Introduction
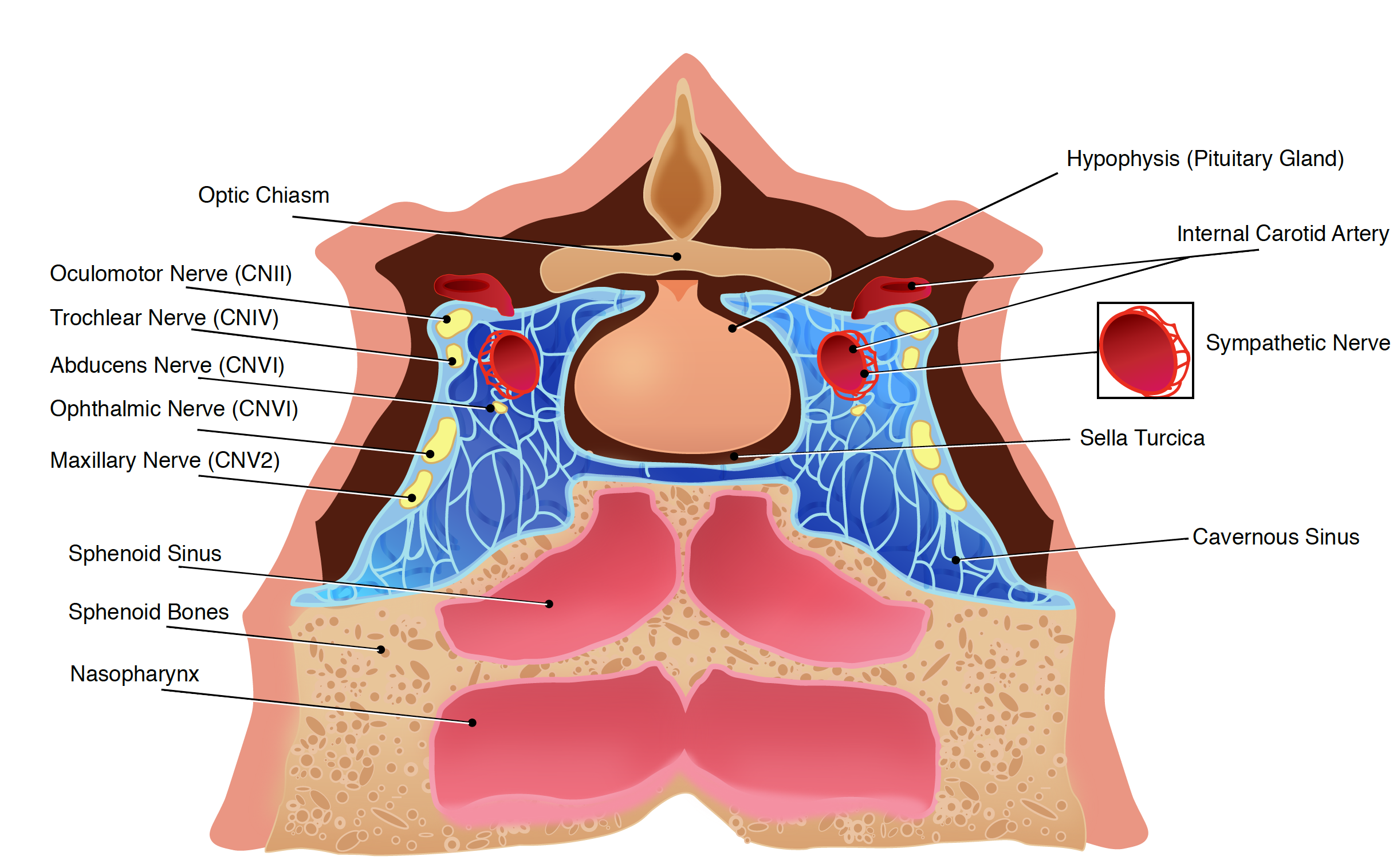
The cavernous sinus is part of the brain’s dural venous sinus and contains multiple neuro-vasculatures. It is situated bilaterally to the sella turcica and extends from the superior orbital fissure anteriorly to the petrous part of the temporal bone posteriorly, and is about 1 cm wide and 2 cm long. The venous blood that flows to the cavernous sinus is from the superior and anterior ophthalmic veins, superficial middle cerebral vein, and sphenoparietal sinus. The communication between the left and right cavernous sinuses is made by the intercavernous sinuses anterior and posterior to the infundibulum of the pituitary gland.[1][2][3]
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
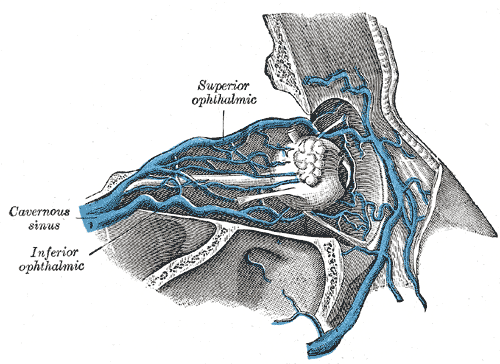
The cavernous sinus works as a conduit. Cranial nerves leaving the brainstem travel through the cavernous sinus before entering the orbit to innervate extraocular and intrinsic eye muscles. Also, different venous tributaries drain into the cavernous sinus. The superior ophthalmic vein collects venous blood from the ethmoidal, vorticose, central retinal, and nasofrontal veins before draining into the anterior part of the cavernous sinus through the superior orbital fissure. The inferior ophthalmic vein, on the other hand, receives blood from the lacrimal sac, eyelids, the inferior rectus and inferior oblique muscles, the vorticose vein, and from the anterior and medial wall of the orbit. It then runs posteriorly toward the lower part of the orbit and divides into two branches. One of these branches joins the cavernous sinus, while the other one drains into the pterygoid plexus. The superficial middle cerebral originates on the lateral surface of the hemisphere, runs in the lateral sulcus, and drains most of the temporal lobe into the cavernous sinus. The sphenoparietal sinus receives blood from some branches of the middle meningeal vein before draining into the cavernous sinus. It is noteworthy to mention that efferent hypophyseal veins also drain into the cavernous sinus. After collecting venous blood from these different veins, the cavernous sinus drains to the superior and inferior petrosal sinuses, which then join the sigmoid sinus to form the internal jugular vein. The internal jugular vein exits the brain through the jugular foramen and connects with the subclavian vein to become the right or left brachiocephalic vein.[4][5][6]
Embryology
Most of the cavernous sinus is formed before birth. It first emerges as a collection of small venous canals consisting of only an endothelial layer. Throughout gestation, these canals gradually expand to form larger structures. In fact, after 13 weeks of gestation, the cavernous sinus appears as a faint cluster of small vessels, whereas after 27 weeks of gestation, the inferior venous pathways suddenly increase in size.
Blood Supply and Lymphatics
