Introduction
The human retina is the most metabolically expensive tissue in the human body. Processing visual input in the retina requires high quantities of arterial blood and, subsequently, venous drainage.[1][2][3][4] The congregation of retinal venules forms the central retinal vein which flows into the cavernous sinus. The blockage of this venous drainage from the retina can be of 2 varieties: central retinal vein occlusion (CRVO) or branch retinal vein occlusion (BRVO).
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Branch retinal vein occlusion was first described by the German ophthalmologist Theodor von Leber in 1877. Since then, scientists have discovered that BRVO can have multiple underlying causes, including age, hypertension, diabetic retinopathy, or hypercoagulability.[5] Branch retinal vein occlusion can be subdivided into major BRVO (retinal vein occlusion) and macular BRVO (macular vein occlusion). Regardless of the underlying cause, BRVO refers to the obstruction of a branch of the retinal vein at an arteriovenous crossing.[5] This compression of the vein is thought to cause turbulent blood flow that leads to thrombus formation.[5] The quadrant of the retina most commonly affected is the superotemporal quadrant in 63% to 66% of eyes affected with BRVO. Inferotemporal retina involvement constitutes 22% to 43% of eyes affected with BRVO. Nasal involvement is rare and is usually asymptomatic until neovascularization causes vitreous hemorrhage.
Epidemiology
Retinal venous occlusion (RVO) is the second most common retinal vascular pathology after diabetic retinopathy.[6] The exact incidence of BRVO is difficult to gauge, given the frequent asymptomatic nature of BRVOs.[5] Nonetheless, the Blue Mountain Eye study found a 10-year cumulative risk of RVO to be 1.6%[7] in the United States while finding no predilection for gender or race. The Beaver Dam Eye Study found a 15-year cumulative risk of BRVO to be 1.8%, three times more than CRVO at 0.5%.[5][7] Risk factors for developing BRVO include increasing age or age over 70 years old, history of systemic arterial hypertension, history of smoking, or a history of glaucoma.[8] A pooled analysis of population-based studies from the United States and found BRVO to have a higher prevalence in Asians and Hispanics compared to Caucasians, although this was not statistically significant.[9] Developing BRVO in one eye increases the risk of BRVO in the fellow eye to 7% to 10%.[18][10]
Pathophysiology
The loss of vision in BRVO is caused by macular edema which can have multiple pathophysiologic mechanisms.[11] Patients with long-standing systemic arterial hypertension undergo retinal artery arteriosclerosis that results in thickening of the arterial wall clinically evident as “silver and copper” wiring appearance. Retinal arteries and veins share a common adventitial sheath; therefore, thickening of the arterial wall that can compress the retinal vein at a point where they cross resulting in turbulent blood flow and potential thrombus formation.[5] Japanese ophthalmologist Yoshizo Koyanagi was the first to associate the mechanical nature of BRVO and arteriovenous knicking in 1928. Another mechanism of BRVO is thrombus formation due to hypercoagulability secondary to increased acute phase reactants or other clotting disorders such as resistance to activated protein C, deficiency of Protein C and S, deficiency of antithrombin III, a genetic mutation in prothrombin gene, antiphospholipid antibodies, and hyperhomocysteinemia.[12]
Histopathology
Microscopic cross-section of the retinal vein will show a thickened, sclerotic vessel with a reduced diameter and reduced color saturation of the blood column.
Toxicokinetics
Theories suggest increased acute phase reactants can lead to thrombus formation and subsequent BRVO, with C-reactive protein and pentraxin-3 being the most likely substances. Prolonged retinal ischemia in concert with inflammation and vascular dysfunction leads to documented increases in VEGF mRNA which can result in deleterious effects such as increased capillary permeability and neovascularization.[12][11][13] Studies have reported elevated levels of aqueous and vitreous vascular endothelial growth factor (VEGF) and interleukin-6 (IL-6) in BRVO, with the levels of VEGF and IL-6, correlated to the severity of macular edema and the degree retinal ischemia.[14][15]
History and Physical
Branch retinal vein occlusion is often asymptomatic. However, it may present with sudden-onset of painless vision loss or visual field defect correlating to the area of perfusion of the obstructed vessels. It is important to document a history of systemic hypertension, smoking, glaucoma, diabetes, or other systemic diseases and risk factors. Evaluation of patients for hypercoagulability may be beneficial. If the occlusion does not occur at an arteriovenous crossing, the possibility of underlying retinochoroiditis or retinal vasculitis should be ruled out. In patients with suspected BRVO, the blood pressure should be obtained and documented. The patient should also undergo a complete physical examination and systemic vascular workup including carotid doppler and transesophageal echocardiogram to rule out cardiovascular causes of vision loss.
