Introduction
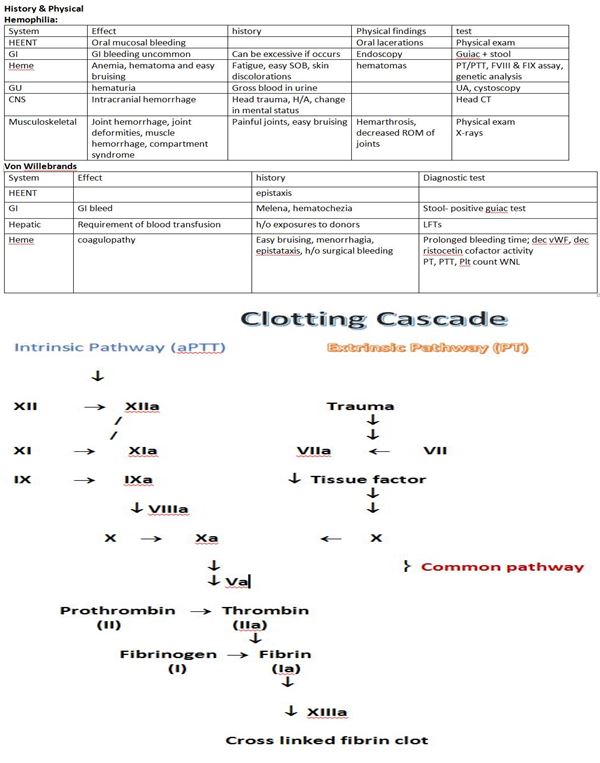
The body possesses innate mechanisms to control bleeding in the setting of an injury. An understanding of these basic physiologic processes is critical to aid in the identification and diagnosis of bleeding disorders. The hemostatic system is responsible for maintaining blood in a fluid state, free of the aggregation of platelets and thrombus formation with the help of prostacyclin, antithrombin III and nitric oxide within the endothelial cells. These naturally occurring substances found in the blood assist in the prevention of clots by causing conversion of plasminogen to plasmin to promote fibrinolysis. Damage or injury to the endothelium will initiate a cascade of events in an attempt to control bleeding. Disruption of the endothelium will first cause local vasoconstriction to occur, limiting blood flow to the area. Primary hemostasis initiates by platelets with the release of von Willebrand factor (vWF), a large plasma glycoprotein made and stored in endothelial cells and megakaryocytes. Platelets and vWF will combine to form a plug at the site of injury. Circulating vWF continues to bind with collagen and Factor VIII as well as other endothelial substances, allowing the platelet plug to adhere to the area of injury.[1] Through activation of the clotting cascade (see image) and secondary hemostasis, this initial platelet plug will get reinforced to a sturdy fibrin clot. The clotting cascade operates through a dual process system in which the various clotting factors become activated with the result being the formation of a fibrin strand or clot at the site of tissue injury. A deficiency of any of the essential clotting factors will result in difficulty forming a fibrin clot, and excessive bleeding can occur.
Bleeding disorders fall into two main categories: inherited and acquired. Inherited bleeding disorders have a genetic predisposition and involve a deficiency of coagulation factors. Acquired bleeding disorders can be caused by conditions that an individual may develop at any point during their lifetime. These can be broader in range and dependent on comorbid conditions. The focus of this discussion will be on congenital coagulopathies; acquired bleeding disorders will be considered to be outside the scope of the information presented here.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Hemophilia, an x-linked heredity disorder, is diagnosed by an abnormal concentration of Factor VIII or IX. Approximately one-third of cases arise from a spontaneous mutation. Von Willebrand disease, with an autosomal dominant inheritance pattern, has variable penetrance and clinical symptoms can vary from person to person. The most severe pathology occurs in homozygotes.[2] Neither bleeding disorder has a predilection for a specific race.
