Introduction
The carotid sinus, also known as the carotid bulb, is a neurovascular structure that appears as a dilation at the bifurcation of the common carotid artery, and the beginning of the internal carotid artery. It is localized near the arterial pulse, inferior to the angle of the mandible at the level of the thyroid cartilage. The carotid sinus contains baroreceptors (stretch receptors), which are sensitive to pressure changes in the arterial blood pressure. The carotid sinus has dense innervation of many types of receptors that play a role in the control of blood pressure. Carotid sinus baroreceptor has a crucial role in the control of blood pressure and heart rate. Afferent signals travel from carotid baroreceptors to the cardiovascular control center in midbrain via the glossopharyngeal nerve. The efferent signals transmit via parasympathetic and sympathetic nerves to the heart and blood vessels. This response brings appropriate changes to maintain heart rate and blood pressure in normal physiological limits, which is known as carotid sinus baroreflex.[1] There is inter and intra-individual variation in the location of the carotid sinus, which is clinically very important.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The common carotid artery travels in the neck, and at the upper thyroid cartilage, it bifurcates into internal and external carotid arteries on both the side. The carotid sinus, which is a neurovascular structure appears as dilatation of the arterial wall more commonly at the beginning of the internal carotid artery.[1] It is in the adventitial layer of the carotid bulb of the internal carotid artery.
The carotid sinus baroreceptor functions as a sensor responding to the mechanical stretch that occurs to the carotid artery as the arterial blood pressure increases. There are two types of baroreceptors. Type 1 (Dynamic) has large myelinated A-fibers, and Type 2 (Tonic) has small A and unmyelinated C-fibers. When mean arterial pressure (MAP) increases baroreceptors in the carotid sinus, and aortic arch sends afferent signals via the glossopharyngeal nerve to the cardiovascular control center (baroreceptor input goes to commissural, medial, dorsomedial and dorsolateral subnuclei of nucleus tractus solitarius in the brainstem).[2] This input will, in turn, stimulate the parasympathetic tone and inhibit sympathetic tone. Thus it will decrease the heart rate (stimulation of parasympathetic efferent nerves acting on SA node) and reduce the blood pressure (due to inhibition of sympathetic tone). In short, the increase in blood pressure in carotid sinus will stimulate stretch receptors, which leads to reflex bradycardia and systemic vasodilatation.
The baroreceptor reflex is also critical in maintaining heart rate and blood pressure during postural changes. Standing from the supine position leads to pooling of 500 to 1000 ml of blood in lower extremities and splanchnic circulation, which results in decreased venous return and a resultant decrease in cardiac output and blood pressure. The reduction in blood pressure leads to a decline in the stretching of the carotid sinus baroreceptor. This reflexly increases sympathetic outflow and decreases a parasympathetic outflow. Thus it increases the heart rate and blood pressure (due to vasoconstriction of systemic vessels). Therefore, changing the posture from supine to standing results in only a small fall in systolic and diastolic blood pressure (5 to 10 mmHg) and an increase in heart rate (10 to 25 bpm). Thus the failure of the baroreceptor reflex leads to a fall in blood pressure (more than 10 mmHg) with the assumption of upright posture, which is known as orthostatic hypotension.
The baroreceptors, both in the carotid sinus and aortic arch, are the terminal endings of sensory nerve fibers that express many nonselective cation channels in the transient receptor potential (TRP) family. TRP1 is sensitive to stretch. The transmural pressure causes the vessel to expand and produce an inward current that depolarizes the receptor, causing a receptor potential whose amplitude is proportional to the stretch of the vessel.
