Introduction
A build-up of plaque in the carotid artery can lead to atherosclerosis and stenosis of the artery, which may or may not be symptomatic clinically. Such carotid artery disease increases a person’s risk for cerebrovascular disease and stroke. Carotid endarterectomy (CEA) is a surgery performed to decrease the risk of stroke in a patient with known cerebrovascular atherosclerotic disease. The procedure entails removing plaque from the common carotid artery and/or internal carotid artery to improve blood flow and remove potential embolic material, restoring more normal cerebral blood flow. Carotid artery reconstructions began in the early 1950s, and techniques for carotid endarterectomy procedures, as well as indications to perform them, have evolved.[1][2][3][4]
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
Within the superior mediastinum, the arch of the aorta can be found at the level of the sternal angle. Three large vessels originate from the aorta: the brachiocephalic trunk, the left common carotid artery, and the left subclavian artery. On the right side, the common carotid artery arises as the first branch of the brachiocephalic trunk. Both the left and right common carotids bifurcate into an internal and external carotid artery, classically in the neck at the level of the fourth cervical vertebra (C4), near the superior border of the thyroid cartilage. The deep cervical fascia forms the carotid sheath, surrounding the carotid arteries, internal jugular veins, and vagus nerves. They are found medially to the sternocleidomastoid muscle. The internal carotid artery will continue into the skull to form part of the Circle of Willis and supply blood to the brain and eyes. Branches of the external carotid artery supply blood to the neck and face.
Indications
In 1987 the North American Symptomatic Carotid Endarterectomy Trials (NASCET) began. Patients with moderate carotid stenosis (less than 70%) and severe carotid stenosis (greater than 70%) were randomly assigned to treatment groups, which included antithrombotic medication for a majority of patients. The study found that the benefit of surgery was significant for those with severe carotid stenosis and that patients with less than 50% stenosis gained no significant benefit from CEA. This important study forms the basis of current practice guidelines: patients with 50% or more stenosis of the carotid artery and history of ipsilateral stroke or TIA are recommended to have carotid endarterectomy. Symptoms of TIA can include amaurosis fugax, a painless temporary loss of vision in one or both eyes often described as a "curtain falling down" over the visual field, hemiparesis, facial weakness, and speech loss.
A similarly important study examined asymptomatic patients with documented carotid disease. In the Asymptomatic Carotid Artery Stenosis (ACAS) trials for endarterectomy, it was shown that after the procedure there is a significant 5-year reduction in stroke risk in asymptomatic patients with severe stenosis. Asymptomatic patients with 70% or more narrowing, also are encouraged to undertake the surgery. As medical therapy has improved since the 1980s, the CREST-2 trial is currently underway and enrolling patients. The trial aims to provide data comparing intensive medical therapy versus surgery in patients with asymptomatic, high grade internal carotid stenosis.
It is possible to screen asymptomatic patients with the use of carotid duplex ultrasonography (CDU), which can assess the degree of carotid stenosis. The severity of the obstruction correlates with carotid flow velocity: according to Poiseuille's Law, the narrower the lumen of the vessel, the higher the flow rate will be through the stenotic segment. Inaccuracies can be shown if there are tortuosities in the vessel, which may cause elevated velocities. Although CDU is useful in detecting hemodynamically significant stenosis, it has relatively low specificity for those patients with 50% to 60% stenosis. Other forms of screening include computed tomography angiography (CTA), and contrast-enhanced magnetic resonance angiography (CE-MRA). These imaging modalities help to assess other variables that can impact an individual's risk including plaque morphology, intracranial collateralization, and brain perfusion. CTA or CE-MRA information can be used alongside CDU to help determine an individual patient's risk profile when contemplating surgery. [5][6][7][8]
For patients with symptomatic carotid occlusion (50-99%), CEA must be performed shortly after the onset of symptoms to be beneficial. If CEA is performed within 2 weeks of symptom onset, the number needed to treat for preventing one stroke is 5 and is recommended. The number needed to treat increases to 125 if it has been more than 2 weeks from the onset of symptoms or if the patient has had a stroke (lasting neurologic deficit). CEA is beneficial in this group of patients if the symptoms are non-disabling, there are no tandem high-grade stenosis, though CEA can be deferred if the stroke area is large (risk of cerebral edema), if there is contralateral carotid occlusion, hemodynamic instability, and contralateral laryngeal palsy is a relative contraindication. There is more myocardial infarction associated with CEA in this setting.
Carotid artery stenting (CAS) is preferred in symptomatic carotid occlusion (50-99%) with multiple comorbidities, tracheostomy, patients with prior neck radiation or dissection. There is an increased peri-procedural risk of stroke after CAS due to the advancement of the stents and technique, otherwise, outcomes after CAS are comparable to CEA in most instances[9]. CAS is a treatment modality under investigation in the ongoing CREST-2 study.
