Umbilical Artery Catheterization
Umbilical Artery Catheterization
Introduction
Umbilical arterial catheterization provides direct access to the arterial system, thus enabling arterial blood sampling and the measurement of the systemic arterial blood pressure. It is one of the commonly performed procedures in extremely premature neonates. The procedure is relatively easy to perform but requires practice.[1] This chapter will review the indications, technique of catheterizing the umbilical artery, and potential complications associated with its use in managing neonates who undergo this procedure.
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
The umbilical artery originates from the anterior division of the internal iliac artery. In fetal life, it traverses within the umbilical cord carrying oxygen-depleted blood from the fetus to the placenta. Usually, there are two umbilical arteries and one umbilical vein within the umbilical cord. In approximately 1% of pregnancies, one of the umbilical arteries may undergo atresia, aplasia, or agenesis resulting in a single umbilical artery. In most cases, a single umbilical artery is an isolated finding, but if it is associated with other fetal anomalies, there is an increased risk of chromosomal abnormalities. The umbilical arteries are identified by their caudal location within the cord with thicker walls and smaller lumen.[2]
Indications
The primary indications for umbilical artery catheterization include the need for frequent measurement of arterial blood gases, frequent blood sampling, or continuous blood pressure monitoring in the extremely low-birthweight infant or critically ill neonates. Occasionally, it can be used temporarily to infusion parenteral nutrition if alternate access is unavailable.
Refractory hypoglycemia is a rare complication of umbilical arterial catheters when dextrose is infusing through them.
An umbilical arterial catheter can be lifesaving in managing critically ill neonates. However, the risks and benefits must be carefully weighed before attempting the procedure due to the potential complications associated with its use. Very low birth weight infants (with less than 1000 g body weight), preterm infants who need mechanical ventilator support, infants with hypoxic-ischemic encephalopathy undergoing therapeutic hypothermia, critically ill late preterm or term infants requiring mechanical ventilation are some of the groups of neonates who might benefit from the use of umbilical arterial catheter owing to the need for frequent blood sampling.[2]
Contraindications
Omphalitis, necrotizing enterocolitis, omphalocele, gastroschisis, and peritonitis are some of the contraindications for the placement of an umbilical arterial catheter.[3]
Equipment
- Sterile gown, sterile gloves, cap, and mask
- Sterile drapes
- Bactericidal solution
- Umbilical tie
- Measuring tape
- Scissors
- Scalpel
- Toothed iris forceps
- Two curved, nontoothed iris forceps
- Two curved mosquito hemostats
- Umbilical catheter-5-French (Fr) gauge for infants weighing >1200 g, 3.5-Fr gauge for infants weighing >1500 g
- Three-way stopcock
- Intravenous (IV) tubing
- Needle driver
- 3-0 silk suture
- Sterile saline flush
- 4 x 4-inch gauze sponges[4]
Personnel
A clinician or an advanced practitioner with adequate training should perform the procedure. Secondary personnel, such as a nurse, should also be present to help monitor the patient throughout the process.
Preparation
After determining the necessity for an umbilical arterial catheter, informed consent must be obtained as per the local institutional policy. Measures should be taken to avoid hypothermia in the infant while doing the procedure. These include the use of a radiant warmer and placement of an exothermic mattress under the infant, as necessary while performing the procedure. The three-way stopcock must be attached to the desired catheter and flushed with saline solution. It is better to use 0.45% normal saline to avoid hypernatremia using 0.9% normal saline. The flush syringe must be left attached to the stopcock with the stopcock turned off. The length of the insertion of the catheter tip has to be determined before the insertion.
The ideal position of the catheter tip should be in the descending aorta above the origin of the celiac, mesenteric, and renal arteries to avoid occlusion of these vessels. This high position (thoracic vertebra level T6-T9) is preferred compared to the low position, i.e., below the renal arteries (lumbar vertebra level L3-L4), as it is associated with fewer complications of thrombosis.[5] The catheter length is estimated from the formula [(birth weight in kg x 3) + 9] cm. Other methods for estimating the depth of insertion are also described.[6][7] The length of the stump above the skin is added to this measurement.