Embryology
The common carotid artery, the proximal part of the internal carotid artery, and the carotid sinus derive from the third pharyngeal arch.[3] The common carotid artery develops from the proximal segment of the third aortic arch. The internal carotid artery and carotid sinus develop from the distal segment of the third aortic arch.[4] The carotid sinus derives from the ectodermal sheet. Even though there is a substantial growth of the internal carotid artery from childhood to young adult, the appearance of the carotid sinus near the base of the artery appears only at the teenage age.[5][6]
Blood Supply and Lymphatics
The carotid sinus is a dilation at the base of the internal carotid artery. The nearby carotid body is a fibrous-covered structure that rests posteriorly to the carotid bifurcation. The blood supply to carotid sinus is by the vasa vasorum vessels. It is an observable phenomenon that atherosclerotic plaques stimulate the release of serotonin and passes through vasa vasorum vessels of the carotid sinus. This serotonin then affects nerves leading to the dysfunction of baroreceptors.[7] The lymphatics from carotid sinus drain directly into the deep cervical lymph nodes that are within the carotid sheath.[8]
Nerves
Primarily, the glossopharyngeal nerve innervates the carotid sinus, particularly the branch called the sinus nerve of Hering. The glossopharyngeal nerve will synapse with the nucleus tractus solitarius in the brainstem's medulla, which will send information to the autonomic nervous system to control MAP. The glossopharyngeal nerve is a mixed nerve, and it is the general visceral afferent component that carries the sensory information from the carotid sinus.
Muscles
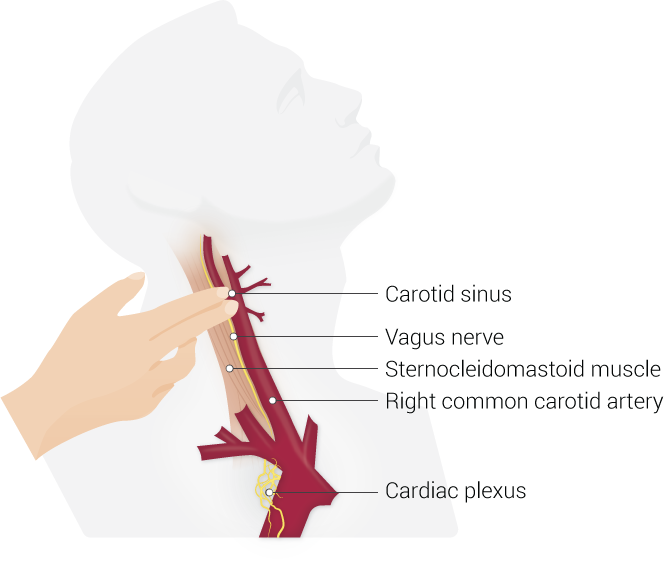
The carotid sinus is a sensitive structure and can change the blood pressure quite drastically. Hence it is well protected from outside with superficial muscle like sternocleidomastoid muscle and deep muscles of the neck, especially the suprahyoid muscles.[9] It is particularly found with regards to the sternocleidomastoid muscle, that any stimulation of this muscle leads to interference with the firing of the carotid baroreceptors. This interference results in syncope in patients with carotid sinus hypertension, which is the same mechanism used in carotid sinus massage eliciting cardioinhibitory and vasodepressor responses.[9]
Physiologic Variants
There is an inter and intraindividual variation in the location of the carotid sinus. This knowledge of variations of the carotid sinus is quite essential for a surgeon before going for any interventions (like carotid endarterectomy, carotid stenting, etc.) at this site, as accidental stimulating it might lead to severe hypotension, bradycardia and rarely cardiac arrest.
Four different sites of carotid sinus exist:
- Site 1 - starts in the distal common carotid artery and extends to the proximal internal carotid artery, which is the most common location (74.3%).
- Site 2 - starts in the distal common carotid artery and extends to both the proximal internal carotid artery and proximal external carotid artery (7.3%).
- Site 3 - starts in the distal common carotid artery with no extension after bifurcation (17.1%).
- Site 4 - starts in the distal common carotid artery and extends to the proximal external carotid artery, which is the least common location of all (1.22%).[10]
Surgical Considerations
The carotid sinus is a common site for the formation of atheromatous plaque predisposing to significant disabilities and fatal strokes. This plaque is detected and removed by procedures like carotid endarterectomy.[10]
This location is also a site for unique tumors called the carotid bifurcation paragangliomas arising from the carotid bodies.[11] In some cases of carotid sinus syndrome where the symptoms are uncontrolled by medical treatment, an intervention will be necessary by surgical denervation close to the carotid sinus itself.[12]
The sternocleidomastoid plays an important role, and its chronic denervation is essential in old patients with carotid sinus hypersensitivity.[13]
Clinical Significance
The carotid sinus is very sensitive to touch and pressure. Carotid bifurcation is a prevalent site for the formation of atheromatous plaque, which leads to thromboembolic stroke. During the intervention for its correction, anatomical variation in the location of the carotid sinus in different individuals can lead to an increased risk of injury to carotid sinus or stimulation of carotid sinus by angioplasty stent or balloon. Damage to carotid sinus during surgery leads to postoperative hemodynamic instability. Carotid sinus stimulation during intervention predisposes to coronary vasospasm and resultant myocardial infarction. During carotid endarterectomy surgery, the surgeon will usually desensitize the carotid sinus by injecting a tiny amount of lidocaine into the carotid adventitia to prevent the baroreceptor stimulation during the procedure.