Evaluation
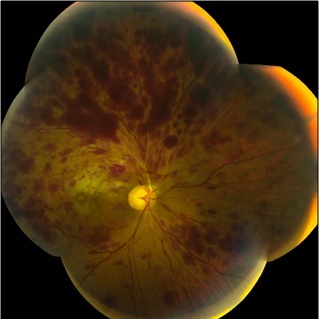
A complete dilated fundus examination including a slit lamp and indirect ophthalmoscopy exam to check for neovascularization should be performed. Optical coherence tomography (OCT) of the macula can also be used to check for macular edema. Early fundus features of BRVO on ophthalmoscopy include sectorial superficial retinal hemorrhages that rarely cross the horizontal raphe, cotton-wool spots, retinal edema, and dilated and tortuous retinal vein. Late features of BRVO on ophthalmoscopy include all of the signs mentioned above plus hard exudates, microaneurysms, sclerosed veins, telangiectatic vessels, collateral vascular shunt at the optic disc, narrowing and sheathing of the adjacent artery, vitreous hemorrhage, tractional retinal detachment, retinal neovascularization, optic disc neovascularization, and iris neovascularization.
Patients should have their fasting blood sugar, and hemoglobin A1C, lipid profile, complete blood count (CBC) with differential and platelets, PT/PTT, and ESR evaluated. It is appropriate to attain an intravenous (IV) fluorescein angiography after hemorrhage has cleared or sooner if neovascularization is suspected.
Treatment / Management
The treatment for BRVO is the prevention of the complications that cause vision loss and treatment of those complications, primarily macular edema and neovascularization. The systemic risk factors should be optimized in consultation with the patient's internist. The 2 general approaches to treating BRVO are pharmacologic management or surgical intervention. Pharmacologic management of BRVO involves intravitreal injections of anti-VEGF therapy and/or corticosteroids. For anti-VEGF injections, one study showed patients with BRVO who were injected monthly with either 0.5 or 0.3 mg of ranibizumab versus those receiving sham injections showed greater than 15% improvement in best-corrected visual acuity (BCVA) from baseline at 12 months.[16] The CRAVE study compared the efficacy between bevacizumab with ranibizumab and showed them to be equally as effective in substantially reducing macular edema after 6 months.[17] Intravitreal corticosteroid injections can have unwanted side-effects of cataract formation and intraocular pressure elevations. The GENEVA study was a randomized, sham-controlled trial which showed that a 0.7-mg dexamethasone intravitreal implant in the eye had a statistically significant improvement in vision versus sham controls.[18] Another study looked at the interval between onset of BRVO and initiating intravitreal dexamethasone injection and found that waiting 7 days has better efficacy in BRVO.[19] The SCORE study found intravitreal triamcinolone injections to be as effective as macular grid laser treatment, which is the current benchmark for BRVO treatment in cases of chronic macular edema with vision below 20/40 in the absence of macular capillary non-perfusion.(A1)
The Branch Vein Occlusion Study (BVOS) established macular laser treatment as the standard of care for BRVO.[8][17][20] The BVOS showed that patients whose foveal vasculature was still intact, and with vision between 20/40 to 20/200, had a 65% chance of gaining 2 lines of visual acuity and 37% of gaining 3 lines with laser treatment.[17][20] It is important to note that the BVOS study was conducted in the mid-1980s, and patients waited 3 months to allow macular edema to resolve before receiving laser treatment; whereas today pharmacologic treatments may commence immediately to bridge that gap. The Branch Vein Occlusion Study also looked at the efficacy of scatter photocoagulation in treating the formation of new vessels (neovascularization) and reducing the risk of vitreous hemorrhage and found that the risk of vitreous hemorrhage was reduced from 60% to 30%. When iris neovascularization occurs, which it does in about 2% of patients, scatter photocoagulation has been shown to be beneficial in reducing the risk of neovascular glaucoma. Pars plana vitrectomy may be indicated for eyes that develop non-clearing vitreous hemorrhage or retinal detachment.(A1)
Differential Diagnosis
Important differential diagnosis of BRVO includes diabetic retinopathy and hypertensive retinopathy. Diabetic retinopathy can be discerned from BRVO based on a few key features. Diabetic retinopathy is usually bilateral whereas BRVO is usually unilateral. Although both BRVO and diabetic retinopathy may present with dot blot hemorrhages and microaneurysms, only in diabetic retinopathy will extend across the horizontal raphe. Hypertensive retinopathy is the same; hemorrhages are not confined to a single sector, and the findings are usually bilateral.
