Introduction
Blepharoplasty is the general term for correcting defects, deformities, and disfigurations of the eyelids either for functional reasons, cosmetic reasons, or both. The most common reason is cosmetic in which excess skin and fat are removed and or repositioned to give a more pleasing appearance. In many cases, the upper eyelids are droopy or ptotic, and a ptosis procedure is combined with upper eyelid blepharoplasty. In the combined procedure the levator aponeurosis is repositioned on the tarsal plate, and the upper eyelid height is titrated. Once the upper eyelid height is set, excess skin and fat are removed to give a more youthful appearance. However, upper blepharoplasty may also be indicated for functional reasons, whereby the upper eyelid fat, orbicularis hypertrophy or laxity, skin laxity and lash ptosis may affect the patient's field of vision. The etiology of upper eyelid ptosis in most cases is levator dehiscence due to age. [1][2]However infections, trauma, tumors or inflammation can cause dehiscence as well. Other less common causes of ptosis of the upper eyelid include myasthenia gravis, trauma, orbital or eyelid tumors, congenital ptosis, third never palsy or Horner syndrome. It is important to evaluate the patient to ensure that dehiscence of the levator is the cause of the ptosis before attempting a repair. If there is minimal levator function (less than 4 mm), advancing the levator will not give adequate lift, and a frontalis sling technique is used to elevate the eyelid.
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
The layers of the upper eyelid start, going from outer to inner, skin, orbicularis, orbital septum, pre-aponeurotic fat pads, levator aponeurosis, Muller's muscle tarsal plate, and conjunctiva. Pre-aponeurotic fat has been referred to as a surgeon's only friend in the upper eyelids since it lies immediately anterior to the levator aponeurosis. As long as the surgeon stays anterior to the fat pads, he or she cannot damage the levator muscle.
Indications
Ptosis surgery is indicated when there is visual compromise due to ptotic upper eyelids. The patient will frequently complain of loss of peripheral vision or look through their eyelashes. [3][4][5]They may state that visual acuity improves when they physically lift their eyelids with their fingers or forehead muscle. Excess skin can cause the same problems as the skin can hang over the eyelid margin and obscure vision like a window shade. Surgeons can document the loss of visual field by doing perimetry. Insurance may cover the repair if the physician submits proof of visual field loss due to a ptotic upper eyelid or excess upper eyelid skin.
Contraindications
Most contraindications for ptosis surgery revolve around the exposure of the cornea. Conditions like thyroid orbitopathy, progressive external ophthalmoplegia, or loss of Bell's phenomenon can make patients more prone to exposure keratopathy after ptosis surgery: a more conservative approach is needed in these patients. A complete evaluation of dry eye is essential to estimate the risk of dry eye symptoms progressing after surgery. If myasthenia gravis is suspected, patients need a workup including acetylcholine receptor antibodies and or a tensilon test. If myasthenia is diagnosed a trial of Mestinon is indicated before ptosis surgery. It is important to perform a complete workup before ptosis repair to rule out other cause of ptosis or possible risk factors. CT scan of the orbits should be obtained if an orbital process such as thyroid orbitopathy or an orbital tumor is suspected. Slit lamp evaluation is essential to detect corneal erosions or dry eye.
Personnel
Blepharoplasty/ptosis surgery can be done with a scrub tech and a circulating nurse. A nurse anesthetist should be in the room with an anesthesiologist. Monitoring the patient at all times is essential for safety.
Preparation
Preoperative workup is essential to ensure that the cause of the ptosis is levator-induced and that levator function is adequate to resolve the ptosis with a levator advancement. Rule out tumors, myasthenia, and severe dry eye conditions before surgery.