Some individuals develop carotid sinus hypersensitivity (CSH) or carotid sinus syncope.[14] The CSH is a pause in the heart rate (HR) of more than three seconds, and more than 50 mmHg of a drop in blood pressure during carotid sinus massage, may or may not present with symptoms such as syncope, pre-syncope/lightheadedness, near-syncope or unexplained fall in older individuals.[15] The CSH presenting with such symptoms has the name carotid sinus syndrome.[16] It is more common in older individuals, particularly males (twice that of females) who suffer from atherosclerotic vascular disease, patients with tumors in the carotid sinus region, or persons with a history of prior neck surgery or irradiation.[17][18][17] It can be due to increased response of peripheral receptors or abnormal response of central reflex sites. In these individuals, stimulation of carotid sinus baroreceptors results in a more significant than expected decrease in heart rate and blood pressure. In such personalities, even shaving the neck, turning the neck, or looking upward may cause attacks of syncope and loss of consciousness.
Diagnosis is possible by performing a carotid sinus massage, which is the external stimulation of baroreceptors. The patient in the supine position with the neck flexed, gentle pressure is applied for 5 to 10 seconds on one carotid sinus. Head-up tilt test is more effective than carotid massage. HR and BP changes are monitored with a beat-by-beat HR/BP monitor system during the procedure. The response elicited can be cardioinhibitory (more than 3 seconds of pause in HR), vasodepressor (more than 50 mmHg decrease in BP), or mixed.[1] However, the practitioner should only perform this test in a controlled environment with resuscitation equipment available. Before performing carotid sinus massage, it is essential to obtain an ultrasound to ensure that the patient does not have a thrombus or atheroma in the carotid artery, which could be susceptible to dislodgement and put the patient in immediate danger of cerebrovascular thromboembolism. It can also be useful to differentiate supraventricular tachycardia from ventricular tachycardia.[2] Research has also observed that the carotid sinus massage was more accurate in the diagnosis of coronary artery disease. The higher the number of coronary vessels involved, the more was the drop in blood pressure and pulse.[19]
Treatment:
Asymptomatic patients with normal response to carotid sinus massage do not require any intervention. Patients must understand that they need to avoid positions or movements which might accidentally stimulate carotid baroreceptors.
In symptomatic patients with a cardioinhibitory response or mixed response, clinicians achieve permanent cardiac pacing by implanting a permanent cardiac pacemaker (dual-chamber pacing is the favored approach). In patients with abnormal vasodilator response, vasoconstrictor drugs such as midodrine are an option.[1]
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Kikuta S, Iwanaga J, Kusukawa J, Tubbs RS. Carotid Sinus Nerve: A Comprehensive Review of Its Anatomy, Variations, Pathology, and Clinical Applications. World neurosurgery. 2019 Jul:127():370-374. doi: 10.1016/j.wneu.2019.04.064. Epub 2019 Apr 14 [PubMed PMID: 30995553]
Porzionato A, Macchi V, Stecco C, De Caro R. The Carotid Sinus Nerve-Structure, Function, and Clinical Implications. Anatomical record (Hoboken, N.J. : 2007). 2019 Apr:302(4):575-587. doi: 10.1002/ar.23829. Epub 2018 May 2 [PubMed PMID: 29663677]
Sethi D, Gofur EM, Munakomi S. Anatomy, Head and Neck: Carotid Arteries. StatPearls. 2023 Jan:(): [PubMed PMID: 31424822]
