Introduction
Clonus is a rhythmic, oscillating, stretch reflex, the cause of which is not totally known; however, it relates to lesions in upper motor neurons and therefore is generally accompanied by hyperreflexia. Therefore, clonus is used as part of the neurological physical exam to evaluate the status of a patient’s nervous system. It can be evaluated in many joints but is most commonly seen in the ankle joint by briskly dorsiflexing the foot. An illustrative example of what clonus might look like is a clinician tapping the patellar tendon once lightly and a subsequent series of obvious repeated knee extensions and relaxations going on for a dozen beats. The test is free of cost, generally requires no equipment and can be performed rapidly and easily in a hospitalized patient. Like other signs of upper motor neuron syndrome clonus indicates some insult to the central rather than peripheral nervous system, so part of its utility as a clinical examination skill is in differentiating the two. It has other roles, for instance, it is prognostic of seizures in certain drug overdoses and therefore can be used to decide when to treat this condition prophylactically.
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
The precise pathophysiology behind clonus is not known, but there are 2 leading theories.[1][2] In one, clonus is caused by a self-perpetuating reactivation of peripheral muscle stretch circuits, with each beat producing the next. On the other, there is an initial appropriate external stimulus that leads to activation of the stretch reflex circuit followed by a central signal which commands the muscles to continue to produce that motor response in the absence of an appropriate stimulation of the stretch reflex. A complete explanation may be a combination of the 2 theories.[2]
Hyperexcitability in muscle stretch circuits is produced when there is less tonic inhibition of motor neurons involved in the monosynaptic stretch reflex. This can occur when there is a lesion to descending motor nerves, predominantly the dorsal reticulospinal pathway, which can occur anywhere from the cortex to the spinal cord. The inhibitory dampening effect of these descending nerves on alpha and gamma motor neurons is removed, leading to a hyper excitatory state in the muscle stretch reflex circuit. Therefore, clonus is considered a manifestation of upper motor neuron pathology and this explains why other signs of hyperreflexia generally accompany it.
The rhythm of a given joint's clonus is defined by the nervous anatomy involved in that joint's stretch reflex. The longer the nerves involved, the longer it takes for a signal to be conducted to the spine and back out to the periphery, and therefore the longer the time between beats. For example, the wrist or fingers will oscillate at a higher frequency (shorter interval between beats) than the ankle which is significantly further from the spine.
The most common site to test for clonus is in the ankle/Achilles reflex (S1/S2 nerve routes). Some other commonly tested clonus reflexes include the[1]:
- Jaw jerk/masseter: Trigeminal nerve, tested at the chin/mental protuberance
- Patellar/quadriceps/knee: L2 to L4 (mostly L4), tested just inferior to the patella (or by pushing patella distally)
- Biceps: C5 to C6, just anterior to the elbow
- Triceps: C7 to C8 (mostly C7), just posterior to the elbow
Equipment
One of the appealing aspects of clonus as a physical examination technique is that it can easily be performed without equipment. As it is most commonly tested at the ankle, with swift dorsiflexion of the entire foot, no equipment is required. Elsewhere, when testing other joints, for instance, the knee, the patellar tendon can be struck briskly with the fingers, or an improvised object like a stethoscope, or phone. However, as clonus is a mark of hyperreflexia, it is generally easy to elicit in a patient without much force, so the examiner’s fingers may even be preferred over other equipment.[3] If desired, a reflex hammer of any type would be adequate equipment to test this reflex.
Technique or Treatment
Eliciting the clonus reaction can be done in the same manner as eliciting a muscle stretch reflex, which involves tapping the tendon of the joint when it is in a relaxed position often at ninety degrees of flexion (see MSR Statpearls article for a more detailed description of these techniques).[3] This article will focus on the clonus specific reflex maneuvers at the knee and ankle. In these cases, the examiner maintains sustained pressure on the joint which allows the clonus to be appreciated through tactile feedback and helps elicit this response.
For the ankle this involves allowing the patient to relax with a passively flexed ankle to about ninety degrees and a passively flexed knee if possible; this usually involves the examiner supporting the leg with the hand not performing clonus. Next, at the ankle, the examiner places their hand on the dorsum of the patient’s forefoot and briskly dorsiflexes it, after which the examiner continues to maintain dorsiflexion pressure. It is against this pressure that the clonus beats will be felt, and the rhythm and number of beats can be appreciated. Each beat will be felt as a plantarflexion followed by a relaxation. The initial beat is the longest, with decreasing duration of beats until the fourth beat, after which the beat frequency becomes equivalent from one to the next.[1] The initial brisk dorsiflexion and sustained pressure are sometimes done with slight eversion of the foot.
At the knee, the process is somewhat similar, but the positioning is different. The knee should be completely extended (passively) with the thigh and leg muscles completely relaxed. Then the patella is briskly moved distally using the examiner’s fingers, and a light pressure is maintained in the distal direction. Each beat of clonus will be felt as a proximal movement of the patella followed by relaxation.
Clinical Significance
Clonus can be physiologic, for instance, term infants can be hyperreflexic, and a few beats of clonus can be a normal finding in this population; however, most infants will not exhibit this finding, and most infants who will go on to demonstrate cerebral palsy will not exhibit clonus.[4] In adults, it is generally pathological. If greater than 10 beats, it is considered "sustained clonus," which is sometimes denoted as a "5" when evaluating reflexes, or just documented in the text along with a rating of "4" which is otherwise the highest the reflex scale goes.