Epidemiology
Hereditary bleeding disorders are due to the absence or deficiency of specific clotting proteins which act as procoagulants through precise interactions in the clotting cascade. The three most common are hemophilia A (Factor VIII deficiency), hemophilia B (Factor IX deficiency) and von Willebrand disease. Hemophilia A is an X-linked recessive genetic disorder affecting 1 in 5000 males making it the most common congenital coagulopathy. Hemophilia B is an X-linked genetic coagulopathy affecting 1 in 30000 male births. Hemophilia B is also known as Christmas disease. The origin of its namesake is from Steven Christmas, the first patient diagnosed with Hemophilia B in 1952. Since hemophilia is genetic, its prevalence increases in populations in which higher levels of consanguinity exists. Females may be asymptomatic carriers of the hemophilia gene or may be found to have a partial deficiency of the specific factors involved. Von Willebrand disease is an autosomal dominant trait with no predilection for sex; however, women are more likely to exhibit symptoms as a result of increased bleeding during menstruation.[3] Von Willebrand disease was first described in 1926 by Finnish physician Erik Adolf von Willebrand. According to the CDC, von Willebrand disease affects approximately 1% of the general population.[4]
Pathophysiology
Bleeding disorders may present in correlation with their severity, and some may be undetected until a major trauma or surgery occur. Patients with a severe form of hemophilia In hemophilia, categorized as less than 1% of normal plasma levels, will often present with 20 to 30 episodes of epistaxis a year, excessive bleeding after minor traumas or into muscles and joints (hemarthrosis). Diagnosis usually occurs within the first two years of life and can be immediately evident after circumcision. Newborns can also present with intracranial hemorrhages, cephalohematoma or umbilical cord bleeding immediately following delivery.[5] Those with a more moderate form of the disease (6 to 30% of normal levels) may only bleed excessively after surgery or a major trauma.
Von Willebrand factor (vWF) is a glycoprotein produced in endothelial cells and megakaryocytes that is responsible for facilitating platelet binding after injury of the endothelial surface occurs. Von Willebrand disease is a common congenital bleeding disorder in which there is a deficiency or dysfunction of vWF. Factor VIII levels can be affected as well. The disease presents similarly to that of a platelet abnormality and can exhibit variable clinical symptomatology from mild mucocutaneous bleeding of the nose or gingiva or menorrhagia to hemarthrosis in more severe cases. The disease categorized into three types. Type I is the most common, representing 60 to 80% of cases. Type 1 von Willebrand disease is a heterozygous deficiency in which there may be only 20% to 40% of normal levels of vWF in addition to a reduction in Factor VIII levels. Patients with Type I von Willebrand disease can present with mild clinical symptoms like a propensity for easy bruising, mucosal bleeding or menorrhagia.[6] Medications which inhibit prostaglandin and thromboxane synthesis may significantly exacerbate symptoms and can often aid in initial diagnosis.[7] Type 2 von Willebrand disease is less common, representing approximately 17% of the reported cases, and is characterized by a qualitatively abnormal vWF which can also be associated with thrombocytopenia and decreased Factor VIII. There are four distinct subtypes within the Type 2 category. Type 2A lacks a normal vWF multimer because of abnormal proteolysis or reduced secretion of the factor. Type 2B is a mutation which causes the vWF to be hyperactive and have an increased binding affinity to platelets causing the creation of complexes which are quickly cleared from the circulation, ultimately resulting in thrombocytopenia.[8] Type 2M possesses a decreased platelet binding ability to vWF with depleted factor levels, and Type 2N exhibits a decrease in binding of vWF to Factor VIII. Type 3 is the rarest and the most severe form of the disease representing approximately 3% of the cases, where there are markedly diminished levels of vWF and FVIII.
