Introduction
Cor triatriatum is a rare condition when a child is born with a thin, fibro-muscular membrane subdividing the left or right atrium into 3 chambers (see Image. Cor Triatriatum). The condition is also classified as a congenital heart defect. Cor triatriatum sinister is the most common form. The left atrium divides via an atrial appendage into an upper and a lower chamber. The upper chamber receives blood from the pulmonary veins. In contrast, the lower chamber is attached to the left atrial appendage, blocking the mitral valve orifice and creating a significant left ventricular inflow obstruction. The presence of the left atrial appendage differentiates cor triatriatum from another congenital heart defect, supravalvular mitral stenosis.[1]
Another more rare form of cor triatriatum is cor triatriatum dextrum. With cor triatriatum dextrum, the right valve of the sinus venosus persists, dividing the right atrium into 2 chambers. This form presents similarly to the Ebstein anomaly and is difficult to differentiate.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Cor triatriatum results from the incomplete absorption of the common pulmonary vein, which is normally reabsorbed during the development of a fetus and becomes a part of the left atrium. The incomplete absorption results in the formation of an appendage that subdivides the left atrium into 2 chambers. No known genetic mutations or risk factors are found to be associated with the development of this condition.
Epidemiology
Cor triatriatum is associated with other congenital cardiac defects, such as tetralogy of Fallot, atrial septal defect, ventricular septal defect, and partial anomalous pulmonary venous connection, and represents only 0.1% to 0.4% of all congenital abnormalities.[2] The membrane may be complete or contain 1 or more fenestrations of differing sizes.
Pathophysiology
A malincorporation theory[3] presented by Dr. Clifford G. Parsons explains how cor triatriatum sinister occurs. During normal fetal development, the pulmonary vein incorporates into the left atrium. If it fails to do so, the common pulmonary venous ostium remains narrow, resulting in a septum-like structure called the atrial appendage. The appendage then further divides the left atrium into 2 compartments. Although widely accepted, this theory fails to explain how fossa ovalis and atrial muscle fibers are also present in the proximal atrial chamber.[4]
Two other theories, malseptation and entrapment, also explain the pathophysiology of cor triatriatum. The malseptation theory states that the fibro-muscular membrane is an abnormal growth of the septum primum. In contrast, the entrapment theory emphasizes the entrapment of the common pulmonary vein in the embryonic sinus venosus, thereby preventing its incorporation into the left atrium. The malincorporation theory remains the most widely accepted theory.
History and Physical
Classically, cor triatriatum presents in infancy with signs and symptoms of pulmonary hypertension and pulmonary venous obstruction. Due to low cardiac output, children can show poor growth and weight gain, feeding difficulties, respiratory distress, and tet spells. In childhood and adulthood, the signs and symptoms of pulmonary venous hypertension and right heart failure dominate as the membrane calcifies and the opening becomes smaller and smaller, decreasing cardiac output even further. Mitral valve regurgitation and atrial fibrillation impose serious dangers. Most patients present with the following features[5]:
- Dyspnea and orthopnea
- Easy fatigability
- Hemoptysis
- Exercise intolerance and shortness of breath
- Palpitations
Atrial fibrillation can cause systemic thromboembolism and present as pulmonary embolism or stroke. The left atrial enlarges due to the backing up of blood and can present as life-threatening arrhythmias.
Cor triatriatum sinister that presents for the first time in adulthood is rare but possible. It presents similarly to mitral stenosis, but the absence of loud S1 and an opening snap helps to distinguish between the 2. Chest x-ray showing pulmonary congestion with an absence of left atrial enlargement is characteristic of cor triatriatum. A continuous gradient on Doppler echocardiography confirms the diagnosis.[4][6]
Physical Exam
The physical exam findings are due to right heart failure and pulmonary congestion.
- Accentuated pulmonary component of second heart sound
- A soft mid-systolic murmur at the upper left sternal border with a wide and fixed splitting of an atrial septal defect.
