Introduction
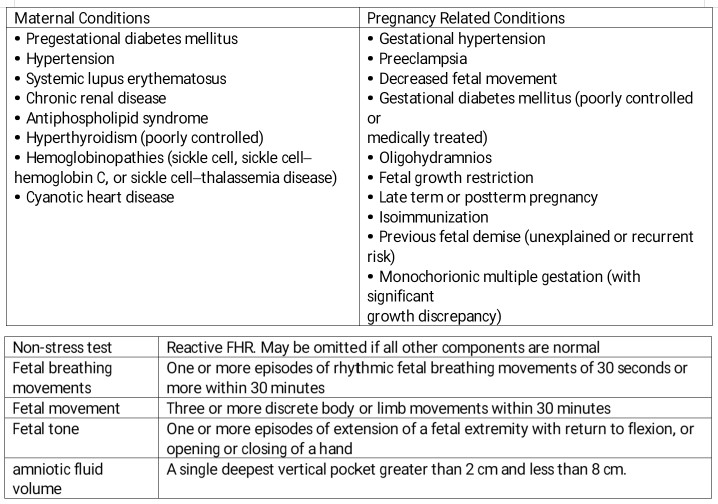
Point of care ultrasound (POCUS) in obstetrics is an invaluable tool in the evaluation of the pregnant patient. Given its ease of use and interpretation, a quick assessment can provide important information regarding the management of obstetric concerns. The biophysical profile (BPP) is a maximum 30-minute long ultrasound assessment to assess fetal well-being coupled with a fetal heart rate tracing. The elements are a non-stress test, assessment of fluid index, fetal breathing movements, total body movements, and limb tone demonstrated by flexion and extension of the limbs. The modified BPP is a shortened study that involves a non-stress test (NST) and amniotic fluid index (AFI). See Image. Ultrasound Biophysical Profile Table.
The history of this test has been the source of investigation from the 1970s to the 1990s. Initial studies were in fetal lambs and analyzed the cardiovascular and metabolic changes experienced in fetal lambs under controlled environments that altered the maternal pCO2 and cardiac output. Reflections in the fetal-placental, umbilical, and cardiovascular hemodynamics were monitored using vascular catheters and blood sampling. Additionally, the ultrasound findings and fetal heart rate (FHR) patterns were studied. In the 1990s, the correlation between these variables came together in a landmark study that identified a linear relationship between the BPP score and umbilical cord venous pH sampled via cordocentesis. Scores of 8 and 10 consistently had normal cord pH levels. However, a score of 0 exhibited a mean cord pH of 7.07 prompting urgent intervention or delivery. Researchers were able to break down the scores further and found that abnormal amniotic fluid correlated with a lower pH compared to short term abnormalities such as an abnormal NST or fetal breathing movements.[1] This ultimately provides the rationale for BPP scoring and obstetric management. The modified BPP provides almost as powerful a study as the full BPP and is normally part of antenatal testing for high risk maternal and fetal conditions.
Procedures
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Procedures
The ultrasound technique is simple and described as follows. The patient positioning is supine with the understanding that some of the gravid patients may become very uncomfortable lying horizontally. Accuracy is ensured by establishing fetal lie, natural tilt of the uterus, and size of the uterus. Near term, the umbilicus is a common center point for determining quadrants in the amniotic fluid index. However, secondary to the gestational age of the pregnancy and fetal size, this landmark can be deceiving, and probe positioning should be adjusted to achieve four roughly equal quadrants. The curvilinear probe is used with the depth ranging from 10 cm to 15 cm for most patients. Again, to ensure accuracy and reproducibility in the fluid assessment, the probe should be held in the sagittal plane and parallel to the bed taking care not to angle the probe cephalad or caudal. Measurements are taken in the vertical plane in a pocket of fluid that does not contain limbs or umbilical cord. The American College of Obstetrics and Gynecology recommends that a single deepest pocket (SDP) measurement is preferable over a four-quadrant AFI. The intent of this is to prevent unnecessary workup and early induction of labor for oligohydramnios. Regardless, all quadrants of fluid need to be assessed to know the single deepest pocket with confidence. For the fetal movement assessment, the probe will need to be angled to capture a window that clearly shows the target anatomy. Again, thirty minutes is the maximum time to spend on assessing fetal movement. The NST portion uses standard fetal monitoring to evaluate for at least two accelerations of at minimum 15 beats for at least 15 seconds in a 30-minute interval for gestational age greater than 32 weeks.