The common carotid artery bifurcates in the cervical region and gives rise to the external and internal carotid artery. The internal carotid artery travels superiorly and enters the skull via the carotid canal. After entering the carotid canal, the internal carotid makes a 90-degree turn and travels horizontally in the petrous part of the temporal bone - this is the petrous part of the internal carotid artery. The petrous part of the internal carotid then enters the cavernous sinus via the foramen lacerum. In the cavernous sinus, the internal carotid artery is also referred to as the cavernous part. The cavernous part travels horizontally and anteriorly until it reaches the anterior limit of the sinus, where it curves vertically, exits the sinus superiorly, and becomes the cerebral part of the internal carotid artery. It is important to mention that the cavernous part of the internal carotid artery is the only artery in the body that is surrounded completely by venous blood.
Nerves
The nerves of the cavernous sinus are the oculomotor nerve (CN III), trochlear nerve (CN IV), ophthalmic nerve (V1), maxillary nerve (V2), abducens nerve (CN VI), and the sympathetic plexus around the internal carotid artery.
The CN III exits the midbrain ventrally at the interpeduncular fossa, pierces the dura, and enters the cavernous sinus, where it runs on the roof and lateral wall. After exiting the cavernous sinus, it goes through the superior orbital fossa. Within the superior orbital fossa, it splits into the superior and inferior division.
The CN IV is the only nerve exiting the midbrain dorsally. It originates from the trochlear nerve nucleus; it crosses the midline and emerges inferior to the inferior colliculus, situated in the posterior part of the midbrain. It then travels anteriorly around the midbrain, pierces and enters the dura mater near the tentorium cerebelli, and continues its course in the lateral wall of the cavernous sinus. After exiting the cavernous sinus, it enters the orbit through the superior orbital fissure to innervate the superior oblique muscle.
The ophthalmic nerve (V1) and the maxillary nerve (V2) are divisions of the trigeminal nerve (CN V). The CN V exits the brainstem from the ventrolateral pons and enters the Meckel’s cave, where the trigeminal ganglion lies. The V1 branches of the trigeminal ganglion pass through the inferior part of the cavernous sinus and after exiting the cavernous sinus, they enter the orbit via the superior orbital fissure. Also, the V2 branches of the trigeminal ganglion enter the cavernous sinus and exit the skull via the foramen rotundum.
The CN VI exits the brainstem ventrally at the pontomedullary junction, pierces the dura, and travels the longest intracranial distance of all the cranial nerves. After its long intracranial course, it enters the cavernous sinus, where it is surrounded by venous blood, like the internal carotid artery.
The sympathetic plexus around the internal carotid artery originates from the superior cervical ganglion, travels with the internal carotid artery, enters the skull through the carotid canal, and enters the cavernous sinus through the jugular foramen. Within the cavernous sinus, it gives sympathetic fibers to the CN III and V1.
