Introduction
The cervical spine is a dynamic structure tasked with protecting nervous innervation to the entire body while also maintaining a range of motion for the head and neck. Fractures of the cervical spine are a leading cause of mobility and mortality in trauma patients, and a bone fracture is associated with 56% of cervical spinal cord injuries. Fractures of the cervical spine can be described based on the level involved and typically divided into three groups: C1, C2 and the sub-axial spine (C3 to C7).[1][2][3]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Fractures of the cervical spine result from abnormal movement or a combination of movements including hyperflexion, hyperextension, rotation, axial loading, and lateral bending of the spinal column.[4]
Epidemiology
Cervical spine fractures may occur in all age groups but are more common in males. Falls account for the most common cause followed by motor vehicle accidents, biking, and diving. Mortality ranges from 5-10%. [5][6]
Pathophysiology
C1 fractures typically result from axial loading. C2 fractures typically occur due to a combination of compression, hyperflexion, and hyperextension. Subaxial cervical spine fracture is commonly seen with high impact accidents such as motor vehicle accidents.[7]
History and Physical
Examination of a patient with cervical spine fractures should begin with a thorough trauma examination of ABCs (check of the airway, breathing, and circulation). Injury to the cervical spine has the potential to compromise respiratory and cardiovascular function and even once stabilized these patients must be closely monitored for the ongoing possibility of changes in the respiratory and cardiovascular function. Next, formal strength and sensation testing of the upper and lower extremities, as well as rectal tone and palpation of the cervical spine should be performed. This is most commonly done following the ASIA scoring system. Acute spinal cord injury is important to identify as early decompression within 24 hours can increase the chance of neurological recovery.
Evaluation
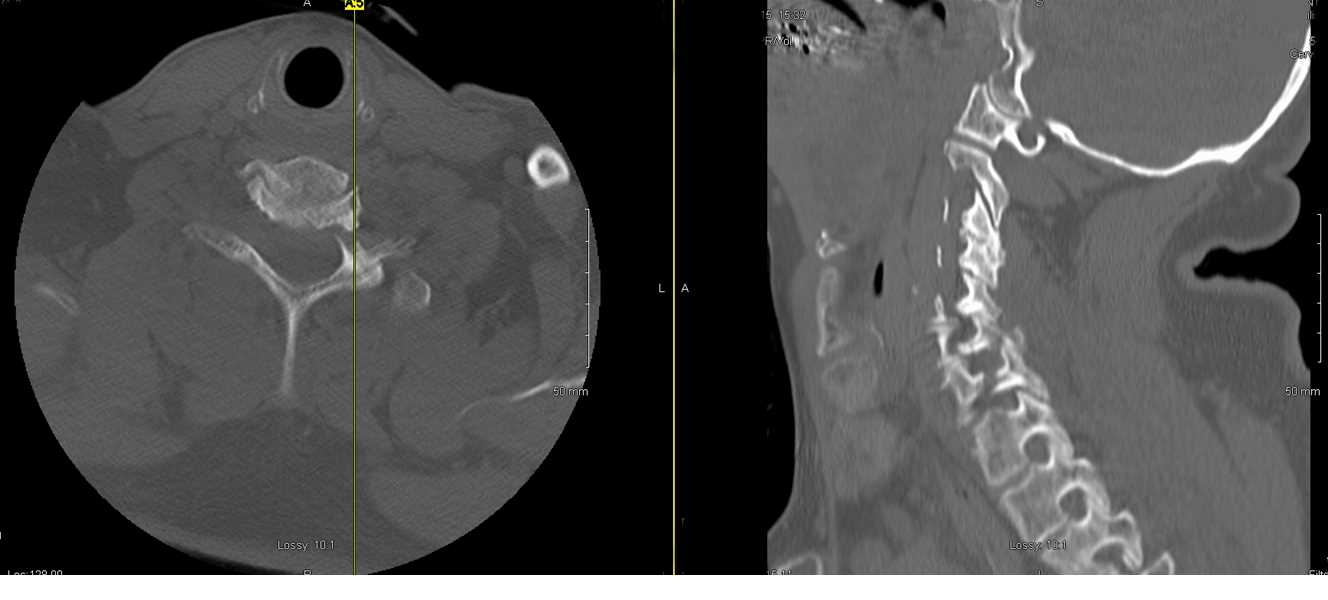
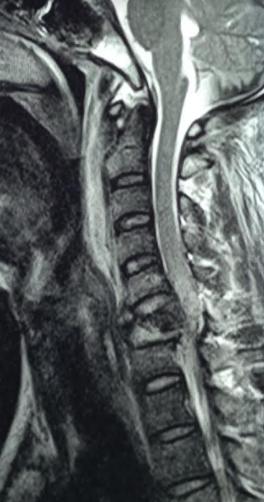
Indications for cervical spine imaging include localized neck pain, deformity, edema, altered mental status, head injury, or neurological deficit. Computed tomography is the preferred imaging in acute spine trauma as it is more sensitive for detection of bony cervical spine injury when compared to plain radiographs (sensitivity of 98% versus 52%). Further evaluation of ligamentous structures of the spinal cord with MRI is important for determining spinal stability and in planning surgical treatment. Scoring systems in dealing with cervical spinal cord injury that includes ligamentous, bony and neurologic injury exist, a common one is called SLICS (Subaxial Cervical Spine Injury Classification System), and this can be used to help with evaluation and guidance of surgical or nonsurgical management. A SLICS score of 1 to 3 is nonsurgical, a score of 4 is not specified, and a score of 5 or greater is a surgical indication. [8][9][10]The scoring system is as follows:
Fracture Morphology
- No abnormality - 0
- Compression endplate disruption or vertebral body fracture - 1
- Burst - 2
- Distraction - 3
- Rotation or translocation - 4
Discoligamentous Complex
- Intact - 0
- Indeterminate - 1
- Disrupted - 2
Neurologic Status
- Intact - 0
- Root injury - 1
- Complete spinal cord injury - 2
- Incomplete spinal cord injury - 3
Continuous Cord Compression
- With neuro deficit - 1
Treatment / Management
Injuries to C1 and C2 compose approximately 30% of cervical spine fractures. Fractures of C1 occur through the lateral mass or arch in single or multiple places (multiple arch fractures, Jefferson fracture). Neurological injury rarely results from an isolated C1 fracture due to abundant space surrounding the spinal cord. C1 fractures may be managed in a rigid cervical collar or halo if the transverse alar ligament (TAL) remains intact on MRI. If the TAL is disrupted C1 to C2 posterior fusion should be considered.[11][12](B2)
C2 fractures can result in a fracture through the body, dens, or pars. If the fracture extends bilaterally through the pars interarticularis, a Hangman fracture is described. Hangman fracture with less than 3mm of displacement and no significant angulation may be treated in a hard cervical collar. If the fracture is displaced greater than 3mm or with greater than 11 degrees of angulation, reduction with halo placement or surgical fixation should be considered. Associated disruption of the C2 to C3 disc with a Hangman fracture requires surgical fixation. Fracture through the C2 dens can be classified as type I, II, or III. Type I is avulsion of the tip of the dens, type II is a fracture through the base of the dens, and type III is a fracture extending into the C2 vertebral body. Type I and III fractures should be treated in a rigid cervical collar or halo. Type II fractures without risk of nonunion can be considered for hard cervical collar or halo. Risk factors for nonunion include 5mm or more of displacement, greater than 10 degrees of angulation, or age older than 50. Type II fractures at risk for nonunion should be considered for odontoid screw placement or posterior C1 to C2 fusion. All fractures of the C1 to C2 complex are considered unstable and should be treated initially with a hard cervical collar, and then evaluated by a spine surgeon.