Indications
The indications for a biophysical profile are most commonly a nonreactive non-stress test or the presenting complaint of decreased fetal movement. However, many high risk obstetric and fetal conditions require this study to help guide management. Often a modified BPP is performed as part of antepartum testing for a variety of maternal and fetal conditions seen in the table below. The timing of the study is recommended to start at 32 weeks gestation for most fetal and maternal conditions. If there are multiple or severe conditions, antenatal testing can begin earlier. Given the high risk involved in providing obstetric care, any time an equivocal assessment occurs or intuition directs that the fetus may be distressed, a provider would not be wrong to perform a BPP.
Potential Diagnosis
Diagnosis and management must take into consideration maternal and fetal risk factors. A biophysical profile can only diagnose oligohydramnios or polyhydramnios. Otherwise, it is an indicator of fetal wellbeing reflecting the blood pH. A score of 8 to 10 is normal and provides reassurance that the risk of fetal asphyxia within 1 week is extremely low. Rates of this study being a false negative range from fetal death rates of 0.55 per 1000 to 0.83 per 1000.[2] A score of 6 is considered either equivocal or abnormal. If oligohydramnios is diagnosed, the study should be repeated in 24 hours or the patient should possibly be induced if at term. If the score is 6 and all the points off relate to fetal movement, this is more reassuring, but the study should be repeated in a short interval. A score of 2 to 4 is not reassuring, and the recommendation is to either move toward labor induction or cesarean section depending on what is most prudent. A score of 0 indicates impending fetal asphyxia and delivery should be by urgent cesarean section at a hospital with NICU capability.
Normal and Critical Findings
Each factor receives either 2 or 0 points. An abnormal fluid assessment is a chronic finding as maternal or fetal pathology reflects in the fluid amount only after many days.[3] It is always abnormal and should be followed up in short interval regardless if the other findings in the biophysical profile are normal. An NST should have two accelerations in twenty minutes. A variety of fetal breathing patterns is normal and ranges from rapid, regular breathing, sighs, pauses while swallowing, and intermittent long slow breaths during sleep cycles. Theses breathing variations exert a mechanical and chemical effect on the cardiac pacemaker which results in normal beat to beat variability in a healthy fetal heart rate tracing. This phenomenon explains the mechanism for lost variability and reactivity during fetal sleep cycles and also explains the rationale for the NST needing an extension beyond a 20-minute strip.
In the continuum of fetal distress, acidosis, hypoxia, and asphyxia, the fetal breathing movements are lost first, followed by body movements, then extremity tone. These findings should reflect in the fetal heart rate as decreased variability and absent accelerations. In a normal exam, there should be at least one episode of 30 seconds of fetal breathing movements in 30 minutes. For fetal body movements there should be at least three movements of the body or limbs in 30 minutes and for fetal tone at least one extension and flexion of a limb or opening and closing of a hand during the test.[4] The sum of the points is used to guide management discussed in the potential diagnosis section. A summary of the elements of the BPP is in the table below.
Interfering Factors
Factors that interfere are seen first in the fetal heart rate. Most commonly, fetal sleep cycles can contribute to a non-reactive NST, as well as a number of medications. Narcotics, magnesium sulfate, corticosteroids, and tocolytics are well known to cause a slowing in the FHR and lead to non-reactive FHR patterns.[5] Maternal obesity can make adequate visualization a challenge so depth and gain on the ultrasound may need to be adjusted.
Complications
Generally, the use of ultrasound in obstetrics is considered safe. However, the ACOG published a bulletin in 2017 regarding the limited use of interventions in pregnancy.[6][7][8][6] They note that it is generally accepted as a safe study; there is no way to know if prolonged or repeated exposure to ultrasound waves has a damaging effect on a fetus. Therefore the "As Low As Reasonably Achievable" (ALARA) principle is encouraged, which means only using ultrasound if there is a specific indication such as mentioned above.[4] Providers should be mindful of the thermal energy released by the probe which shows in the margins of the ultrasound display as a thermal index (TI). It is a ratio of the acoustic power emitted by the transducer to the power necessary to raise the temperature of the tissue one-degree Celsius anywhere along the beam. Ideally, recommendations are for settings that have the lowest thermal index.