Surgical Considerations
Performing surgery in the cavernous sinus is challenging given the fact that it contains vital neuronal structures and elevated risk of hemorrhage. Direct exposure of the cavernous sinus is possible, but it is considered to be a morbid procedure, even for experienced neurosurgeons. However, other approaches such as a transorbital pathway may provide found to be less morbid. The transorbital pathway provides less-invasive access to the cavernous sinus. This approach provides the entire lateral wall of the cavernous sinus to be exposed, without entering its neurovascular compartment, while also providing a favorable angle for performing procedures. Also, this angle allows for procedures to be performed without injuring cranial nerves, temporal lobes, or having to open venous spaces, and the procedure has proven to be quick. Although the transorbital pathway is an unfamiliar approach and requires proper equipment for retraction, it has demonstrated to be feasible and safe in more than 1500 orbital decompressions. The transorbital pathway may provide access to the inside of the lateral wall of the cavernous sinus in a minimally invasive manner; however, more surgeries are needed to provide more clinical advantages and disadvantages of this novel approach.[7][8]
Clinical Significance
Cavernous Sinus Syndrome
Cavernous sinus syndrome is a medical emergency and life-threatening disorder that presents with different symptoms depending on what structure is affected. A severe lesion involving the entire sinus will present with total ophthalmoplegia, due to CN III, IV, and VI injury, accompanied with fixed and dilated pupils due to compression of the superficial parasympathetic fibers of the CN III. Cavernous sinus syndrome can lead to Horner’s syndrome. Horner’s syndrome occurs when the sympathetic plexus around the internal carotid is damaged. When CN V1 and CN V2 are involved, sensory loss in the face, scalp, maxilla, nasal cavity, sinuses, and palate occurs. There are several causes of cavernous sinus syndrome, including metastatic tumor, meningioma, pituitary tumor, extension of nasopharyngeal tumors, granulomatous diseases, cavernous sinus thrombosis, and aneurysms of the cavernous part of the internal carotid artery. In case of rupture of a cavernous aneurysm, a carotid-cavernous fistula is created, leading to a pulsating exophthalmos on physical examination.
Facial veins and implication to cavernous sinus infection
Blood from the medial angle of the eye, lips, and nose usually drain via the facial vein. However, blood from these parts may also drain superiorly through the facial vein, to the superior ophthalmic, to the cavernous sinus. By doing so, it provides a pathway for infections from the face to spread to the cavernous sinus and from the sinus to the brain.
Another way for infections to spread from the face to the brain is via the inferior ophthalmic vein. In fact, the inferior ophthalmic vein communicates with the pterygoid plexus of veins, and the pterygoid plexus communicates with the cavernous sinus via the emissary's vein. Gravity dictates the blood flow from the cavernous sinus to the pterygoid plexus; however, in the case of inflammation or obstruction, the pressure gradient can be reversed. Because there are no valves in the brain’s venous sinus, blood will flow from the pterygoid plexus to the cavernous sinus carrying bacteria with it.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Ipsalali HO, Ciftci AC, Kilic D, Sendemir G, Seyhan S, Kaya I, Ortug G. Variations of the 6(th) cranial nerve (nervus abducens) in the petroclival region: A microsurgical study. Morphologie : bulletin de l'Association des anatomistes. 2019 Jun:103(341 Pt 2):103-109. doi: 10.1016/j.morpho.2019.01.001. Epub 2019 Feb 1 [PubMed PMID: 30713002]
Ngnitewe Massa R, Minutello K, Mesfin FB. Neuroanatomy, Cavernous Sinus. StatPearls. 2023 Jan:(): [PubMed PMID: 29083662]
Graffeo CS, Perry A, Copeland WR 3rd, Raghunathan A, Link MJ. Histology of the distal dural ring. Clinical anatomy (New York, N.Y.). 2017 Sep:30(6):742-746. doi: 10.1002/ca.22916. Epub 2017 Jun 12 [PubMed PMID: 28514500]
Patel CR, Fernandez-Miranda JC, Wang WH, Wang EW. Skull Base Anatomy. Otolaryngologic clinics of North America. 2016 Feb:49(1):9-20. doi: 10.1016/j.otc.2015.09.001. Epub [PubMed PMID: 26614826]
Klinger DR, Flores BC, Lewis JJ, Barnett SL. The treatment of cavernous sinus meningiomas: evolution of a modern approach. Neurosurgical focus. 2013 Dec:35(6):E8. doi: 10.3171/2013.9.FOCUS13345. Epub [PubMed PMID: 24289133]
Park HS, Chung MS, Shin DS, Jung YW, Park JS. Whole courses of the oculomotor, trochlear, and abducens nerves, identified in sectioned images and surface models. Anatomical record (Hoboken, N.J. : 2007). 2015 Feb:298(2):436-43. doi: 10.1002/ar.23048. Epub 2014 Sep 22 [PubMed PMID: 25212480]
Duong DK, Leo MM, Mitchell EL. Neuro-ophthalmology. Emergency medicine clinics of North America. 2008 Feb:26(1):137-80, vii. doi: 10.1016/j.emc.2007.11.004. Epub [PubMed PMID: 18249261]
Swanson MW. Neuroanatomy of the cavernous sinus and clinical correlations. Optometry and vision science : official publication of the American Academy of Optometry. 1990 Dec:67(12):891-7 [PubMed PMID: 2082236]