Introduction
Bitemporal hemianopsia (or bitemporal hemianopia) describes the ocular defect that leads to impaired peripheral vision in the outer temporal halves of the visual field of each eye. This condition commonly results from a tumor or lesion impinging on the optic chiasm, the decussation point of the optic nerve conveying visual information from the nasal retina in each eye.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
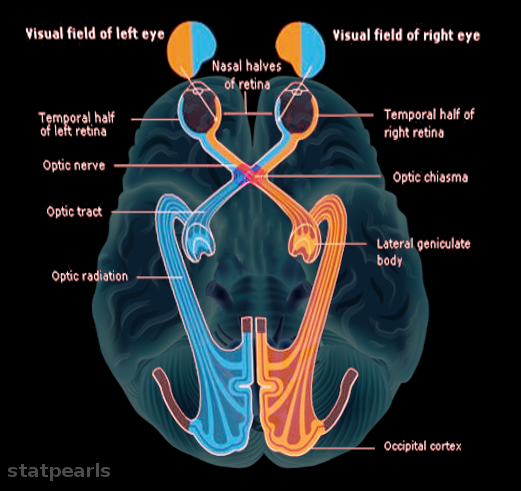
Cranial nerve II (CN II or optic nerve) runs along the midline of the ventral surface of the brain and conveys visual information from the retina of each eye to the corresponding region of the primary visual cortex. The right half of the visual field of both eyes is processed by the left half of the retina, while the right half of the retina processes the left half of the visual field. These retinal ganglion cells project myelinated axons, carrying CN II sensory afferent fibers, through the optic chiasm, where optic nerve fibers from the nasal half of each retina decussate to the contralateral side of the brain for processing. This decussation allows for greater organization of visual processing by directing all optic nerve fibers relaying information from the left visual field of both eyes to the right hemisphere of the brain and conversely, all fibers carrying the right visual field information to the left hemisphere. The optic chiasm positioning is along the midline of the ventral subarachnoid space of the brain, inferior to the hypothalamus and anterior communicating artery, and superior to the pituitary gland situated within the sella turcica. After passing through the optic chiasm, the optic nerve becomes the optic tract that synapses to the lateral geniculate nucleus (LGN) of the thalamus and subsequently projects optic radiations to the primary visual cortex (V1) of the occipital lobe. The optic tract also projects to the superior colliculus, pretectal nuclei, and suprachiasmatic nuclei.[1] This part of the optic pathway serves the important light reflex.
Embryology
Ocular structure development begins around gestational week three.[2] Both the retina and optic nerve originate from the neural ectoderm.[3] Therefore, strictly speaking, the optic nerve is not a peripheral nerve but part of the central nervous system. Its myelin sheath gets produced and maintained by the oligodendrocytes and not Schwann cells as in real peripheral nerves. Around seven weeks gestation,[3] axonal projections of the retinal ganglion cells (RGCs) develop into the optic stalk and subsequently the optic nerve.[2]
Blood Supply and Lymphatics
Different branches of the circle of Willis provide blood to the primary visual structures at and around the optic chiasm. The optic nerve gets supplied by the superior hypophyseal artery and ophthalmic artery, both branches of the internal carotid artery (ICA).[4] The optic chiasm receives supply from the anterior communicating artery, anterior cerebral artery (ACA), posterior communicating artery, and superior hypophyseal artery.[5] The ICA and posterior communicating artery also deliver blood to the optic tract.[1]
Nerves
The optic nerves, one from each eye, are the sole nervous tissue transporting visual information from the retinal ganglion cells in the retina to the optic chiasm and ultimately to higher visual processing centers in the brain. Roughly 2.4 million optic nerve fibers pass through the optic chiasm. In general, temporal retinal fibers occupy the lateral portions of the optic chiasm, around 35% to 45% of the total area, and project to the LGN uncrossed. Although the exact topographical mapping of these fibers remains a topic of debate, the widely accepted view is that the remaining area is composed of decussating nasal optic nerve fibers.[6]
Physiologic Variants
Depending on the number of nasal optic nerve fibers affected, the extent of bitemporal hemianopsia can range from partial to complete. Complete bitemporal hemianopsia is more common, and patients with this condition have noted additional issues with binocular vision. The absence of any overlap between the intact nasal and impaired temporal visual fields leads to hemi-sliding, a phenomenon where the left and right nasal fields slide respective to each other instead of merging as a fused image.[7]
The inferior nasal fibers which carry fibers from the retinal ganglion cells responsible for seeing objects in the contralateral superior temporal visual field, pass forward slightly in the contralateral optic nerve before they travel backward towards the lateral geniculate body. A compressive lesion here will result in an anterior chiasmal syndrome as described below.
