Definition/Introduction
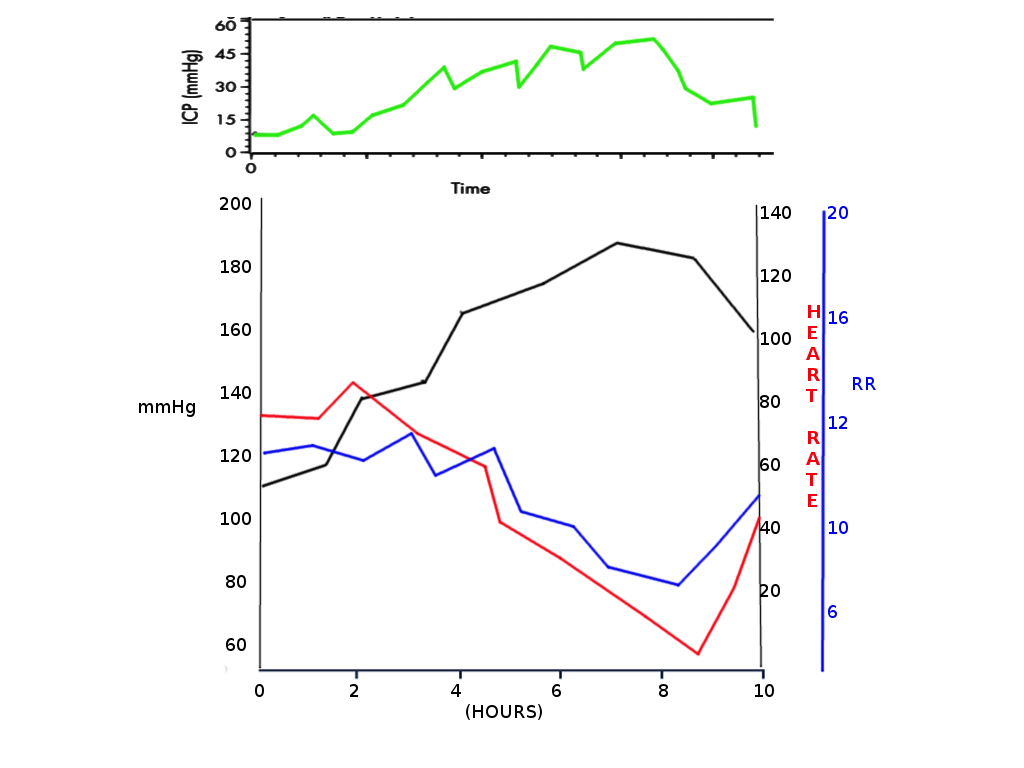
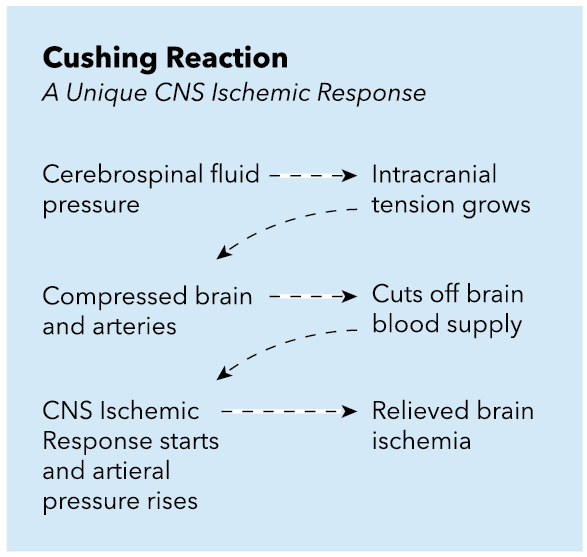
The Cushing reflex (vasopressor response, Cushing reaction, Cushing effect, and Cushing phenomenon) is a physiological nervous system response to acute elevations of intracranial pressure (ICP), resulting in Cushing’s triad of widened pulse pressure (increasing systolic, decreasing diastolic), bradycardia, and irregular respirations. The Cushing reflex was proposed in 1901 by Dr. Harvey Cushing. He believed that the dramatic increase in blood pressure was a reflex to brainstem ischemia seen in patients with increasing ICP from causes such as intracranial hemorrhage, a mass effect from a tumor, and cerebral edema, to name a few. In cases of increased ICP, cerebral perfusion pressure (CPP) drops as the systolic blood pressure cannot overcome the resistance present in the brain. CPP is the pressure that pushes blood through the cerebrovascular network and is defined by the difference between mean arterial pressure (MAP) and intracranial pressure (ICP).[1]
With an acute intracranial pathology that causes a mass effect and increased resistance in intracranial vessels, the only way for the body to perfuse intracranial tissue is through elevating the MAP to restore baseline CPP. Dr. Cushing proposed that systemic vasoconstriction and subsequent rise in systemic blood pressure was a mechanism to overcome increased resistance in the brain, increase the CPP, and prevent further ischemia in the brain.[2]
Issues of Concern
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Issues of Concern
Intracranial pressure and cerebral blood flow are determined by the amount of blood and cerebrospinal fluid (CSF) in the skull and the force exerted by the brain on the inside of the skull. As necessary, autoregulatory mechanisms enable the CSF movement between the brain and spinal subarachnoid space and constriction and dilation of arterioles to maintain ICP within a normal range (5 mmHg to 15 mmHg). Although daily activities such as breathing, coughing, and lifting can cause transient pressure, autoregulatory mechanisms can respond to such changes (so long as mean arterial pressure (MAP) remains between 50 mmHg to 150 mmHg) and maintain ICP within a normal range.
An increase in intracranial pressure most commonly occurs due to the presence of a space-occupying lesion (e.g., intracranial hemorrhage, hematoma, tumor, or abscess). However, it may also result from cerebral edema (e.g., due to head injury, hypoxic or ischemic encephalopathy, postoperative edema, or ischemic stroke with vasogenic edema), metabolic disorders (e.g., hyponatremia, uremic or hepatic encephalopathy), increased CSF production (e.g., choroid plexus tumor), decreased CSF drainage (e.g., due to flow obstruction by space-occupying lesion, aqueductal stenosis, or Chiari malformation), increased venous pressure (e.g., due to cerebral venous sinus thrombosis, jugular vein obstruction or thrombosis, or heart failure), idiopathic intracranial hypertension, or pseudotumor cerebri.
