masking. Audiology : official organ of the International Society of Audiology. 1985:24(4):275-87 [PubMed PMID: 4051877]
Chertoff M, Lichtenhan J, Willis M. Click- and chirp-evoked human compound action potentials. The Journal of the Acoustical Society of America. 2010 May:127(5):2992-6. doi: 10.1121/1.3372756. Epub [PubMed PMID: 21117748]
Dau T, Wegner O, Mellert V, Kollmeier B. Auditory brainstem responses with optimized chirp signals compensating basilar-membrane dispersion. The Journal of the Acoustical Society of America. 2000 Mar:107(3):1530-40 [PubMed PMID: 10738807]
Wegner O,Dau T, Frequency specificity of chirp-evoked auditory brainstem responses. The Journal of the Acoustical Society of America. 2002 Mar; [PubMed PMID: 11931309]
Elberling C, Don M. Auditory brainstem responses to a chirp stimulus designed from derived-band latencies in normal-hearing subjects. The Journal of the Acoustical Society of America. 2008 Nov:124(5):3022-37. doi: 10.1121/1.2990709. Epub [PubMed PMID: 19045789]
Suzuki J, Kodera K, Kaga K. Auditory evoked brainstem response assessment in otolaryngology. Annals of the New York Academy of Sciences. 1982:388():487-513 [PubMed PMID: 6953884]
Kodera K, Yamane H, Yamada O, Suzuki JI. Brain stem response audiometry at speech frequencies. Audiology : official organ of the International Society of Audiology. 1977 Nov-Dec:16(6):469-79 [PubMed PMID: 921605]
Legatt AD, Arezzo JC, Vaughan HG Jr. The anatomic and physiologic bases of brain stem auditory evoked potentials. Neurologic clinics. 1988 Nov:6(4):681-704 [PubMed PMID: 3070334]
Level 3 (low-level) evidenceDavies RA. Audiometry and other hearing tests. Handbook of clinical neurology. 2016:137():157-76. doi: 10.1016/B978-0-444-63437-5.00011-X. Epub [PubMed PMID: 27638069]
Melcher JR, Guinan JJ Jr, Knudson IM, Kiang NY. Generators of the brainstem auditory evoked potential in cat. II. Correlating lesion sites with waveform changes. Hearing research. 1996 Apr:93(1-2):28-51 [PubMed PMID: 8735067]
Level 3 (low-level) evidenceMelcher JR,Kiang NY, Generators of the brainstem auditory evoked potential in cat. III: Identified cell populations. Hearing research. 1996 Apr; [PubMed PMID: 8735068]
Level 3 (low-level) evidenceBuchwald JS, Huang C. Far-field acoustic response: origins in the cat. Science (New York, N.Y.). 1975 Aug 1:189(4200):382-4 [PubMed PMID: 1145206]
Level 3 (low-level) evidenceCaird DM, Klinke R. The effect of inferior colliculus lesions on auditory evoked potentials. Electroencephalography and clinical neurophysiology. 1987 May:68(3):237-40 [PubMed PMID: 2436886]
Level 3 (low-level) evidenceBarrs DM, Brackmann DE, Olson JE, House WF. Changing concepts of acoustic neuroma diagnosis. Archives of otolaryngology (Chicago, Ill. : 1960). 1985 Jan:111(1):17-21 [PubMed PMID: 3966892]
Level 3 (low-level) evidenceZappia JJ,O'Connor CA,Wiet RJ,Dinces EA, Rethinking the use of auditory brainstem response in acoustic neuroma screening. The Laryngoscope. 1997 Oct; [PubMed PMID: 9331319]
Level 2 (mid-level) evidenceEl-Kashlan HK, Eisenmann D, Kileny PR. Auditory brain stem response in small acoustic neuromas. Ear and hearing. 2000 Jun:21(3):257-62 [PubMed PMID: 10890735]
Level 2 (mid-level) evidenceLegatt AD. Electrophysiology of Cranial Nerve Testing: Auditory Nerve. Journal of clinical neurophysiology : official publication of the American Electroencephalographic Society. 2018 Jan:35(1):25-38. doi: 10.1097/WNP.0000000000000421. Epub [PubMed PMID: 29298210]
Jevtovic-Todorovic V, Brambrick A. General Anesthesia and Young Brain: What is New? Journal of neurosurgical anesthesiology. 2018 Jul:30(3):217-222. doi: 10.1097/ANA.0000000000000432. Epub [PubMed PMID: 28622158]
Wilder RT, Flick RP, Sprung J, Katusic SK, Barbaresi WJ, Mickelson C, Gleich SJ, Schroeder DR, Weaver AL, Warner DO. Early exposure to anesthesia and learning disabilities in a population-based birth cohort. Anesthesiology. 2009 Apr:110(4):796-804. doi: 10.1097/01.anes.0000344728.34332.5d. Epub [PubMed PMID: 19293700]
Level 2 (mid-level) evidenceCullington HE, Bele D, Brinton JC, Cooper S, Daft M, Harding J, Hatton N, Humphries J, Lutman ME, Maddocks J, Maggs J, Millward K, O'Donoghue G, Patel S, Rajput K, Salmon V, Sear T, Speers A, Wheeler A, Wilson K. United Kingdom national paediatric bilateral project: Demographics and results of localization and speech perception testing. Cochlear implants international. 2017 Jan:18(1):2-22. doi: 10.1080/14670100.2016.1265055. Epub 2016 Dec 23 [PubMed PMID: 28010679]
Harrison RV, Gordon KA, Mount RJ. Is there a critical period for cochlear implantation in congenitally deaf children? Analyses of hearing and speech perception performance after implantation. Developmental psychobiology. 2005 Apr:46(3):252-61 [PubMed PMID: 15772969]
Ching TY,Day J,Van Buynder P,Hou S,Zhang V,Seeto M,Burns L,Flynn C, Language and speech perception of young children with bimodal fitting or bilateral cochlear implants. Cochlear implants international. 2014 May; [PubMed PMID: 24869442]
Level 2 (mid-level) evidenceMatthies C, Samii M. Management of vestibular schwannomas (acoustic neuromas): the value of neurophysiology for intraoperative monitoring of auditory function in 200 cases. Neurosurgery. 1997 Mar:40(3):459-66; discussion 466-8 [PubMed PMID: 9055284]
Level 3 (low-level) evidenceVoordecker P, Brunko E, de Beyl Z. Selective unilateral absence or attenuation of wave V of brain-stem auditory evoked potentials with intrinsic brain-stem lesions. Archives of neurology. 1988 Nov:45(11):1272-6 [PubMed PMID: 3190507]
Level 3 (low-level) evidence