Prognosis
Branch retinal vein occlusion typically has a good prognosis: 50% to 60% of eyes have a final visual acuity (VA) of 20/40 or better even without treatment. One important prognostic factor for final VA appears to be the initial VA. Also, the extent of macular or foveal involvement in acute BRVO is an important factor in determining the prognosis. Patients with retinal ischemia at least 5-disc diameters in size have 36% chances of developing neovascularization of the retina or optic disc. Patients with retinal ischemia at least 5-disc diameters in size have a 60% to 90% chance of developing vitreous hemorrhage if laser photocoagulation is not performed.[17][21]
Complications
The primary complication of concern regarding BRVO is neovascularization. Patients with large areas of non-perfusion were found to have an increased risk of neovascularization.[22][23]
Neovascularization of the iris occurs in 2% of patients. Patients may present with neovascularization may present with vitreous hemorrhage, floaters, loss of vision, retinal detachment, and glaucoma.[17][21]
Enhancing Healthcare Team Outcomes
Given that systemic disorders such as hypertension and coagulation defects can cause BRVO, it is recommended that patients follow up with their primary care physicians for systemic evaluation and treatment. More important patients should be encouraged to stop smoking, maintain a healthy weight. and keep the blood glucose levels under control.
Media
(Click Image to Enlarge)
References
Kaur C, Foulds WS, Ling EA. Hypoxia-ischemia and retinal ganglion cell damage. Clinical ophthalmology (Auckland, N.Z.). 2008 Dec:2(4):879-89 [PubMed PMID: 19668442]
Kergoat H, Hérard ME, Lemay M. RGC sensitivity to mild systemic hypoxia. Investigative ophthalmology & visual science. 2006 Dec:47(12):5423-7 [PubMed PMID: 17122132]
Harris AL. Hypoxia--a key regulatory factor in tumour growth. Nature reviews. Cancer. 2002 Jan:2(1):38-47 [PubMed PMID: 11902584]
Level 3 (low-level) evidenceKitagawa K,Matsumoto M,Tagaya M,Hata R,Ueda H,Niinobe M,Handa N,Fukunaga R,Kimura K,Mikoshiba K, 'Ischemic tolerance' phenomenon found in the brain. Brain research. 1990 Sep 24 [PubMed PMID: 2245337]
Level 3 (low-level) evidenceKaria N. Retinal vein occlusion: pathophysiology and treatment options. Clinical ophthalmology (Auckland, N.Z.). 2010 Jul 30:4():809-16 [PubMed PMID: 20689798]
Shahid H, Hossain P, Amoaku WM. The management of retinal vein occlusion: is interventional ophthalmology the way forward? The British journal of ophthalmology. 2006 May:90(5):627-39 [PubMed PMID: 16622095]
Cugati S, Wang JJ, Rochtchina E, Mitchell P. Ten-year incidence of retinal vein occlusion in an older population: the Blue Mountains Eye Study. Archives of ophthalmology (Chicago, Ill. : 1960). 2006 May:124(5):726-32 [PubMed PMID: 16682596]
Scott IU, Ip MS, VanVeldhuisen PC, Oden NL, Blodi BA, Fisher M, Chan CK, Gonzalez VH, Singerman LJ, Tolentino M, SCORE Study Research Group. A randomized trial comparing the efficacy and safety of intravitreal triamcinolone with standard care to treat vision loss associated with macular Edema secondary to branch retinal vein occlusion: the Standard Care vs Corticosteroid for Retinal Vein Occlusion (SCORE) study report 6. Archives of ophthalmology (Chicago, Ill. : 1960). 2009 Sep:127(9):1115-28. doi: 10.1001/archophthalmol.2009.233. Epub [PubMed PMID: 19752420]
Level 1 (high-level) evidenceRogers S, McIntosh RL, Cheung N, Lim L, Wang JJ, Mitchell P, Kowalski JW, Nguyen H, Wong TY, International Eye Disease Consortium. The prevalence of retinal vein occlusion: pooled data from population studies from the United States, Europe, Asia, and Australia. Ophthalmology. 2010 Feb:117(2):313-9.e1. doi: 10.1016/j.ophtha.2009.07.017. Epub [PubMed PMID: 20022117]