History and Physical
Hemophilia:
While mild hemophilia may only present after a traumatic injury or surgery, those with a moderate to severe form of the disease may exhibit hallmark characteristics such as mucosal or gingival bleeding, easy bruising, and hematoma formation. The concern is when there is bleeding into joints, particularly in the ankles, knees, and elbows, referred to as hemarthrosis. Hemarthrosis can initiate an inflammatory process to occur in which the joints become painfully swollen and eventually limit motion.[9] There is potential for the perpetuation of a vicious cycle whereby the joints are damaged resulting in synovitis, and an area for subsequent bleeding can occur. Over time hemophilic arthropathy occurs with joint narrowing, bone cysts and a decreased range of motion. Bleeding into muscle tissue from minor traumas can result in anemia and compression of vital structures and nerves leading to compartment syndrome. Bleeding less frequently occurs in the urinary and gastrointestinal tracts. These patients are at significant risk of intracranial bleeds which would be a life-threatening emergency. Hemophilia can present in infancy with cephalohematoma formation after vaginal birth and with significant bleeding after circumcisions.
Von Willebrand Disease
Von Willebrand disease can exhibit clinical signs and symptoms starting in childhood with a history of easy bruising and bleeding. While patients with a very mild version of the disease may not have clinical symptoms at all, patients with vWF that is qualitative or quantitatively low may present with a predisposition to mucosal bleeding and episodic epistaxis. Women with von Willebrand disease may have significant menorrhagia which is often a presenting sign of the illness, precipitating a workup and eventual diagnosis.[10] These patients can also go unrecognized until undergoing major surgery or experiencing a traumatic injury.
Evaluation
Laboratory Evaluation for Bleeding Disorders
Laboratory testing is essential for diagnosing bleeding disorders. However, the specific panels necessary for an accurate diagnostic evaluation are not standardized and may vary significantly between hospitals and regions. Routine laboratory analysis for clotting disorders starts with platelet count, prothrombin time (PT), partial thromboplastin time (aPTT), the international normalized ratio (INR) and bleeding time. The platelet count should not only have a sufficient quantity (normal = 150000 to 500000/ml) but must also be functional. The bleeding time assesses the function of the platelets. Bleeding times can be delayed in a patient with vWF deficiency or from specific medications that interfere with platelet function (NSAIDS, aspirin and valproic acid). PT (normal = 11.5 to 14s) represents the function of coagulation factors II, V, VII, and X which are the hepatically synthesized vitamin K dependent factors. The PT and INR will be affected by patients taking warfarin as it interferes with the synthesis of vitamin K dependent factors. The INR (normal= 0.8 to 1.2) is a ratio that is used to estimate the percent of functional clotting factors. For example, an INR of between 2 to 3 correlates approximately to 10% of active clotting factors present. It is necessary to have at least 30% of the clotting factors present for normal coagulation. Partial thromboplastin time (normal = 25 to 40s) measures the efficacy of von Willebrand Factor and factors VIII, IX, XI, and XII.[11]
Hemophiliacs will have an elevated aPTT and a normal PT/INR, bleeding time and platelet count. The aPTT, a measure of the intrinsic pathway, will be elevated as a result of low levels of FVIII. An elevated aPTT should prompt investigation by looking at individual factor levels, specifically Factor VIII and IX.[12] When evaluating specific factor levels, the amount of factor present will determine the severity of the disease. When the diagnosis is suspected, emphasis must also focus on family history including maternal male family members.
Diagnosis of von Willebrand disease is represented by increased bleeding time and a decrease in vWF levels as measured by the ristocetin cofactor collagen binding, in addition to a history of bleeding and positive family history of von Willebrand disease. The reocmmendation is that patients are tested at least three times before making the official diagnosis as vWF levels are subject to fluctuate, changing with stress, pregnancy, exercise, and inflammatory processes. There are also some subtle differences in vWF levels based on gender and blood type.[13] Von Willebrand disease requires factor multimer assays to diagnose the specific subtype of the disease. Additionally, the aPTT may be mildly elevated in approximately 50% of patients with von Willebrand disease second to low levels of factor VIII.