Technique or Treatment
The patient should always be re-examined immediately prior to surgery. It is also important to make eyelid markings with the patient sitting up so that the appropriate position of the brows may be determined and compensated for as needed. The patient's natural skin crease is marked. When a blepharoplasty is performed with or without concurrent ptosis repair, the relative amount of skin to be removed is marked with a lateral rise to the upper eyelid skin crease marking.[6][7][8][9][10]
Once in the operating room, the patient is sedated; however, general anesthesia is avoided since the patient's cooperation is needed to set the eyelid height. A combination of Xylocaine, marcaine and hyaluronidase with epinephrine is used in the block, and about 2 mL are injected subcutaneously anterior to orbital septum. The patient's entire face is then prepped and draped in the usual fashion. The incision is made with a 15 blade along the entire length of the upper eyelid and hemostasis is obtained. Dissection is taken down through orbicularis muscle until the orbital septum is located. A variable amount of orbicularis oculi muscle may need to be removed, depending upon the patient's age, the degree of orbicularis hypertrophy or laxity. Slight pressure on the globe will cause the preaponeurotic fat to prolapse and be visible just deep to the orbital septum. The septum is incised with a Westcott scissor and opened along the entire length of the upper eyelid keeping the fat pads in front of the levator. The fat pads are then gently dissected off underlying levator aponeurosis. Dissection is then taken inferiorly to expose the tarsal plate by dissecting pre tarsal orbicularis off of the tarsal plate. Everting the eyelid can help identify the tarsus. Once the tarsus is exposed, a double-armed 6-0 non-absorbable monofilament surgical suture is placed in the tarsus centrally 2 mm below the superior edge. The needle should only go halfway through the tarsus, and the tarsus is picked up off the globe to avoid placing the needle through the cornea. Once in position, the eyelid is everted, and the posterior of the lid is observed to ensure the suture does not go all the way through the tarsal plate. Doing so would cause severe abrasions of the cornea. The 2 ends of the suture are then placed through the levator in a horizontal mattress fashion and tied with a single throw. The patient then sits up and is asked to open the eyes, and the lid height and contour are evaluated. Depending on height and contour, additional levator advancement may be needed, and additional stitches may be needed medial or lateral to the initial suture to obtain optimal height and contour. Once the lid height is satisfactory, the patient is placed back down, and the sutures are tied and trimmed. At this point, the patient's co-operation is not necessary, so if there is any discomfort the level of anesthesia can be deepened. Excess preaponeurotic fat is now excised taking care not to remove the lacrimal gland which is in the far lateral orbit and appears paler (and sometimes pink) than the preaponeurotic fat pads. The fat pads are excised by clamping them with a hemostat and excising with scissors although many surgeons excize the fat using an open-sky approach without clamping the fat in hemostats . The edge of the fat still in the clamp is cauterized with bipolar cautery. The edge of the fat is grasped with a forceps, and the clamp is removed. The edge of the cauterized fat is inspected for bleeding. If the lacrimal gland is prolapsed, it can be sutured back into the superior temporal orbit with a 5-0 resorbable suture. Excess skin is now pulled down over the wound and marked with a sterile marking pen and excised with Westcott scissors. Excess preseptal orbicularis is excised, and hemostasis is obtained. The wound is closed with interrupted 6-0 mild chromic sutures, and topical steroid/antibiotic ointment is placed over the wound. The eye is patched overnight and ice packs applied to the eye.
Complications
The most common complication is uneven or asymmetric eyelid height or poor contour and lid peaking. Another operation can usually resolve this. Orbital hemorrhage is the most devastating complication and can lead to blindness if not identified and treated immediately. If the hemorrhage is severe enough, it can cause compressive optic neuropathy and lead to blindness. Opening the wound and draining blood will resolve the problem but it needs to be identified quickly. The patients will complain of significant pain, and if this is the case, the patient needs to be evaluated immediately. If a hemorrhage has occurred and the intraocular pressure is significantly elevated the wound needs to be opened immediately and excess blood drained before compression of the optic nerve causes permanent damage. Postoperative infections are rare although it is possible to develop orbital cellulitis since the orbital septum is opened during surgery. Infections are treated with heat and the appropriate systemic antibiotics. Chances of getting an infection may be reduced by irrigating the operative site with bass solution impregnated with 40 mg of intravenous (IV) gentamycin.
Clinical Significance
Patients benefit cosmetically and functionally from combined ptosis/blepharoplasty. The lids are elevated to their normal position allowing better peripheral vision and the eyes are given a refreshed more youthful appearance.