Level 1 (high-level) evidence. Argon laser scatter photocoagulation for prevention of neovascularization and vitreous hemorrhage in branch vein occlusion. A randomized clinical trial. Branch Vein Occlusion Study Group. Archives of ophthalmology (Chicago, Ill. : 1960). 1986 Jan:104(1):34-41 [PubMed PMID: 2417579]
Level 1 (high-level) evidenceFunk M,Kriechbaum K,Prager F,Benesch T,Georgopoulos M,Zlabinger GJ,Schmidt-Erfurth U, Intraocular concentrations of growth factors and cytokines in retinal vein occlusion and the effect of therapy with bevacizumab. Investigative ophthalmology [PubMed PMID: 19060280]
Park KS, Kim JW, An JH, Woo JM. Elevated plasma pentraxin 3 and its association with retinal vein occlusion. Korean journal of ophthalmology : KJO. 2014 Dec:28(6):460-5. doi: 10.3341/kjo.2014.28.6.460. Epub 2014 Nov 19 [PubMed PMID: 25435748]
Level 2 (mid-level) evidencePe'er J, Folberg R, Itin A, Gnessin H, Hemo I, Keshet E. Vascular endothelial growth factor upregulation in human central retinal vein occlusion. Ophthalmology. 1998 Mar:105(3):412-6 [PubMed PMID: 9499769]
Noma H, Funatsu H, Yamasaki M, Tsukamoto H, Mimura T, Sone T, Jian K, Sakamoto I, Nakano K, Yamashita H, Minamoto A, Mishima HK. Pathogenesis of macular edema with branch retinal vein occlusion and intraocular levels of vascular endothelial growth factor and interleukin-6. American journal of ophthalmology. 2005 Aug:140(2):256-61 [PubMed PMID: 16086947]
Level 2 (mid-level) evidenceNoma H,Funatsu H,Yamasaki M,Tsukamoto H,Mimura T,Sone T,Hirayama T,Tamura H,Yamashita H,Minamoto A,Mishima HK, Aqueous humour levels of cytokines are correlated to vitreous levels and severity of macular oedema in branch retinal vein occlusion. Eye (London, England). 2008 Jan [PubMed PMID: 16826241]
Brown DM, Campochiaro PA, Bhisitkul RB, Ho AC, Gray S, Saroj N, Adamis AP, Rubio RG, Murahashi WY. Sustained benefits from ranibizumab for macular edema following branch retinal vein occlusion: 12-month outcomes of a phase III study. Ophthalmology. 2011 Aug:118(8):1594-602. doi: 10.1016/j.ophtha.2011.02.022. Epub [PubMed PMID: 21684606]
Level 1 (high-level) evidenceQian T, Zhao M, Xu X. Comparison between anti-VEGF therapy and corticosteroid or laser therapy for macular oedema secondary to retinal vein occlusion: A meta-analysis. Journal of clinical pharmacy and therapeutics. 2017 Oct:42(5):519-529. doi: 10.1111/jcpt.12551. Epub 2017 Jun 22 [PubMed PMID: 28639290]
Level 2 (mid-level) evidenceHaller JA, Bandello F, Belfort R Jr, Blumenkranz MS, Gillies M, Heier J, Loewenstein A, Yoon YH, Jacques ML, Jiao J, Li XY, Whitcup SM, OZURDEX GENEVA Study Group. Randomized, sham-controlled trial of dexamethasone intravitreal implant in patients with macular edema due to retinal vein occlusion. Ophthalmology. 2010 Jun:117(6):1134-1146.e3. doi: 10.1016/j.ophtha.2010.03.032. Epub 2010 Apr 24 [PubMed PMID: 20417567]
Level 1 (high-level) evidencePacella F,La Torre G,Basili S,Autolitano M,Pascarella A,Lenzi T,Pacella E, Comparison between [PubMed PMID: 27903073]
. Argon laser photocoagulation for macular edema in branch vein occlusion. The Branch Vein Occlusion Study Group. American journal of ophthalmology. 1984 Sep 15:98(3):271-82 [PubMed PMID: 6383055]
Level 1 (high-level) evidencePatz A. Argon laser photocoagulation for macular edema in branch vein occlusion. American journal of ophthalmology. 1984 Sep 15:98(3):374-5 [PubMed PMID: 6540993]
Brar M, Grewal DS, Sharma M, Grewal SPS. Rapid regression of retinal neovascularization following intravitreal bevacizumab in branch retinal vein occlusion imaged by optical coherence tomography angiography. Indian journal of ophthalmology. 2018 Apr:66(4):572. doi: 10.4103/ijo.IJO_868_17. Epub [PubMed PMID: 29582824]
Mastropasqua R,Di Antonio L,Di Staso S,Agnifili L,Di Gregorio A,Ciancaglini M,Mastropasqua L, Optical Coherence Tomography Angiography in Retinal Vascular Diseases and Choroidal Neovascularization. Journal of ophthalmology. 2015 [PubMed PMID: 26491548]