- Right ventricular heave
- Rales at the lung base
- Diminished peripheral pulses
- Hepatomegaly and right upper quadrant tenderness
- Ascites
- Peripheral edema
- Distended peripheral veins
- Distended jugular venous and elevated jugular venous pressure
- Pallor
- Poor weight gain
Evaluation
The mainstay of evaluation and diagnosis includes imaging studies such as chest x-rays, electrocardiography, echocardiography, angiography, and left and right heart catheterization.[7][8]
Chest X-Ray
A chest x-ray is the initial investigation of choice. The findings include:
- Pulmonary congestion with haziness (Kerley B-lines)
- Ground glass appearance of acute pulmonary edema
- Prominent pulmonary vessels
- Pleural effusion
- Left atrial enlargement
- Cardiomegaly
Electrocardiography
Electrocardiography findings are non-specific in cor triatriatum. It can range from atrial fibrillation and no specific P-wave changes to right axis deviation due to pulmonary congestion and right ventricular hypertrophy.
Echocardiography
Echocardiography is the diagnostic modality of choice as it not only allows for definitive diagnosis, but the 3-dimensional reconstruction of echocardiographic images pinpoints the exact location of the defect and appendage and helps direct the surgical approach to the disease. The left atrial appendage and its fenestrations can be easily visualized with an atrial septal defect, pulmonary stenosis, mitral valve stenosis, or regurgitation. Pulmonary arterial and venous drainage patterns can also be seen on echocardiography. Echocardiography differentiates between cor triatriatum and supravalvular mitral stenosis by clearly visualizing the left atrial appendage in the left atrium.
Transesophageal echocardiography outlines the precise nature and anatomy of the defect, especially in older patients, but transthoracic echocardiography can be performed if unavailable.[9][10]
Angiography
Angiography helps determine the severity of obstruction and the time of surgical intervention needed.
Treatment / Management
Medical Management
Asymptomatic Patients
Asymptomatic patients need no specific treatment. Observe the patients for the development of signs and symptoms. Schedule regular medical follow-ups.
Symptomatic Patients
Treatment options for symptomatic patients include medical/conservative management and surgical repair. Medical treatment includes:
- Hemodynamic stabilization of fluid overload and pulmonary edema
- Rate and rhythm control and anticoagulation for patients with atrial fibrillation
- Thromboembolic prophylaxis with anticoagulation against deep vein thrombosis, pulmonary embolism, and stroke
- Obtain surgical consultation
Surgical Management
Surgery is the definitive treatment. Complete surgical resection of the atrial appendage/accessory membrane through a midline sternotomy under cardiopulmonary bypass and closure of the atrial septum with a pericardial patch provides the optimum cure. The 10-year survival rate following surgery is 83%, while patients with coexisting congenital heart diseases have a greater risk of adverse outcomes and a lower survival rate.[11][12](B2)
Differential Diagnosis
Many congenital heart diseases can present similarly to cor triatriatum and should be taken into consideration when making a diagnosis of this disorder. These include:
- Supravalvular mitral stenosis
- Mitral stenosis
- Idiopathic pediatric pulmonary arterial hypertension
- Pulmonary venous hypertension
- Total anomalous pulmonary venous return
- Partial anomalous pulmonary venous return
- Atrial septal defect/ ventricular septal defect
- Ventricular septal defect
- Idiopathic pulmonary hypertension
- Tricuspid stenosis
- Atrial myxoma
An experienced surgical team should evaluate imaging results, as high suspicion can accelerate diagnosis and delay or prevent unfavorable outcomes.