Contraindications
Symptomatic patients who are very ill and unable to undergo an open surgical procedure may be candidates for carotid angioplasty and stenting (CAS). The stent, a small, flexible, mesh-like tube is inserted into the artery under local anesthesia. The tube is then expanded over a balloon to expand the lumen of the artery and improve blood flow. A multi-institutional study, the Carotid Revascularization Endarterectomy versus Stenting Trials (CREST), demonstrated CEA and CAS yield similar outcomes in terms of postoperative complications such as restenosis, myocardial infarction, long-term stroke, and/or death. However, the risk of peri-procedural stroke was significantly higher in patients undergoing CAS, while the overall risk of myocardial infarction was significantly higher in CEA[9]
While not an absolute contraindication, patients with a history of radiation therapy to the neck are at higher risk of developing temporary cranial nerve injury during CEA, and also at increased risk of late cerebrovascular events and restenosis following CAS. CEA is more technically challenging in the radiated neck because these patients tend to have more diffuse plaques, as well as adhesions, scar tissue, and wound complications as a result of radiation.[10]
Symptomatic women may be at increased risk of postoperative complications after CEA when compared to men, while outcomes and complications remain similar among the sexes for asymptomatic patients. [11]
Preparation
A patient undergoing carotid endarterectomy should be on antiplatelet therapy (unless contraindicated) prior to surgery. For this procedure, general anesthesia or local anesthesia may be used. For local anesthesia, the patient can be awake but sedated. They will feel numbness only at the site of the surgery. The patient should be draped and sterilized at the neck including the jaw and earlobe.
Technique or Treatment
There are two main surgical techniques for carotid endarterectomy: the classical/conventional method and the eversion method.
Classical/Conventional Method
The surgeon makes an incision alongside the medial aspect of the sternocleidomastoid muscle, cutting through fat, the platysma muscle, dissecting deeply to reach the carotid sheath. After carefully incising the sheath, the carotid arteries are exposed. The internal carotid artery is clamped proximal and distal to the plaque temporarily stop blood flow. The surgeon will open along the length of the internal carotid artery, progressing proximally and distally to locate both ends of the plaque. The clamps are released one at a time and a flexible bypass stent is placed to temporarily shunt blood around the endarterectomy site while the blockage is removed. The artery then repaired with a patch that will widen the vessel lumen, and the bypass stent is removed. There are different patch materials available including autologous vein, bovine patch, or synthetics (Dacron). After the vessel is repaired, satisfactory blood flow is confirmed with ultrasound Doppler or angiography.
Eversion Method
With the eversion method, the internal carotid artery is transected at its origin at the bifurcation. The vessel wall is everted circumferentially around the plaque, and the plaque is divided and removed. The artery is then repaired in an end to end anastomotic fashion. The advantages of the eversion method include no need for patch closure and overall shorter carotid clamping time and total operative time.
Complications
Complications during and after surgery are dependent on various factors, such as surgeon skill and technique, patient’s risk factors, management before or after surgery.
Complications of CEA include:
Major complications
- Myocardial Infarction
- Hyperperfusion syndrome
- Nerve Injury, particularly the cranial nerves: hypoglossal, vagus, glossopharyngeal, and facial (marginal mandibular) nerves
- Perioperative stroke
- Restenosis
- Death
Minor Complications
- Transient ischemic attack
- Bleeding
- Infection
- Greater auricular nerve injury
- Dysphagia
Clinical Significance
Carotid endarterectomy is a stroke-preventing procedure that helps improve patient health and subsequent quality of life. Surgical treatment in patients with moderate to severe carotid disease has been shown to significantly decrease stroke and improve overall survival.[12][13]
Enhancing Healthcare Team Outcomes