Enhancing Healthcare Team Outcomes
Blepharoplasty is performed for functional and cosmetic reasons but is generally performed by the ophthalmologist and the plastic surgeon. The follow up of these patients is with the primary care provider and nurse practitioner. While blepharoplasty appears to be a minor procedure, if attention is not paid to detail it can lead to serious complications ranging from asymmetrical eyelid height or poor contour, lid peaking, Orbital hemorrhage, infection and injury to the eye structures. In general, the outcomes for patients undergoing blepharoplasty are good but the surgery is not durable and minor touchups may be required in future. [11][12][13](Level V)
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
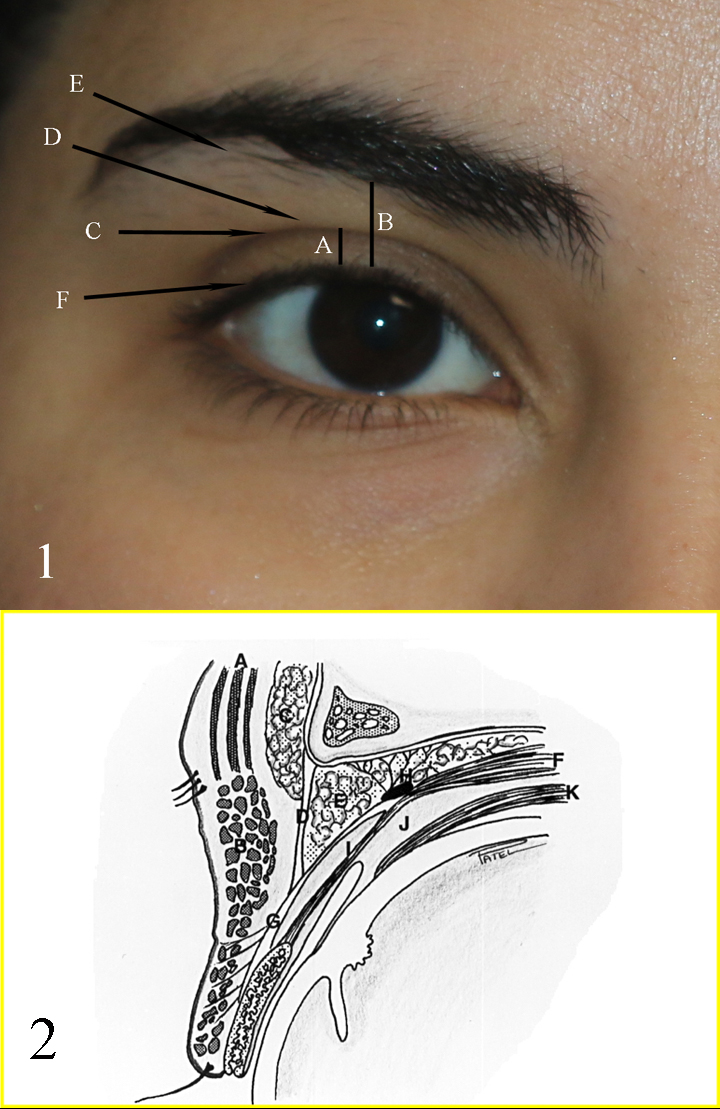
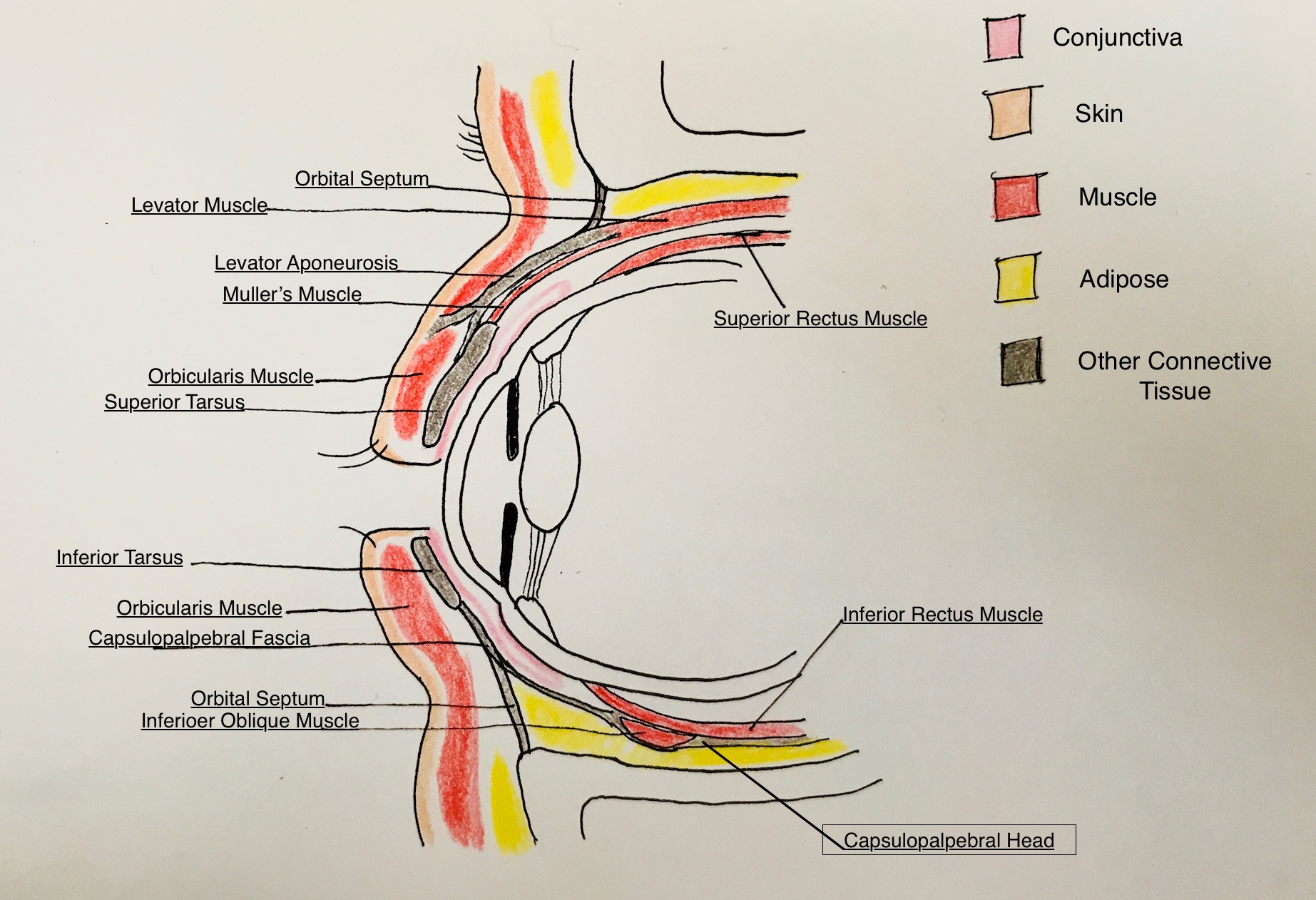
Fig 1: A: upper eyelid platform; B: Brow to Lid margin distance; C: Upper eyelid crease; D: Upper eyelid fold; E: Brow fatpad; F: Eyelid margin and eyelash curve Fig 2: A: Frontalis muscle; B: Orbicularis muscle; C: Brow fat pad; D: Orbital septum; E: Preaponeurotic fat pads; F: Levator muscle; G: Levator aponeurosis; H: Whitnall ligament; I: Muller muscle; J: Common sheath; K: Superior rectus muscle Contributed by Professor Bhupendra C. K. Patel MD, FRCS
(Click Video to Play)
References
Weaver DT. Current management of childhood ptosis. Current opinion in ophthalmology. 2018 Sep:29(5):395-400. doi: 10.1097/ICU.0000000000000508. Epub [PubMed PMID: 30096088]