Technique or Treatment
Before starting the procedure, the infant must be restrained to minimize movement. The umbilical cord and the surrounding skin are cleaned with an antiseptic solution. The cord is better cleaned with an assistant grasping the cord by the cord clamp or forceps and pulling the cord vertically out of the field. The area is then draped, and an umbilical tie is placed around the cord, tight enough to minimize blood loss but loose enough to allow catheters to be passed easily through the vessels. The cord is then cut horizontally 1 cm to 1.5 cm from the skin. The umbilical arteries are identified by their thick walls with a smaller lumen. The cord stump is grasped, and traction applied. The lumen of the artery is probed gently by introducing the closed tips of the iris forceps and then is dilated by allowing the forceps to spring apart, maintaining in this position for about 30 seconds. The catheter is then grasped with the curved iris forceps, or between the thumb and forefinger, and inserted into the lumen of the dilated artery.
If there is any resistance to the advancement of the catheter, gentle, steady pressure must be applied. Repeated probing or excessive pressure can result in perforation of the vessel. If unsuccessful, catheterization of the other artery must be attempted. After advancing to the appropriate distance, the catheter is secured using purse-string sutures around the base of the cord, and the tie removed. Radiologic confirmation of the catheter tip must be obtained to confirm its location between the T6-T9 vertebra. The catheter can be retracted if needed, but it should never be advanced once it is secured due to the risk of introducing infection. Infusion of a heparinized solution must be started as soon as the catheter tip is verified to be in an appropriate position.[8]
Complications
Thromboembolism is a major concern with the use of umbilical arterial catheters. Occlusion of the mesenteric arteries can result in gut ischemia, bowel infarction, and necrotizing enterocolitis. Renal artery involvement can lead to hypertension or acute renal failure. More distal vascular accidents can result in an ischemic injury to the back, buttocks, and lower extremities. Removal of the catheter must be considered the first sign of any vascular compromise. Other complications, such as vessel perforation, peritoneal perforation, bladder injury, and false aneurysm, can occur during catheter insertion. Catheter-associated infection and bleeding are other frequently associated complications. Refractory hypoglycemia is a rare complication associated with high position umbilical artery catheters whose tip is near the celiac and mesenteric arteries.[9][10][11][12]
There is a theoretical concern of necrotizing enterocolitis while infants are enterally fed in the presence of an umbilical arterial catheter. However, there is no evidence supporting this, and withholding enteral feeds while an infant has an umbilical arterial catheter is no longer recommended.
Thromboembolism is a significant concern with the use of umbilical arterial catheters. Occlusion of the mesenteric arteries can result in gut ischemia, bowel infarction, and necrotizing enterocolitis. Renal artery involvement can lead to hypertension or acute renal failure. Vascular accidents that occur more distally can result in an ischemic injury of the back, buttocks, and lower extremities. Removal of the catheter must be considered the first sign of any vascular compromise. Other complications, such as vessel perforation, peritoneal perforation, bladder injury, and false aneurysm, can occur during catheter insertion. Catheter-associated infection and bleeding are other frequently associated complications. Refractory hypoglycemia is a rare complication associated with high position umbilical artery catheters whose tip is near the celiac and mesenteric arteries.
Clinical Significance
An umbilical arterial catheter can be lifesaving in managing critically ill neonates. However, the risks and benefits must be carefully weighed before attempting the procedure due to the potential complications associated with its use.[13] Extremely low birth weight infants (< 1000 g), preterm infants who require mechanical ventilatory support, infants with hypoxic-ischemic encephalopathy undergoing therapeutic hypothermia, critically ill late preterm or term infants requiring mechanical ventilation are some of the groups of neonates who might benefit from the use of umbilical arterial catheter owing to the need for frequent blood sampling. It is helpful to adhere to guidelines standardizing the use of umbilical catheters in neonates.[14]
There is a theoretical concern of necrotizing enterocolitis while infants are enterally fed in the presence of an umbilical arterial catheter. However, there is no evidence supporting this, and withholding enteral feeds while an infant has an umbilical arterial catheter is no longer recommended.