Surgical Considerations
Tumors around the optic chiasm, leading to bitemporal hemianopsia, are difficult to resect given the limited area and proximity of critical nervous and neurovascular structures. Associated cranial nerve deficits can occur in as many as 56% of cases and even end in mortality in up to 9% of resection surgeries.[8] Two established surgical techniques are microscopic transsphenoidal surgery[9] and endoscopic endonasal surgery (EES) [10] Recent meta-analyses comparing these two procedures regarding pituitary adenomas have shown mixed results for which is overall more beneficial; however, both have proven to be effective resection techniques.[11][12]
Other less invasive options include stereotactic radiosurgery (SRS) as a promising alternative with a lower risk of complications.[8] Another consideration includes intensity-modulated photon radiotherapy (IMRT), a refined and targeted method of radiotherapy.[10]
Clinical Significance
Bitemporal hemianopsia impairs bilateral peripheral vision; however, the central field of vision from 110 to 120 degrees remains intact.[7] This range of vision still allows for generally normal function, yet other complications regarding the underlying cause may require more immediate medical attention. The unique presentation of bitemporal hemianopsia, impairing the temporal visual field of both eyes, helps to narrow down the likely diagnosis to a condition affecting the optic chiasm.[13] When a compressive lesion is located slightly more anterior, it will compress the ipsilateral optic nerve and the inferior nasal fibers from the contralateral optic nerve. The compression of the ipsilateral optic nerve leads to a central scotoma. The compression of the crossing inferior nasal fibers from the contralateral optic nerve will result in a contralateral upper quadrantic hemianopia. The combined deficits are called an anterior chiasmal syndrome, which may progress to bitemporal hemianopia with ipsilateral scotoma or blindness. Some of the most common causes are neoplasms, including pituitary adenomas, craniopharyngiomas, and meningiomas.[14]
Pituitary adenomas are benign tumors of the pituitary gland and the most common origin of masses near the sella turcica.[9] Due to the anatomical location of the optic chiasm superior to the pituitary gland, a suprasellar extension of a pituitary macroadenoma will lead to compression of the optic nerve fibers decussating at the optic chiasm.[9] Impingement of these nerves prevents visual information from the temporal visual fields of each eye from reaching the processing centers in the brain, leading to peripheral vision loss. Very rarely when a pituitary adenoma outgrows its blood supply, it will result in acute hemorrhagic infarction and acute swelling of the pituitary gland with pressure on the optic chiasma and cranial nerves in the cavernous sinus. This condition is a medical emergency called pituitary apoplexy. The patient will present with acute onset headache, ophthalmoplegia, and visual field defects of bitemporal hemianopia.
Craniopharyngiomas, a rare condition that presents most often in childhood (5 to 14 years) or as an adult (50 to 74 years), involves an outgrowth of the developmental remnants of Rathke’s pouch near the sella turcica.[15] The proximity of this mass to the optic chiasm also leads to bitemporal hemianopsia as a key clinical presentation of this condition.[16]
Meningiomas, the most prevalent form of intracranial tumors, are generally benign neoplasms of arachnoid cells with an insidious onset.[8] When located in the parasellar region, meningiomas can also present with bitemporal hemianopsia if located close enough to the optic chiasm to compress the medial optic nerve fibers on both sides.