Patient Safety and Education
In some obstetric patients, it is very uncomfortable to lie supine. For these cases, this positioning is needed only for the amniotic fluid assessment, and then reposition the patient in a more comfortable pose for the remainder of the BPP.
Clinical Significance
The outcomes of this study can be a challenge to interpret for intermediate scores knowing that a preterm delivery has several inherent risks to the mother and infant. Again, as mentioned above, with an equivocal score or an abnormal fluid index, the study can be repeated in 1 day. Nonreassuring studies should lead to a medical investigation as to why and preparing the mother and fetus for delivery. The urgency toward delivery must be based on consensus among the interdisciplinary medical team and take into account all factors such as gestational age, medical conditions, and capabilities of the hospital.
BPP takes into account multiple factors of fetal wellbeing, and it is a powerful tool to guide management in high-risk obstetric cases. It is easily reproducible and is performable in a variety of settings ranging from austere to the most prestigious hospitals.
Media
References
Manning FA, Snijders R, Harman CR, Nicolaides K, Menticoglou S, Morrison I. Fetal biophysical profile score. VI. Correlation with antepartum umbilical venous fetal pH. American journal of obstetrics and gynecology. 1993 Oct:169(4):755-63 [PubMed PMID: 8238129]
Manning FA, Morrison I, Harman CR, Lange IR, Menticoglou S. Fetal assessment based on fetal biophysical profile scoring: experience in 19,221 referred high-risk pregnancies. II. An analysis of false-negative fetal deaths. American journal of obstetrics and gynecology. 1987 Oct:157(4 Pt 1):880-4 [PubMed PMID: 3674161]
Level 2 (mid-level) evidenceMagann EF, Sandlin AT, Ounpraseuth ST. Amniotic fluid and the clinical relevance of the sonographically estimated amniotic fluid volume: oligohydramnios. Journal of ultrasound in medicine : official journal of the American Institute of Ultrasound in Medicine. 2011 Nov:30(11):1573-85 [PubMed PMID: 22039031]
. AIUM Practice Parameter for the Performance of Limited Obstetric Ultrasound Examinations by Advanced Clinical Providers. Journal of ultrasound in medicine : official journal of the American Institute of Ultrasound in Medicine. 2018 Jul:37(7):1587-1596. doi: 10.1002/jum.14677. Epub [PubMed PMID: 30133848]
Verdurmen KM, Renckens J, van Laar JO, Oei SG. The influence of corticosteroids on fetal heart rate variability: a systematic review of the literature. Obstetrical & gynecological survey. 2013 Dec:68(12):811-24 [PubMed PMID: 25102018]
Level 1 (high-level) evidenceSimpson L, Khati NJ, Deshmukh SP, Dudiak KM, Harisinghani MG, Henrichsen TL, Meyer BJ, Nyberg DA, Poder L, Shipp TD, Zelop CM, Glanc P. ACR Appropriateness Criteria Assessment of Fetal Well-Being. Journal of the American College of Radiology : JACR. 2016 Dec:13(12 Pt A):1483-1493. doi: 10.1016/j.jacr.2016.08.028. Epub 2016 Oct 28 [PubMed PMID: 28029583]
Zelop CM, Javitt MC, Glanc P, Dubinsky T, Harisinghani MG, Harris RD, Khati NJ, Mitchell DG, Pandharipande PV, Pannu HK, Podrasky AE, Shipp TD, Siegel CL, Simpson L, Wall DJ, Wong-You-Cheong JJ, American College of Radiology. ACR Appropriateness Criteria® growth disturbances - risk of intrauterine growth restriction. Ultrasound quarterly. 2013 Sep:29(3):147-51. doi: 10.1097/RUQ.0b013e31829ea221. Epub [PubMed PMID: 23867573]
Maulik D. Management of fetal growth restriction: an evidence-based approach. Clinical obstetrics and gynecology. 2006 Jun:49(2):320-34 [PubMed PMID: 16721110]