Enhancing Healthcare Team Outcomes
An interprofessional healthcare team approach is essential for the successful insertion and maintenance of umbilical arterial catheterization. This team will include PHysicians (MDs and DOs), specialists, mid-level practitioners (NPs and PAs), nursing staff, and surgical assistants, all with specialized neonatal care training. As discussed earlier, communication and coordination between the clinicians/advanced practitioners and nurses are very important. The necessity of the catheter must be evaluated every day by the healthcare team, with nursing staff reporting any findings they observe during care, and it must be removed when no longer necessary.[15] [Level 2] Continuation of the umbilical arterial catheter beyond five days is not recommended due to the risk of infection and thrombosis associated with its prolonged use.[16][17] [Level 2]
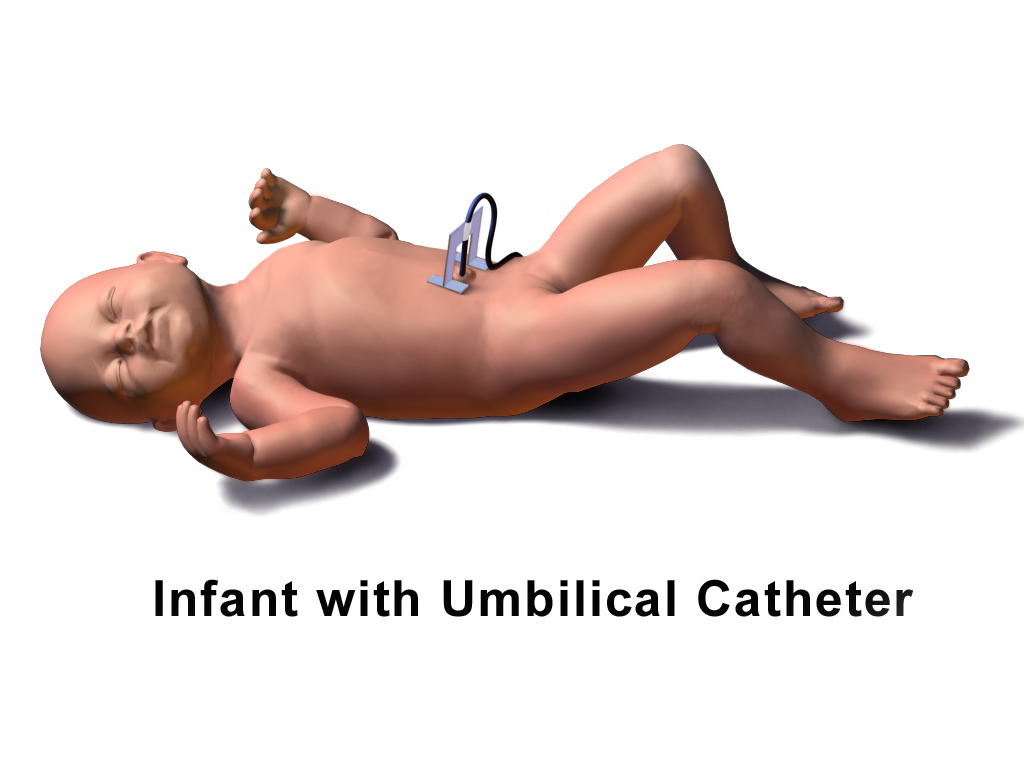
Media
(Click Image to Enlarge)
References
Wallenstein MB, Shaw GM, Yang W, Stevenson DK. Failed umbilical artery catheterization and adverse outcomes in extremely low birth weight infants. The journal of maternal-fetal & neonatal medicine : the official journal of the European Association of Perinatal Medicine, the Federation of Asia and Oceania Perinatal Societies, the International Society of Perinatal Obstetricians. 2019 Nov:32(21):3566-3570. doi: 10.1080/14767058.2018.1468430. Epub 2018 May 2 [PubMed PMID: 29681181]
DeFreitas MJ, Mathur D, Seeherunvong W, Cano T, Katsoufis CP, Duara S, Yasin S, Zilleruelo G, Rodriguez MM, Abitbol CL. Umbilical artery histomorphometry: a link between the intrauterine environment and kidney development. Journal of developmental origins of health and disease. 2017 Jun:8(3):349-356. doi: 10.1017/S2040174417000113. Epub 2017 Mar 6 [PubMed PMID: 28260559]
Sakurai M, Donnelly LF, Klosterman LA, Strife JL. Congenital diaphragmatic hernia in neonates: variations in umbilical catheter and enteric tube position. Radiology. 2000 Jul:216(1):112-6 [PubMed PMID: 10887235]
Level 2 (mid-level) evidenceElser HE. Options for securing umbilical catheters. Advances in neonatal care : official journal of the National Association of Neonatal Nurses. 2013 Dec:13(6):426-9. doi: 10.1097/ANC.0000000000000038. Epub [PubMed PMID: 24300962]
Level 3 (low-level) evidenceBarrington KJ. Umbilical artery catheters in the newborn: effects of position of the catheter tip. The Cochrane database of systematic reviews. 2000:1999(2):CD000505 [PubMed PMID: 10796375]
Level 1 (high-level) evidenceRosenfeld W, Estrada R, Jhaveri R, Salazar D, Evans H. Evaluation of graphs for insertion of umbilical artery catheters below the diaphragm. The Journal of pediatrics. 1981 Apr:98(4):627-8 [PubMed PMID: 7205493]