Clonus exists as a physical examination finding, but also as pathology in those with the condition. There is a range of impact on daily life among those with the condition, ranging from somewhat debilitating to a minor annoyance.[5] As a physical examination finding, clonus is a marker of hyperreflexia, which is part of an upper motor neuron syndrome. Therefore, it is generally accompanied by other upper motor neuron signs including positive signs like spasticity, and negative signs like weakness (which is also a lower motor neuron sign).[6] These signs, especially when taken together in the right context, signal central nervous system insult, which can come in many varied forms, to only name a few: vascular (stroke), infectious (encephalopathy), congenital (cerebral palsy), autoimmune (multiple sclerosis), traumatic (spinal cord insult). Another significant category of pathology which can manifest as clonus would be iatrogenic or toxicological. Clonus is often evaluated in suspected serotonin syndrome, which can be brought on by many drugs including psychiatric (monoamine oxidase inhibitor, selective serotonin reuptake inhibitor, serotonin-norepinephrine reuptake inhibitor, tricyclic antidepressant) or street drugs (cocaine, ecstasy, amphetamines) to name a few. Clonus has been identified as an effective way to predict seizures in patients who have overdosed on tramadol which is an SNRI.[7]
Enhancing Healthcare Team Outcomes
Part of what makes clonus a useful assessment is how quickly and easily it can be performed without specialized equipment or added cost. The test can be performed by nurses, medical students, the primary caregiver, or the specialist. It is commonly used to evaluate patients for which there is a concern for upper motor neuron syndrome, for instance, in patients at risk of stroke. Many types of clinicians are trained to perform clonus including nurses and physicians. The clearest way to document clonus findings is to explain what was found and how it was performed, but often, simply noting that reflexes are "4" or "5" is adequate.
If clonus is discovered on the physical exam, the nurse practitioner or primary care provider should refer the patient to a neurologist for further investigation. In addition, a pharmacist should be consulted to evaluate drugs as an underlying cause. Once the etiology is determined, and a course of action undertaken, the interprofessional team will communicate to monitor for a successful outcome. [Level V]
Media
(Click Image to Enlarge)
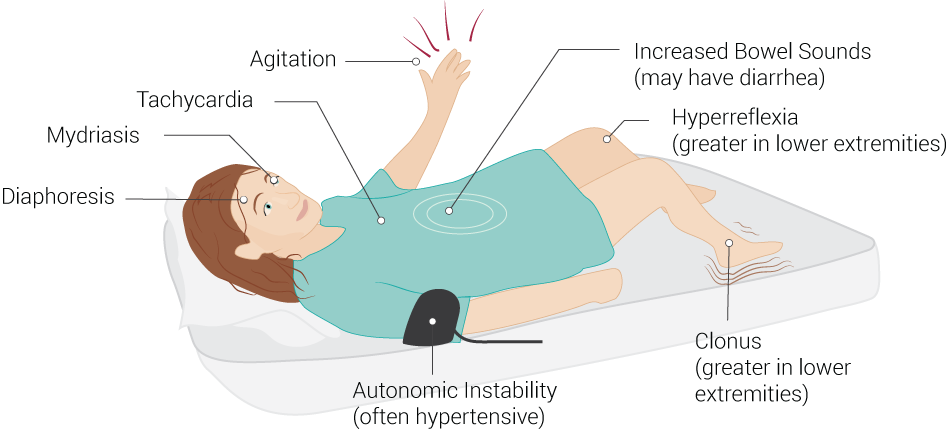
Common Signs of Serotonin Syndrome. Serotonin syndrome signs include increased bowel sounds (may have diarrhea), hyperreflexia (greater in lower extremities), clonus (greater in lower extremities), autonomic instability (often hypertensive), diaphoresis, mydriasis, tachycardia, and agitation.
Contributed by B Palmer
(Click Video to Play)
Clinical Examination of Ankle Clonus. Clinical examination of ankle clonus is typically demonstrated in upper motor neuron lesions or serotonin syndrome.
Contributed by RS Menon, MD
References
Boyraz I, Uysal H, Koc B, Sarman H. Clonus: definition, mechanism, treatment. Medicinski glasnik : official publication of the Medical Association of Zenica-Doboj Canton, Bosnia and Herzegovina. 2015 Feb:12(1):19-26 [PubMed PMID: 25669332]
Beres-Jones JA, Johnson TD, Harkema SJ. Clonus after human spinal cord injury cannot be attributed solely to recurrent muscle-tendon stretch. Experimental brain research. 2003 Mar:149(2):222-36 [PubMed PMID: 12610691]
Zimmerman B, Hubbard JB. Deep Tendon Reflexes. StatPearls. 2023 Jan:(): [PubMed PMID: 30285397]
Hamer EG,La Bastide-Van Gemert S,Boxum AG,Dijkstra LJ,Hielkema T,Jeroen Vermeulen R,Hadders-Algra M, The tonic response to the infant knee jerk as an early sign of cerebral palsy. Early human development. 2018 Apr [PubMed PMID: 29549793]
Mummidisetty CK, Bohórquez J, Thomas CK. Automatic analysis of EMG during clonus. Journal of neuroscience methods. 2012 Feb 15:204(1):35-43. doi: 10.1016/j.jneumeth.2011.10.017. Epub 2011 Oct 26 [PubMed PMID: 22057220]
Ivanhoe CB, Reistetter TA. Spasticity: the misunderstood part of the upper motor neuron syndrome. American journal of physical medicine & rehabilitation. 2004 Oct:83(10 Suppl):S3-9 [PubMed PMID: 15448572]
Najari F, Alizadeh-Ghamsari A, Vahabzadeh M, Dadpour B, Reza Mousavi S, Baradaran Kayal I. A Study of the Importance of Clonus Symptoms in Patients with Tramadol Poisoning. Journal of toxicology. 2017:2017():2151536. doi: 10.1155/2017/2151536. Epub 2017 Oct 11 [PubMed PMID: 29158734]