The Cushing reflex is a physiological nervous system response to acute elevations of intracranial pressure (ICP), resulting in the Cushing triad of widened pulse pressure (increasing systolic, decreasing diastolic) bradycardia, and irregular respirations. In the first stage of the Cushing reflex, blood pressure and heart rate rise in response to sympathetic activation to overcome increases in ICP.[3] This sympathetic response allows for brain perfusion as long as the ICP is not too high to overcome. For the brain to remain adequately perfused, mean arterial pressure (MAP) must be maintained higher than ICP. In the second stage of the Cushing reflex, hypertension continues to be present, but the patient becomes bradycardic rather than tachycardic. There are differing opinions on the mechanisms leading to this stage of the Cushing reflex. The prior thinking was that increased blood pressures lead to activation of baroreceptors in the aortic arch, triggering parasympathetic activation and resultant bradycardia. Tsai et al. proposed that chemoreceptors outside the brain do not participate in this stage, and bradycardia actually results from compression of the intracranial vagal nerve.[4][5][6]
It is still not wholly agreed upon as to what causes bradycardia, but there is now a wide acceptance that this is a late-stage and likely terminal sign of worsening intracranial pathology. Blood pressure will continue to rise until the MAP overcomes the ICP, and blood can adequately perfuse the brain, thereby resolving hypoxia and avoiding infarction. In the later stages of the Cushing reflex, brainstem dysfunction secondary to increased ICP, tachycardia, or bradycardia is observable clinically as an irregularity in breathing; this is characterized initially by shallow breaths with occasional periods of apnea. This activity occurs due to compression of the brainstem by increased ICP, and as a result, distortion of the respiratory centers.[4] Eventually, agonal breathing may develop as herniation of the brain begins, progressing to respiratory and cardiac arrest. Overall, it seems that the Cushing reflex is the very last hemodynamic response to a systemic sympathetic activation that follows the acute rise in ICP.[7]
Clinical Significance
As a result of the Cushing reflex, the Cushing triad is typically observed in the later stages of acute head injury. Although the reflex is a homeostatic response by the body in an attempt to rescue under-perfused brain tissues, the Cushing triad is, unfortunately, a late sign of increasing ICP and indicative that brainstem herniation is imminent. Patients who present to the emergency department with concerns for increased ICP and two of three signs of the Cushing reflex have been found to have almost two-fold higher mortality than patients with normal and stable vital signs. It is, therefore, important to recognize early signs of elevated ICP (e.g., a headache, nausea, vomiting, altered level of consciousness) to intervene as early as possible.[8] Many clinicians use the presence of bradycardia and hypertension as an indication of increased ICP; however, this signals a late-stage Cushing reflex that carries a poor prognosis for the patient. Moving into the future, it may be wise to look for the presence of tachycardia and hypertension in patients with suspected intracranial pathology so that interventions can start promptly.[9]