Level 3 (low-level) evidenceLiu CY, Chhadva P, Setabutr P. Blepharoptosis repair. Current opinion in otolaryngology & head and neck surgery. 2018 Aug:26(4):221-226. doi: 10.1097/MOO.0000000000000463. Epub [PubMed PMID: 29746305]
Level 3 (low-level) evidenceKim MJ, Oh TS. Treatment for ophthalmic paralysis: functional and aesthetic optimization. Archives of craniofacial surgery. 2019 Feb:20(1):3-9. doi: 10.7181/acfs.2019.00066. Epub 2019 Feb 20 [PubMed PMID: 30840813]
Kokubo K, Katori N, Hayashi K, Sugawara J, Kou S, Fujii A, Kitamura S, Ninomiya R, Maegawa J. Evaluation of the eyebrow position after aponeurosis advancement. Journal of plastic surgery and hand surgery. 2019 Feb:53(1):60-64. doi: 10.1080/2000656X.2018.1547735. Epub 2019 Jan 24 [PubMed PMID: 30676851]
Chung YH, Kang SY, Choi WS. A case of intramuscular xanthelasma palpebrarum found during blepharoplasty. Archives of craniofacial surgery. 2018 Dec:19(4):296-299. doi: 10.7181/acfs.2018.02068. Epub 2018 Dec 27 [PubMed PMID: 30613094]
Level 3 (low-level) evidenceGildener-Leapman JR, Sheps I, Stein R, Benyamini O, Milstein A, Hartstein ME. The Sutureless Mullerectomy. Ophthalmic plastic and reconstructive surgery. 2019 May/Jun:35(3):290-293. doi: 10.1097/IOP.0000000000001331. Epub [PubMed PMID: 30844915]
Kokubo K, Katori N, Hayashi K, Sugawara J, Kou S, Fujii A, Haga S, Maegawa J. Evaluation of the eyebrow position after external Müller's muscle tucking: A new technique for ptosis repair. Journal of plastic, reconstructive & aesthetic surgery : JPRAS. 2019 Apr:72(4):662-668. doi: 10.1016/j.bjps.2019.01.010. Epub 2019 Jan 14 [PubMed PMID: 30772203]