Subaxial cervical spine fractures follow similar patterns at each level. Compression fractures result in loss of anterior vertebral body height without canal compromise and neural injury. Burst fractures are a variant of compression fractures that result in retropulsion of the vertebral body into the cervical canal. Of note, C7 burst fractures carry a higher risk of developing kyphotic deformity that other levels of the subaxial cervical spine. Teardrop fractures occur with flexion or flexion-extension of the cervical spine leading to an anterior–inferior fracture of the vertebral body. There are also three-column fractures extending through the anterior vertebral body all the way through to the posterior ligaments, and these are highly unstable. Unilateral facet fractures are controversial, but many are highly unstable or can lead to progressive deformity and warrant surgical evaluation. Any fracture extending into the foramina transversarium from C2 to C6 should be evaluated for the possibility of co-occurring vertebral artery injury. Surgical fixation of subaxial cervical spine fractures should take into consideration the SLICS scoring system as previously described.
Clay shoveler’s fractures describe fractures of the cervical spinous processes.[13][14]
Each fracture described should warrant cervical collar placement with surgery indicated for restoration of cervical lordosis, decompression of the spinal cord, or fixation as determined by the instability of ligamentous components.
Differential Diagnosis
- Acute torticollis
- Cauda Equina
- Cervical strain
- Hanging injuries
- Neck trauma
- Septic shocks
- Spinal cord infections
- Spinal cord injuries
- Spinal cord neoplasms
- Vertebral artery dissection
Pearls and Other Issues
Cervical spine fractures are high-risk injuries with the potential for devastating neurological sequelae. Hence, a trained spine specialist should carry out subsequent evaluation and treatment. All patients with cervical fractures should be closely monitored with a follow-up to ensure continued cervical stability and healing. Any fracture extending into the foramina transversarium from C2 to C6 should be evaluated for the possibility of co-occurring vertebral artery injury. This is most often done with computed tomogram (CT) angiogram.
Enhancing Healthcare Team Outcomes
The diagnosis and management of cervical spine fractures usually require an interprofessional team that includes an emergency department physician, radiologist, neurosurgeon/orthopedic surgeon, EMS, and nurses.
Cervical spine fractures are high-risk injuries with the potential for devastating neurological sequelae. Hence, a trained spine specialist should carry out subsequent evaluation and treatment. All patients with cervical fractures should be closely monitored with a follow-up to ensure continued cervical stability and healing. Any fracture extending into the foramina transversarium from C2 to C6 should be evaluated for the possibility of co-occurring vertebral artery injury. This is most often done with a CT angiogram.
Each fracture described should warrant cervical collar placement with surgery indicated for restoration of cervical lordosis, decompression of the spinal cord, or fixation as determined by the instability of ligamentous components.
The outcome of cervical spine fractures depends on the neurological deficit at the time of presentation and concomitant head injury.[15][16]
Media
(Click Image to Enlarge)
References
van Eck CF, Fourman MS, Abtahi AM, Alarcon L, Donaldson WF, Lee JY. Risk Factors for Failure of Nonoperative Treatment for Unilateral Cervical Facet Fractures. Asian spine journal. 2017 Jun:11(3):356-364. doi: 10.4184/asj.2017.11.3.356. Epub 2017 Jun 15 [PubMed PMID: 28670403]
Dhillon CS, Jakkan MS, Dwivedi R, Medagam NR, Jindal P, Ega S. Outcomes of Unstable Subaxial Cervical Spine Fractures Managed by Posteroanterior Stabilization and Fusion. Asian spine journal. 2018 Jun:12(3):416-422. doi: 10.4184/asj.2018.12.3.416. Epub 2018 Jun 4 [PubMed PMID: 29879767]