Complications
Complications of cor triatriatum include:
- Right-sided failure
- Pulmonary edema/hypertension
- Atrial arrhythmias
- Death
Deterrence and Patient Education
Clinicians involved in the care of cor triatriatum include:
- Pediatric cardiologist
- Pediatric cardiac surgeon
- Intensivist
Enhancing Healthcare Team Outcomes
Diagnosing and treating cor-triatriatum requires an interprofessional approach. Cor-triatriatum is a very rare congenital heart disorder. However, most infants are symptomatic at birth and need neonatal intensive care unit (NICU) care. Nurses are vital in monitoring these infants, both pre and post-surgery. The infants need to be monitored for arrhythmias, pulmonary edema, or right heart failure. The outcomes for untreated infants are poor. The outcomes for other infants with cor triatriatum depend on the presence of other co-existing heart defects. For those with only the cor triatriatum defect, the outcomes are excellent. The surgery is best done at centers with experience with this disorder. While it appears that only the accessory membrane needs to be resected, the small size of the left atrium and the collapse of the structure during cardiopulmonary bypass can make visualization difficult.[11][13]
Media
(Click Image to Enlarge)
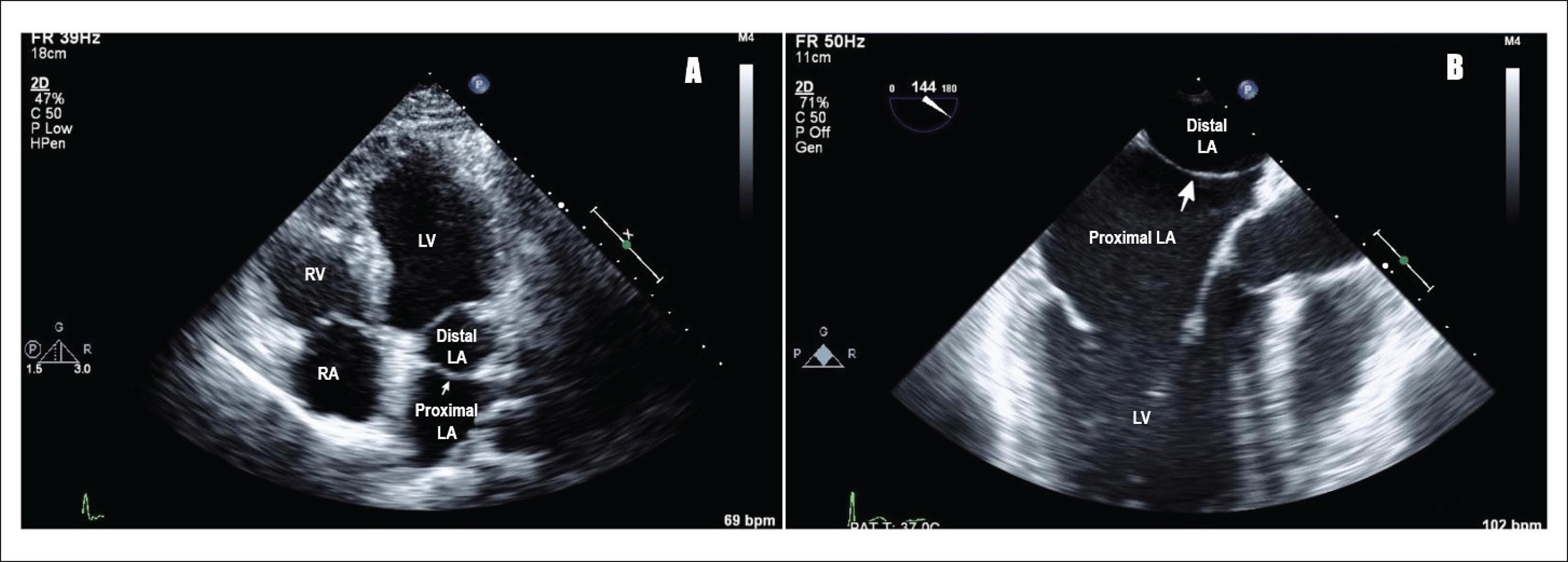
Cor Triatriatum. A) Transthoracic echocardiogram showing cor triatriatum: proximal and distal left atrium separated by a membrane (pointing white arrow), LA (left atrium), LV (left ventricle), RV (right ventricle), RA (right atrium). B) Transesophageal echocardiogram showing cor triatriatum: proximal and distal left atrium separated by a membrane (pointing white arrow), LA (left atrium), and LV (left ventricle).
Raheja H, Namana V, Moskovits N, Hollander G, Shani J. Cor triatriatum sinistrum. Arq. Bras. Cardiol. 2018;110(1). doi: 10.5935/abc.20170138. CC license 4.0.