Treatment / Management
The mainstay treatment of hemophilia is factor replacement, either prophylactically or need-based. Recombinant-derived Factor VIII and IX concentrates are available and prevent the risk of viral transmission.[14] Recombinant Factor VIII increases the plasma concentration by 2% for every 1 IU/kg, and recombinant factor IX produces an increase of 0.8% for every 1IU/kg given. The goals of correction are to achieve a 50% plasma value for the management of bleeding risks such as surgery and 100% correction in the setting of major trauma. These levels should be obtained 30 minutes before the onset of surgery and maintained for 2 to 7 days after surgery. The timing of subsequent doses is determined based on factor half-life which is typically 8 to 12 hours.(B2)
The treatment of von Willebrand disease consists of desmopressin (DDAVP) or cryoprecipitate. DDAVP will enhance the release of vWF in patients with Type 1 von Willebrand disease. DDAVP is a synthetic derivative of antidiuretic hormone that acts on type 2 vasopressin receptors. It works by stimulating the release of vWF from endothelial cells by way of signaling through the cyclic adenosine monophosphate pathway which prompts the release of Weibel-Palade bodies into the endothelial cells and eventually into the plasma.[15] Additionally, DDAVP works on the renal collecting duct as an anti-diuretic. It reduces the amount of water that is eliminated in the urine potentially causing dilutional hyponatremia; therefore, patients should have fluid restriction maintained while receiving this medication.[16] DDAVP administered intravenously (0.3mcg/kg) will increase plasma Factor VIII and VWF levels by 3 to 5 times their baseline within 30 to 60 minutes after administration. DDAVP can also be administered subcutaneously (0.3 mcg/kg) or at fixed intranasal doses which is convenient for prophylactic treatment at home. DDAVP administration is expected to raise levels to 30 to 50% in patients with a baseline of 10% factor activity which may be sufficient for low-risk procedures but may require further supplementation to increase vWF to adequate levels needed for trauma or major surgery. Patients with a baseline of 20% factor level receiving DDAVP can see levels rise to 60 to 100% which would be suitable for most surgical procedures. Approximately 10% of patients within the Type 1 category may fail to respond to DDAVP; therefore, the recommendation is that patients undergo a trial of DDAVP administration at diagnosis or before its clinical need. Patients with Type 2 and 3 von Willebrand disease typically require replacement products consisting of Factor VIII and vWF. It is also important to note that patients with Type 2a and 3 will not respond to DDAVP as the former possesses dysfunctional vWF and Type 3 lacks releasable stores of vWF. Type 2b should never be given DDAVP, as it is contraindicated due to its potential thrombogenicity.[17](A1)
Replacement Products
- There is a human plasma-derived concentrate of Factor VIII with an even higher concentration of vWF. This product has been the subject of extensive study and deemed to be the safest option for factor replacement as it has undergone a pasteurization process to inactivate any blood-borne viruses. It has approval from the Food and Drug Administration (FDA) for the treatment and prevention of bleeding disorders in adult patients with Hemophilia A, as well as adult and pediatric patients with von Willebrand disease.[18] (B2)
Factor VIII replacement with human plasma-derived concentrate of Factor VIII requires a simple weight-based calculation. The patient’s weight (in kg) is multiplied by the desired percent level of Factor VIII, assuming that starting levels are 0. That number then gets multiplied by the volume of distribution, which is approximately 0.5.[19] Thus, the dose of human plasma-derived concentrate of Factor VIII = weight in kg x desired Factor VIII level x 0.5. For a 60kg female, with a target goal of 50% Factor VIII level: 60 x 50 x 0.5 = 1500 units of Factor VIII.
Alphanate is another commercially available, virally inactivated product with Factor VIII and ristocetin cofactor activity essential for vWF support. The FDA has approved its use for both adults and children with Hemophilia A or von Willebrand disease who require treatment or prevention of spontaneous or trauma-related bleeding, including surgery.
- Factor IX concentrate is a commercially available product and has been subject to various purification techniques to eliminate the risk of viral transmission during its administration. These products have FDA approval for use in the setting of prevention and control of bleeding in patients with a factor IX deficiency.[20]. Dosing of Factor IX concentrate = weight in kg x desired factor level x volume of distribution (which is 1 for Factor IX). For a 60kg female with a target goal of 100% Factor IX level: 60 x 100 x 1 = 6000 units.