Hwang I, Myung Y, Park S. Levator Pull-Out Suture Technique for Immediate Postoperative Correction of Eyelid Asymmetry After Ptosis Surgery in Asians. Aesthetic plastic surgery. 2019 Apr:43(2):388-394. doi: 10.1007/s00266-018-1276-x. Epub 2018 Nov 27 [PubMed PMID: 30483936]
Jung GS. Modified Upper Blepharoplasty Using Combination of Incision and Nonincision Surgical Approaches. The Journal of craniofacial surgery. 2019 Jan:30(1):235-236. doi: 10.1097/SCS.0000000000004912. Epub [PubMed PMID: 30444788]
Guo S, Yang M, Zhou C, Lv W, Zhang J, Gu C, Fang X. Corrective Strategies for a Complex Deformity Caused by "European-Style Double Eyelid" Blepharoplasty in Asians. Aesthetic plastic surgery. 2019 Apr:43(2):395-403. doi: 10.1007/s00266-018-1262-3. Epub 2018 Nov 19 [PubMed PMID: 30456638]
Lee JY, Cho K, Choi DD, Park KA, Woo KI, Kim YD, Oh SY. Superior rectus muscle insertion injury following cosmetic upper lid blepharoplasty: a case report. BMC ophthalmology. 2018 Jul 31:18(1):187. doi: 10.1186/s12886-018-0867-2. Epub 2018 Jul 31 [PubMed PMID: 30064402]
Level 3 (low-level) evidenceKlingenstein A, Hintschich C. [Update on upper eyelid blepharoplasty]. Der Ophthalmologe : Zeitschrift der Deutschen Ophthalmologischen Gesellschaft. 2018 Apr:115(4):266-274. doi: 10.1007/s00347-018-0671-7. Epub [PubMed PMID: 29516158]
Lee TS, Wang L, Han R, Mourad M, Ducic Y. Options in Repositioning the Asymmetric Brow from Paralysis and Trauma. Facial plastic surgery : FPS. 2017 Dec:33(6):627-638. doi: 10.1055/s-0037-1607975. Epub 2017 Dec 1 [PubMed PMID: 29195244]