Kau T, Sinzig M, Gasser J, Lesnik G, Rabitsch E, Celedin S, Eicher W, Illiasch H, Hausegger KA. Aortic development and anomalies. Seminars in interventional radiology. 2007 Jun:24(2):141-52. doi: 10.1055/s-2007-980040. Epub [PubMed PMID: 21326792]
Seong J, Jeong W, Smith N, Towner RA. Hemodynamic effects of long-term morphological changes in the human carotid sinus. Journal of biomechanics. 2015 Apr 13:48(6):956-62. doi: 10.1016/j.jbiomech.2015.02.009. Epub 2015 Feb 12 [PubMed PMID: 25702250]
Seong J, Lieber BB, Wakhloo AK. Morphological age-dependent development of the human carotid bifurcation. Journal of biomechanics. 2005 Mar:38(3):453-65 [PubMed PMID: 15652543]
Williams JK, Orgren KI, Armstrong ML, Heistad DD. Vasa vasorum in the carotid sinus of atherosclerotic monkeys: implications for baroreceptor function. Atherosclerosis. 1989 Jul:78(1):25-32 [PubMed PMID: 2757684]
Level 3 (low-level) evidenceClapham R, O'Sullivan E, Weller RO, Carare RO. Cervical lymph nodes are found in direct relationship with the internal carotid artery: significance for the lymphatic drainage of the brain. Clinical anatomy (New York, N.Y.). 2010 Jan:23(1):43-7. doi: 10.1002/ca.20887. Epub [PubMed PMID: 19918869]
Khan YS, Bordoni B. Anatomy, Head and Neck, Suprahyoid Muscle. StatPearls. 2023 Jan:(): [PubMed PMID: 31536316]
West CT, Brassett C, Gaunt ME. Variations in carotid sinus anatomy and their relevance to carotid interventions. Folia morphologica. 2018:77(4):693-697. doi: 10.5603/FM.a2018.0017. Epub 2018 Mar 3 [PubMed PMID: 29500893]
Michalinos A, Chatzimarkos M, Arkadopoulos N, Safioleas M, Troupis T. Anatomical Considerations on Surgical Anatomy of the Carotid Bifurcation. Anatomy research international. 2016:2016():6907472. doi: 10.1155/2016/6907472. Epub 2016 Mar 7 [PubMed PMID: 27047690]
Toorop RJ, Scheltinga MR, Moll FL, Bleys RL. Anatomy of the carotid sinus nerve and surgical implications in carotid sinus syndrome. Journal of vascular surgery. 2009 Jul:50(1):177-82. doi: 10.1016/j.jvs.2009.03.029. Epub [PubMed PMID: 19563966]
Lloyd MG, Wakeling JM, Koehle MS, Drapala RJ, Claydon VE. Carotid sinus hypersensitivity: block of the sternocleidomastoid muscle does not affect responses to carotid sinus massage in healthy young adults. Physiological reports. 2017 Oct:5(19):. doi: 10.14814/phy2.13448. Epub 2017 Oct 16 [PubMed PMID: 29038360]
Moosavi V, Paymard M. Carotid sinus hypersensitivity. The Medical journal of Australia. 2019 Apr:210(6):257-257.e1. doi: 10.5694/mja2.50056. Epub 2019 Mar 4 [PubMed PMID: 30829401]
van den Brink RB, de Lange FJ. [Carotid sinus massage is not a benign intervention]. Nederlands tijdschrift voor geneeskunde. 2017:161():D1312 [PubMed PMID: 28378703]
Sutton R. Carotid sinus syndrome: Progress in understanding and management. Global cardiology science & practice. 2014:2014(2):1-8. doi: 10.5339/gcsp.2014.18. Epub 2014 Jun 18 [PubMed PMID: 25405171]
Level 3 (low-level) evidenceTan MP, Newton JL, Reeve P, Murray A, Chadwick TJ, Parry SW. Results of carotid sinus massage in a tertiary referral unit--is carotid sinus syndrome still relevant? Age and ageing. 2009 Nov:38(6):680-6. doi: 10.1093/ageing/afp160. Epub 2009 Sep 7 [PubMed PMID: 19736287]
Level 2 (mid-level) evidenceKumar NP, Thomas A, Mudd P, Morris RO, Masud T. The usefulness of carotid sinus massage in different patient groups. Age and ageing. 2003 Nov:32(6):666-9 [PubMed PMID: 14600010]
Level 2 (mid-level) evidenceUlgen MS, Karadede A, Alan S, Toprak N. The value of hemodynamic changes induced by carotid sinus massage on the diagnosis of coronary artery disease. Angiology. 2001 Oct:52(10):703-9 [PubMed PMID: 11666135]