Allogenic Replacement Therapy
- Fresh frozen plasma (FFP) contains Factor VIII and vWF, but large volumes are needed to obtain adequate factor levels (20 to 25mL/kg).
- Cryoprecipitate is a human plasma-derived product containing high levels of Factor VIII, vWF and fibrinogen (Factor I). It comes packaged in small volumes, so multiple bags are often required to obtain the adequate level of the factor desired. Virus inactivation is not routinely applied to these products therefore virally inactivated replacement products are considered a safer alternative to FFP and cryoprecipitate. The absence of factor IX in cryoprecipitate negates its use in Hemophilia B.
- Platelet transfusions are necessary when bleeding continues despite normal Factor VIII levels. Platelets can transport and localize the vWF from the site of the vascular injury.
Antifibrinolytic Acid Therapy
- Aminocaproic acid is a synthetic analog of lysine used to control or prevent hemorrhage. It competitively reduces the conversion of plasminogen to plasmin thereby inhibiting fibrinolysis and promoting clot formation. It is typically administered as an intravenous infusion during a surgical procedure but is also available in an oral form for home use in patients with bleeding disorders. It is available as a mouthwash or a tablet for oral bleeding, recurrent epistaxis or menorrhagia. This agent is FDA approved in the treatment of patients with bleeding disorders and is often useful as an adjunct therapy in patients with coagulopathic potential.
- Tranexamic acid is a synthetic medication made from lysine which acts by competitively inhibiting plasminogen activation and is considered more potent than aminocaproic acid. At higher concentrations, it can act as a non-competitive inhibitor of plasmin. It has ten times the potency of aminocaproic acid and is FDA approved for use in patients with bleeding disorders. It is available in intravenous and oral formulations. The oral preparation can also help in the treatment of recurrent minor bleeding issues that occur at home and in preparation for dental work.[21] (A1)
Hormonal Treatments
Oral contraceptives such as oral progestins and depot medroxyprogesterone have been shown to be effective in women with Type 1 von Willebrand disease with menorrhagia by significantly elevating circulating vWF levels. While the exact mechanism of estrogens influence on vWF is not entirely understood, it is hypothesized to occur as a result of its lipophilic nature, allowing it to penetrate the cytoplasm of the nuclear receptors thereby increasing gene transcription of the various clotting proteins.[22]
Differential Diagnosis
- Malignancy
- Severe liver failure
- Thrombocytopenia
- Vitamin K deficiency
- Antithrombin III deficiency
- Massive transfusion
- Disseminated intravascular coagulation
- Lupus anticoagulant
- Protein C deficiency
- Protein S deficiency
- Idiopathic thrombocytopenic purpura (ITP)
- Medication side effects
Prognosis
Patients living with congenital bleeding disorders can expect to live full, productive lives with appropriate medical treatment, education and a management plan in case of trauma or surgery. Patients should consider wearing a medical identification bracelet so that they can receive proper management in case they are involved in significant trauma or are unable to communicate their medical history verbally.
Enhancing Healthcare Team Outcomes
The World Bleeding Disorder Registry (WBDR) comprises a record of patients with bleeding disorders who receive care through the Hemophilia Treatment Centers throughout the world who have voluntarily allowed their identities and private healthcare information to be entered into a web-based platform. This global data collection aids the advancement of understanding the disease through evidence-based advocacy initiatives. The WBDR is the only global registry of people with bleeding disorders around the world. The accessibility of the information collected in this database strengthens the ability to diagnose and treat people with hemophilia.[23] Hematology nurses, internists, and hematologists should be familiar with the WBDR as it provides access to patient data online.