Although rare, large anterior communicating artery aneurysms can potentially manifest with vision abnormalities, such as bitemporal hemianopsia.[17] The anterior communicating artery runs superiorly to the optic chiasm, and an aneurysm of this artery could impinge on the optic nerve fibers carrying peripheral visual information. Furthermore, comorbid conditions usually due to anterior communicating artery aneurysm ruptures, such as hematomas and vasospasms, can also exert pressure on these fibers.[17]
Media
References
De Moraes CG. Anatomy of the visual pathways. Journal of glaucoma. 2013 Jun-Jul:22 Suppl 5():S2-7. doi: 10.1097/IJG.0b013e3182934978. Epub [PubMed PMID: 23733119]
Bales TR, Lopez MJ, Clark J. Embryology, Eye. StatPearls. 2023 Jan:(): [PubMed PMID: 30860715]
Hoar RM. Embryology of the eye. Environmental health perspectives. 1982 Apr:44():31-4 [PubMed PMID: 7084153]
Level 3 (low-level) evidencevan Overbeeke J, Sekhar L. Microanatomy of the blood supply to the optic nerve. Orbit (Amsterdam, Netherlands). 2003 Jun:22(2):81-8 [PubMed PMID: 12789588]
Salaud C, Ploteau S, Blery P, Pilet P, Armstrong O, Hamel A. Extrinsic and intrinsic blood supply to the optic chiasm. Clinical anatomy (New York, N.Y.). 2018 Apr:31(3):432-440. doi: 10.1002/ca.23037. Epub 2017 Dec 27 [PubMed PMID: 29243332]
Jain NS, Jain SV, Wang X, Neely AJ, Tahtali M, Jain S, Lueck CJ. Visualization of Nerve Fiber Orientations in the Human Optic Chiasm Using Photomicrographic Image Analysis. Investigative ophthalmology & visual science. 2015 Oct:56(11):6734-9. doi: 10.1167/iovs.15-17443. Epub [PubMed PMID: 26567784]
Peli E, Satgunam P. Bitemporal hemianopia; its unique binocular complexities and a novel remedy. Ophthalmic & physiological optics : the journal of the British College of Ophthalmic Opticians (Optometrists). 2014 Mar:34(2):233-42. doi: 10.1111/opo.12118. Epub [PubMed PMID: 24588535]
Level 3 (low-level) evidenceCohen-Inbar O, Tata A, Moosa S, Lee CC, Sheehan JP. Stereotactic radiosurgery in the treatment of parasellar meningiomas: long-term volumetric evaluation. Journal of neurosurgery. 2018 Feb:128(2):362-372. doi: 10.3171/2016.11.JNS161402. Epub 2017 Mar 24 [PubMed PMID: 28338439]
Lake MG, Krook LS, Cruz SV. Pituitary adenomas: an overview. American family physician. 2013 Sep 1:88(5):319-27 [PubMed PMID: 24010395]
Level 3 (low-level) evidenceO'steen L, Indelicato DJ. Advances in the management of craniopharyngioma. F1000Research. 2018:7():. pii: F1000 Faculty Rev-1632. doi: 10.12688/f1000research.15834.1. Epub 2018 Oct 11 [PubMed PMID: 30363774]
Level 3 (low-level) evidenceEsquenazi Y, Essayed WI, Singh H, Mauer E, Ahmed M, Christos PJ, Schwartz TH. Endoscopic Endonasal Versus Microscopic Transsphenoidal Surgery for Recurrent and/or Residual Pituitary Adenomas. World neurosurgery. 2017 May:101():186-195. doi: 10.1016/j.wneu.2017.01.110. Epub 2017 Feb 6 [PubMed PMID: 28185971]
Akbari H, Malek M, Ghorbani M, Ramak Hashemi SM, Khamseh ME, Zare Mehrjardi A, Emami Z, Ebrahim Valojerdi A. Clinical outcomes of endoscopic versus microscopic trans-sphenoidal surgery for large pituitary adenoma. British journal of neurosurgery. 2018 Apr:32(2):206-209. doi: 10.1080/02688697.2018.1429569. Epub 2018 Feb 8 [PubMed PMID: 29417847]
Level 2 (mid-level) evidenceSwienton DJ, Thomas AG. The visual pathway--functional anatomy and pathology. Seminars in ultrasound, CT, and MR. 2014 Oct:35(5):487-503. doi: 10.1053/j.sult.2014.06.007. Epub 2014 Jun 25 [PubMed PMID: 25217301]
Foroozan R. Chiasmal syndromes. Current opinion in ophthalmology. 2003 Dec:14(6):325-31 [PubMed PMID: 14615635]
Level 3 (low-level) evidenceMüller HL. Craniopharyngioma. Endocrine reviews. 2014 Jun:35(3):513-43. doi: 10.1210/er.2013-1115. Epub 2014 Jan 27 [PubMed PMID: 24467716]
Garnett MR, Puget S, Grill J, Sainte-Rose C. Craniopharyngioma. Orphanet journal of rare diseases. 2007 Apr 10:2():18 [PubMed PMID: 17425791]
Seung WB, Kim DY, Park YS. A Large Ruptured Anterior Communicating Artery Aneurysm Presenting with Bitemporal Hemianopsia. Journal of Korean Neurosurgical Society. 2015 Sep:58(3):291-3. doi: 10.3340/jkns.2015.58.3.291. Epub 2015 Sep 30 [PubMed PMID: 26539276]