Daniel RT, Hussain MM, Klocke N, Yandamuri SS, Bobinski L, Duff JM, Bucklen BS. Biomechanical Assessment of Stabilization of Simulated Type II Odontoid Fracture with Case Study. Asian spine journal. 2017 Feb:11(1):15-23. doi: 10.4184/asj.2017.11.1.15. Epub 2017 Feb 17 [PubMed PMID: 28243364]
Level 3 (low-level) evidenceModi JV,Soman SM,Dalal S, Traumatic Cervical Spondyloptosis of the Subaxial Cervical Spine: A Case Series with a Literature Review and a New Classification. Asian spine journal. 2016 Dec; [PubMed PMID: 27994781]
Level 2 (mid-level) evidenceBeckmann NM, Chinapuvvula NR, Zhang X, West OC. Epidemiology and Imaging Classification of Pediatric Cervical Spine Injuries: 12-Year Experience at a Level 1 Trauma Center. AJR. American journal of roentgenology. 2020 Jun:214(6):1359-1368. doi: 10.2214/AJR.19.22095. Epub 2020 Mar 31 [PubMed PMID: 32228329]
Fiedler N, Spiegl UJA, Jarvers JS, Josten C, Heyde CE, Osterhoff G. Epidemiology and management of atlas fractures. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2020 Oct:29(10):2477-2483. doi: 10.1007/s00586-020-06317-7. Epub 2020 Jan 30 [PubMed PMID: 32002697]
Fehlings MG, Tetreault L, Nater A, Choma T, Harrop J, Mroz T, Santaguida C, Smith JS. The Aging of the Global Population: The Changing Epidemiology of Disease and Spinal Disorders. Neurosurgery. 2015 Oct:77 Suppl 4():S1-5. doi: 10.1227/NEU.0000000000000953. Epub [PubMed PMID: 26378347]
Hussain M, Javed G. Diagnostic accuracy of clinical examination in cervical spine injuries in awake and alert blunt trauma patients. Asian spine journal. 2011 Mar:5(1):10-4. doi: 10.4184/asj.2011.5.1.10. Epub 2011 Mar 2 [PubMed PMID: 21386941]
Girotto D, Ledić D, Strenja-Linić I, Peharec S, Grubesić A. Clinical and medicolegal characteristics of neck injuries. Collegium antropologicum. 2011 Sep:35 Suppl 2():187-90 [PubMed PMID: 22220432]
Van Goethem JW, Maes M, Ozsarlak O, van den Hauwe L, Parizel PM. Imaging in spinal trauma. European radiology. 2005 Mar:15(3):582-90 [PubMed PMID: 15696292]
Kopczyński S, Derenda M, Kowalina I, Siwiecki T. [Surgical treatment after cervical spine and spinal cord injuries of the C3-C7 level]. Neurologia i neurochirurgia polska. 2002 Jul-Aug:36(4):669-82 [PubMed PMID: 12418133]
Level 2 (mid-level) evidenceVeres R, Pentelényi T, Turóczy L, Zsolczai S, Major J, Kenéz J. [Early experience with the use of the Halo device in the treatment of damage to the cervical spine]. Magyar traumatologia, orthopaedia es helyreallito sebeszet. 1989:32(1):15-23 [PubMed PMID: 2566717]
Smith RM, Bhandutia AK, Jauregui JJ, Shasti M, Ludwig SC. Atlas Fractures: Diagnosis, Current Treatment Recommendations, and Implications for Elderly Patients. Clinical spine surgery. 2018 Aug:31(7):278-284. doi: 10.1097/BSD.0000000000000631. Epub [PubMed PMID: 29620588]
Stein DM, Knight WA 4th. Emergency Neurological Life Support: Traumatic Spine Injury. Neurocritical care. 2017 Sep:27(Suppl 1):170-180. doi: 10.1007/s12028-017-0462-z. Epub [PubMed PMID: 28913694]
Poorman GW, Segreto FA, Beaubrun BM, Jalai CM, Horn SR, Bortz CA, Diebo BG, Vira S, Bono OJ, DE LA Garza-Ramos R, Moon JY, Wang C, Hirsch BP, Tishelman JC, Zhou PL, Gerling M, Passias PG. Traumatic Fracture of the Pediatric Cervical Spine: Etiology, Epidemiology, Concurrent Injuries, and an Analysis of Perioperative Outcomes Using the Kids' Inpatient Database. International journal of spine surgery. 2019 Jan:13(1):68-78. doi: 10.14444/6009. Epub 2019 Feb 22 [PubMed PMID: 30805288]
Ye IB, Girdler SJ, Cheung ZB, White SJ, Ranson WA, Cho SK. Risk Factors Associated with 30-Day Mortality After Open Reduction and Internal Fixation of Vertebral Fractures. World neurosurgery. 2019 May:125():e1069-e1073. doi: 10.1016/j.wneu.2019.01.247. Epub 2019 Feb 18 [PubMed PMID: 30790742]