The management and treatment of bleeding disorders require the collaborative efforts of an interprofessional health team that includes physicians, specialists, specialty-trained nurses, and pharmacists, all working and communicating across disciplines to bring about the most effective treatment and outcomes. [Level V]
Media
References
Méndez Rojano R, Mendez S, Lucor D, Ranc A, Giansily-Blaizot M, Schved JF, Nicoud F. Kinetics of the coagulation cascade including the contact activation system: sensitivity analysis and model reduction. Biomechanics and modeling in mechanobiology. 2019 Aug:18(4):1139-1153. doi: 10.1007/s10237-019-01134-4. Epub 2019 Mar 21 [PubMed PMID: 30900051]
Sultan Y, Caen J, Bernard J. [Demonstration of recessive transmission in Willebrands diseases. Detection of heterozygotes]. Comptes rendus hebdomadaires des seances de l'Academie des sciences. Serie D: Sciences naturelles. 1974 Sep 23:279(13):1139-42 [PubMed PMID: 4219324]
Edlund M. [Menorrhagia--a symptom not sufficiently surveyed. The path to diagnosis and treatment lined with ambiguity and misunderstandings]. Lakartidningen. 2001 Nov 28:98(48):5505-6, 5509-10 [PubMed PMID: 11769366]
Level 3 (low-level) evidenceKurth AA, Ludwig G, Scharrer I. [Prevalence, pathophysiology, diagnosis and treatment of von Willebrand syndrome in orthopedic trauma patients]. Der Orthopade. 1999 Apr:28(4):366-74 [PubMed PMID: 10335531]
Level 3 (low-level) evidenceBertamino M, Riccardi F, Banov L, Svahn J, Molinari AC. Hemophilia Care in the Pediatric Age. Journal of clinical medicine. 2017 May 19:6(5):. doi: 10.3390/jcm6050054. Epub 2017 May 19 [PubMed PMID: 28534860]
Sholzberg M, Teitel J, Hicks LK. A 24-year-old woman with heavy menstrual bleeding. CMAJ : Canadian Medical Association journal = journal de l'Association medicale canadienne. 2017 Jun 5:189(22):E779-E780. doi: 10.1503/cmaj.161469. Epub [PubMed PMID: 28584042]
Moon LM, Perez-Milicua G, Dietrich JE. Evaluation and management of heavy menstrual bleeding in adolescents. Current opinion in obstetrics & gynecology. 2017 Oct:29(5):328-336. doi: 10.1097/GCO.0000000000000394. Epub [PubMed PMID: 28858896]
Level 3 (low-level) evidenceKaraman K, Akbayram S, Garipardıç M, Öner AF. Diagnostic evaluation of our patients with hemophilia A: 17-year experience. Turk pediatri arsivi. 2015 Jun:50(2):96-101. doi: 10.5152/tpa.2015.2516. Epub 2015 Jun 1 [PubMed PMID: 26265893]
Yoo MC, Jeong BO, Ahn J. Anterior osteophyte resection of the ankle joint to increase range of motion in haemophilic ankle arthropathy. Haemophilia : the official journal of the World Federation of Hemophilia. 2019 May:25(3):e159-e164. doi: 10.1111/hae.13719. Epub 2019 Mar 13 [PubMed PMID: 30866148]
Demers C, Derzko C, David M, Douglas J. No. 163-Gynaecological and Obstetric Management of Women With Inherited Bleeding Disorders. Journal of obstetrics and gynaecology Canada : JOGC = Journal d'obstetrique et gynecologie du Canada : JOGC. 2018 Feb:40(2):e91-e103. doi: 10.1016/j.jogc.2017.11.036. Epub [PubMed PMID: 29447730]
Level 2 (mid-level) evidenceNeutze D, Roque J. Clinical Evaluation of Bleeding and Bruising in Primary Care. American family physician. 2016 Feb 15:93(4):279-86 [PubMed PMID: 26926815]