References
Jha AK, Makhija N. Cor Triatriatum: A Review. Seminars in cardiothoracic and vascular anesthesia. 2017 Jun:21(2):178-185. doi: 10.1177/1089253216680495. Epub 2017 Apr 19 [PubMed PMID: 27913770]
Nassar PN, Hamdan RH. Cor Triatriatum Sinistrum: Classification and Imaging Modalities. The European journal of cardiovascular medicine. 2011 Jan:1(3):84-87 [PubMed PMID: 22379596]
PARSONS CG. Cor triatriatum; concerning the nature of an anomalous septum in the left auricle. British heart journal. 1950 Oct:12(4):327-38 [PubMed PMID: 14777837]
Narayanapillai J. Cor triatriatum sinister with severe obstruction: a rare presentation in an adult. BMJ case reports. 2016 Aug 5:2016():. doi: 10.1136/bcr-2016-215718. Epub 2016 Aug 5 [PubMed PMID: 27495175]
Level 3 (low-level) evidenceHumpl T, Reineker K, Manlhiot C, Dipchand AI, Coles JG, McCrindle BW. Cor triatriatum sinistrum in childhood. A single institution's experience. The Canadian journal of cardiology. 2010 Aug-Sep:26(7):371-6 [PubMed PMID: 20847964]
Level 2 (mid-level) evidenceChen Q, Guhathakurta S, Vadalapali G, Nalladaru Z, Easthope RN, Sharma AK. Cor triatriatum in adults: three new cases and a brief review. Texas Heart Institute journal. 1999:26(3):206-10 [PubMed PMID: 10524744]
Level 3 (low-level) evidenceOstman-Smith I, Silverman NH, Oldershaw P, Lincoln C, Shinebourne EA. Cor triatriatum sinistrum. Diagnostic features on cross sectional echocardiography. British heart journal. 1984 Feb:51(2):211-9 [PubMed PMID: 6691871]
Level 3 (low-level) evidenceThakrar A, Shapiro MD, Jassal DS, Neilan TG, King ME, Abbara S. Cor triatriatum: the utility of cardiovascular imaging. The Canadian journal of cardiology. 2007 Feb:23(2):143-5 [PubMed PMID: 17311121]
Level 3 (low-level) evidenceHamdan R, Mirochnik N, Celermajer D, Nassar P, Iserin L. Cor Triatriatum Sinister diagnosed in adult life with three dimensional transesophageal echocardiography. BMC cardiovascular disorders. 2010 Oct 28:10():54. doi: 10.1186/1471-2261-10-54. Epub 2010 Oct 28 [PubMed PMID: 21029431]
Level 3 (low-level) evidenceSlight RD, Nzewi OC, Mankad PS. Echocardiographic diagnosis of cor triatriatum sinister in the adult. Heart (British Cardiac Society). 2004 Jan:90(1):63 [PubMed PMID: 14676245]
Level 3 (low-level) evidenceFuchs MM, Connolly HM, Said SM, Egbe AC. Outcomes in patients with cor triatriatum sinister. Congenital heart disease. 2018 Jul:13(4):628-632. doi: 10.1111/chd.12624. Epub 2018 Jul 22 [PubMed PMID: 30033682]
Ozyuksel A, Yildirim O, Avsar M, Hayirlioglu M, Demiroluk S, Kucukosmanoglu O, Bilal MS. Surgical correction of cor triatriatum sinister in the paediatric population: mid-term results in 15 cases. European journal of cardio-thoracic surgery : official journal of the European Association for Cardio-thoracic Surgery. 2015 Jan:47(1):e25-8. doi: 10.1093/ejcts/ezu390. Epub 2014 Oct 13 [PubMed PMID: 25312520]
Level 2 (mid-level) evidenceAn G, Zhang H, Zheng S, Wang W, Ma L. Mid-term Outcomes of Common Congenital Heart Defects Corrected Through a Right Subaxillary Thoracotomy. Heart, lung & circulation. 2017 Apr:26(4):376-382. doi: 10.1016/j.hlc.2015.05.028. Epub 2016 Feb 17 [PubMed PMID: 27876287]