Patients with TIA or evidence of carotid artery atherosclerosis are frequently seen by the primary care provider or nurse practitioner. If the workup reveals narrowing of the carotid artery, the patient should be referred to the neurologist and vascular surgeon based on degree of stenosis and symptoms present. Carotid endarterectomy has been shown to reduce the risk of stroke in properly selected patients. Stroke is also a potential complication of CEA, therefore physicians must educate the patient regarding potential complications of the procedure. The primary care physician should encourage the patient to eliminate controllable risk factors for stroke by discontinuing smoking, maintaining a healthy weight and lowering levels of cholesterol. Regular exercise is highly recommended.[14]
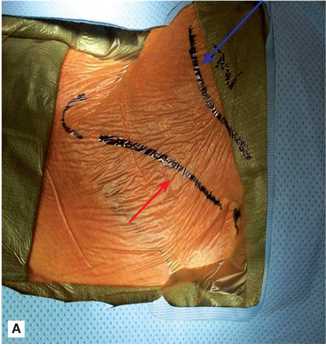
Media
(Click Image to Enlarge)
References
Faateh M, Dakour-Aridi H, Kuo PL, Locham S, Rizwan M, Malas MB. Risk of emergent carotid endarterectomy varies by type of presenting symptoms. Journal of vascular surgery. 2019 Jul:70(1):130-137.e1. doi: 10.1016/j.jvs.2018.10.064. Epub 2019 Feb 15 [PubMed PMID: 30777684]
Rasheed AS, White RS, Tangel V, Storch BM, Pryor KO. Carotid Revascularization Procedures and Perioperative Outcomes: A Multistate Analysis, 2007-2014. Journal of cardiothoracic and vascular anesthesia. 2019 Jul:33(7):1963-1972. doi: 10.1053/j.jvca.2019.01.022. Epub 2019 Jan 9 [PubMed PMID: 30773439]
Lan Y, Lyu J, Ma X, Ma L, Lou X. Longitudinal assessment of cerebral blood flow changes following carotid artery stenting and endarterectomy. La Radiologia medica. 2019 Jul:124(7):636-642. doi: 10.1007/s11547-018-00986-7. Epub 2019 Feb 15 [PubMed PMID: 30771219]
Tyson AC, Parikh S, Singh K, Zia S, Deitch JS, Schor JA. Routine Postoperative Cardiac Testing is Unnecessary after Carotid Endarterectomy. Annals of vascular surgery. 2019 Aug:59():12-15. doi: 10.1016/j.avsg.2018.11.028. Epub 2019 Feb 13 [PubMed PMID: 30769059]
Babić S, Tanasković S, Nešković M, Gajin P, Nenezić D, Stevanović P, Aleksić N, Ševković M, Ilijevski N, Matić P, Popov P, Vučurević G, Unić-Stojanović D, Radak D. Surgical Treatment of Proximal Segmental Occlusion of the Internal Carotid Artery. Surgery research and practice. 2019:2019():2976091. doi: 10.1155/2019/2976091. Epub 2019 Jan 2 [PubMed PMID: 30719497]
Lamanna A, Maingard J, Barras CD, Kok HK, Handelman G, Chandra RV, Thijs V, Brooks DM, Asadi H. Carotid artery stenting: Current state of evidence and future directions. Acta neurologica Scandinavica. 2019 Apr:139(4):318-333. doi: 10.1111/ane.13062. Epub 2019 Feb 6 [PubMed PMID: 30613950]
Level 3 (low-level) evidenceWang LJ, Ergul EA, Conrad MF, Malas MB, Kashyap VS, Goodney PP, Patel VI, Clouse WD. Addition of proximal intervention to carotid endarterectomy increases risk of stroke and death. Journal of vascular surgery. 2019 Apr:69(4):1102-1110. doi: 10.1016/j.jvs.2018.07.042. Epub 2018 Dec 13 [PubMed PMID: 30553728]
Texakalidis P, Giannopoulos S, Kokkinidis DG, Karasavvidis T, Rangel-Castilla L, Reavey-Cantwell J. Carotid Artery Endarterectomy Versus Carotid Artery Stenting for Patients with Contralateral Carotid Occlusion: A Systematic Review and Meta-Analysis. World neurosurgery. 2018 Dec:120():563-571.e3. doi: 10.1016/j.wneu.2018.08.183. Epub 2018 Sep 3 [PubMed PMID: 30189300]
Level 1 (high-level) evidenceMüller MD, Lyrer P, Brown MM, Bonati LH. Carotid artery stenting versus endarterectomy for treatment of carotid artery stenosis. The Cochrane database of systematic reviews. 2020 Feb 25:2(2):CD000515. doi: 10.1002/14651858.CD000515.pub5. Epub 2020 Feb 25 [PubMed PMID: 32096559]
Level 1 (high-level) evidenceRenard R, Davaine JM, Couture T, Jayet J, Tresson P, Gaudric J, Chiche L, Koskas F. Surgical repair of radiation-induced carotid stenosis. Journal of vascular surgery. 2020 Sep:72(3):959-967. doi: 10.1016/j.jvs.2019.11.034. Epub 2020 Feb 5 [PubMed PMID: 32035779]
Mayor JM, Salemi JL, Dongarwar D, Salihu HM, Montero-Baker M, Mills JL, Chung J. Sex-Based Differences in Ten-Year Nationwide Outcomes of Carotid Revascularization. Journal of the American College of Surgeons. 2019 Jul:229(1):38-46.e4. doi: 10.1016/j.jamcollsurg.2019.02.054. Epub 2019 Mar 26 [PubMed PMID: 30922980]
Naylor AR. Endarterectomy versus stenting for stroke prevention. Stroke and vascular neurology. 2018 Jun:3(2):101-106. doi: 10.1136/svn-2018-000146. Epub 2018 Feb 24 [PubMed PMID: 30022797]
Balucani C, Arnedo V, Weedon J, Leys D, Mas JL, Brown M, Grotta JC, Gonzales NR, Hacke W, Brott T, Levine SR. Transatlantic Differences in Management of Carotid Stenosis: BRIDGing the Gap in StrokE Management (BRIDGE) Project. The Neurohospitalist. 2018 Jul:8(3):113-123. doi: 10.1177/1941874417747772. Epub 2018 Jan 17 [PubMed PMID: 29977441]
Chung BH, Heo SH, Park YJ, Kim YW, Woo SY, Kim DI. Comparative Analysis Using Propensity Score Matching Analysis: Primary Closure versus Patch Angioplasty During Carotid Endarterectomy. Annals of vascular surgery. 2020 Jan:62():166-172. doi: 10.1016/j.avsg.2018.11.011. Epub 2019 Feb 11 [PubMed PMID: 30763710]
Level 2 (mid-level) evidence