Jain S, Acharya SS. Management of rare coagulation disorders in 2018. Transfusion and apheresis science : official journal of the World Apheresis Association : official journal of the European Society for Haemapheresis. 2018 Dec:57(6):705-712. doi: 10.1016/j.transci.2018.10.009. Epub 2018 Oct 30 [PubMed PMID: 30392819]
Saif MA, Thachil J, Brown R, Bigger BW, Wynn RF, Nash M, Hay CR. Is it congenital or acquired von Willebrands disease? Haemophilia : the official journal of the World Federation of Hemophilia. 2015 Jan:21(1):e113-5. doi: 10.1111/hae.12588. Epub 2014 Nov 7 [PubMed PMID: 25381916]
Level 3 (low-level) evidenceAnzengruber J, Lubich C, Prenninger T, Gringeri A, Scheiflinger F, Reipert BM, Malisauskas M. Comparative analysis of marketed factor VIII products: recombinant products are not alike vis-a-vis soluble protein aggregates and subvisible particles. Journal of thrombosis and haemostasis : JTH. 2018 Jun:16(6):1176-1181. doi: 10.1111/jth.14125. Epub 2018 May 11 [PubMed PMID: 29665242]
Level 2 (mid-level) evidenceGuddati AK, Rosovsky RP, Van Cott EM, Kuter DJ. Quantitative analysis of desmopressin (DDAVP) response in adult patients with type 1 von Willebrand disease. International journal of laboratory hematology. 2019 Jun:41(3):325-330. doi: 10.1111/ijlh.12978. Epub 2019 Feb 8 [PubMed PMID: 30735311]
Barinsky GL,Buziashvili D,Svider PF,Carron MA,Folbe AJ,Hsueh WD,Eloy JA,Johnson AP, Perioperative Desmopressin for Patients Undergoing Otolaryngologic Procedures: A Systematic Review. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2019 Jul [PubMed PMID: 30857487]
Level 1 (high-level) evidenceKruse-Jarres R, Johnsen JM. How I treat type 2B von Willebrand disease. Blood. 2018 Mar 22:131(12):1292-1300. doi: 10.1182/blood-2017-06-742692. Epub 2018 Jan 29 [PubMed PMID: 29378695]
Miesbach W, Krekeler S, Wolf Z, Seifried E. Clinical use of Haemate® P in von Willebrand disease: a 25-year retrospective observational study. Thrombosis research. 2015 Mar:135(3):479-84. doi: 10.1016/j.thromres.2014.12.017. Epub 2014 Dec 27 [PubMed PMID: 25595881]
Level 2 (mid-level) evidenceOckelford PA,Lowe G,Johns AS,Berry EW, Comparison of methods of plasma volume determination for dose calculation of factor VIII in patients with classic haemophilia. The New Zealand medical journal. 1986 Feb 26 [PubMed PMID: 3081842]
Bar-Natan M, Hymes KB. Management of Intraoperative Coagulopathy. Neurosurgery clinics of North America. 2018 Oct:29(4):557-565. doi: 10.1016/j.nec.2018.06.007. Epub [PubMed PMID: 30223968]
Engelen ET, Schutgens RE, Mauser-Bunschoten EP, van Es RJ, van Galen KP. Antifibrinolytic therapy for preventing oral bleeding in people on anticoagulants undergoing minor oral surgery or dental extractions. The Cochrane database of systematic reviews. 2018 Jul 2:7(7):CD012293. doi: 10.1002/14651858.CD012293.pub2. Epub 2018 Jul 2 [PubMed PMID: 29963686]
Level 1 (high-level) evidenceAsensio JA,Cáceres ARR,Pelegrina LT,Sanhueza MLÁ,Scotti L,Parborell F,Laconi MR, Allopregnanolone alters follicular and luteal dynamics during the estrous cycle. Reproductive biology and endocrinology : RB [PubMed PMID: 29636114]
Hamilton A, Ozelo M, Leggo J, Notley C, Brown H, Frontroth JP, Angelillo-Scherrer A, Baghaei F, Enayat SM, Favaloro E, Lillicrap D, Othman M. Frequency of platelet type versus type 2B von Willebrand disease. An international registry-based study. Thrombosis and haemostasis. 2011 Mar:105(3):501-8. doi: 10.1160/TH10-08-0523. Epub 2011 Feb 8 [PubMed PMID: 21301777]