Level 2 (mid-level) evidenceShukla H, Ferrara A. Rapid estimation of insertional length of umbilical catheters in newborns. American journal of diseases of children (1960). 1986 Aug:140(8):786-8 [PubMed PMID: 3728405]
Barrington KJ. Umbilical artery catheters in the newborn: effects of heparin. The Cochrane database of systematic reviews. 2000:1999(2):CD000507 [PubMed PMID: 10796377]
Level 1 (high-level) evidenceRamasethu J. Complications of vascular catheters in the neonatal intensive care unit. Clinics in perinatology. 2008 Mar:35(1):199-222, x. doi: 10.1016/j.clp.2007.11.007. Epub [PubMed PMID: 18280883]
McAdams RM, Winter VT, McCurnin DC, Coalson JJ. Complications of umbilical artery catheterization in a model of extreme prematurity. Journal of perinatology : official journal of the California Perinatal Association. 2009 Oct:29(10):685-92. doi: 10.1038/jp.2009.73. Epub 2009 Jun 25 [PubMed PMID: 19554012]
Level 3 (low-level) evidenceSobczak A, Klepacka J, Amrom D, Żak I, Kruczek P, Kwinta P. Umbilical catheters as vectors for generalized bacterial infection in premature infants regardless of antibiotic use. Journal of medical microbiology. 2019 Sep:68(9):1306-1313. doi: 10.1099/jmm.0.001034. Epub 2019 Jul 5 [PubMed PMID: 31274401]
Malik M, Wilson DP. Umbilical artery catheterization: a potential cause of refractory hypoglycemia. Clinical pediatrics. 1987 Apr:26(4):181-2 [PubMed PMID: 3549107]
Level 3 (low-level) evidenceElboraee MS, Toye J, Ye XY, Shah PS, Aziz K, Canadian Neonatal Network Investigators. Association between Umbilical Catheters and Neonatal Outcomes in Extremely Preterm Infants. American journal of perinatology. 2018 Feb:35(3):233-241. doi: 10.1055/s-0037-1606607. Epub 2017 Sep 14 [PubMed PMID: 28910847]
Shahid S, Dutta S, Symington A, Shivananda S, McMaster University NICU. Standardizing umbilical catheter usage in preterm infants. Pediatrics. 2014 Jun:133(6):e1742-52. doi: 10.1542/peds.2013-1373. Epub 2014 May 19 [PubMed PMID: 24843063]
Level 3 (low-level) evidenceBoo NY, Wong NC, Zulkifli SS, Lye MS. Risk factors associated with umbilical vascular catheter-associated thrombosis in newborn infants. Journal of paediatrics and child health. 1999 Oct:35(5):460-5 [PubMed PMID: 10571759]
O'Grady NP, Alexander M, Burns LA, Dellinger EP, Garland J, Heard SO, Lipsett PA, Masur H, Mermel LA, Pearson ML, Raad II, Randolph AG, Rupp ME, Saint S, Healthcare Infection Control Practices Advisory Committee (HICPAC) (Appendix 1). Summary of recommendations: Guidelines for the Prevention of Intravascular Catheter-related Infections. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 2011 May:52(9):1087-99. doi: 10.1093/cid/cir138. Epub [PubMed PMID: 21467014]
Fletcher MA, Brown DR, Landers S, Seguin J. Umbilical arterial catheter use: report of an audit conducted by the Study Group for Complications of Perinatal Care. American journal of perinatology. 1994 Mar:11(2):94-9 [PubMed PMID: 8198665]