Cushing reflex is most usually an irreversible condition with a terminal prognosis for the patient. Initial emergency treatments aim to lower the ICP rapidly and include: Elevation of the patient’s head 30 to 45 degrees, mannitol and/or furosemide, which act as an osmotic diuretic, induced hyperventilation, steroids, or cerebrospinal fluid drainage.[10]
Nursing, Allied Health, and Interprofessional Team Interventions
The nurses looking after the neurosurgical patient in the ward or intensive care unit should be aware of the Cushing reflex, and they should bring any abnormal findings to the immediate attention of the attending and other clinicians.
Media
References
Smith M. Cerebral perfusion pressure. British journal of anaesthesia. 2015 Oct:115(4):488-90. doi: 10.1093/bja/aev230. Epub 2015 Jul 18 [PubMed PMID: 26188341]
Wan WH, Ang BT, Wang E. The Cushing Response: a case for a review of its role as a physiological reflex. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia. 2008 Mar:15(3):223-8. doi: 10.1016/j.jocn.2007.05.025. Epub 2008 Jan 7 [PubMed PMID: 18182296]
Level 3 (low-level) evidenceGrady PA, Blaumanis OR. Physiologic parameters of the Cushing reflex. Surgical neurology. 1988 Jun:29(6):454-61 [PubMed PMID: 3375974]
Level 3 (low-level) evidenceTsai YH, Lin JY, Huang YY, Wong JM. Cushing response-based warning system for intensive care of brain-injured patients. Clinical neurophysiology : official journal of the International Federation of Clinical Neurophysiology. 2018 Dec:129(12):2602-2612. doi: 10.1016/j.clinph.2018.09.010. Epub 2018 Sep 21 [PubMed PMID: 30453271]
Pirahanchi Y, Bordoni B. Anatomy, Head and Neck: Carotid Baroreceptors. StatPearls. 2023 Jan:(): [PubMed PMID: 30725908]
Lau EO, Lo CY, Yao Y, Mak AF, Jiang L, Huang Y, Yao X. Aortic Baroreceptors Display Higher Mechanosensitivity than Carotid Baroreceptors. Frontiers in physiology. 2016:7():384. doi: 10.3389/fphys.2016.00384. Epub 2016 Aug 31 [PubMed PMID: 27630578]
Schmidt EA, Despas F, Pavy-Le Traon A, Czosnyka Z, Pickard JD, Rahmouni K, Pathak A, Senard JM. Intracranial Pressure Is a Determinant of Sympathetic Activity. Frontiers in physiology. 2018:9():11. doi: 10.3389/fphys.2018.00011. Epub 2018 Feb 8 [PubMed PMID: 29472865]
Bhandarkar P, Munivenkatappa A, Roy N, Kumar V, Samudrala VD, Kamble J, Agrawal A. On-admission blood pressure and pulse rate in trauma patients and their correlation with mortality: Cushing's phenomenon revisited. International journal of critical illness and injury science. 2017 Jan-Mar:7(1):14-17. doi: 10.4103/2229-5151.201950. Epub [PubMed PMID: 28382254]
Kalmar AF, Van Aken J, Caemaert J, Mortier EP, Struys MM. Value of Cushing reflex as warning sign for brain ischaemia during neuroendoscopy. British journal of anaesthesia. 2005 Jun:94(6):791-9 [PubMed PMID: 15805143]
Aronovich D, Scumpia A, Edwards D. Cushing's reflex in a rare case of adult medulloblastoma. World journal of emergency medicine. 2014:5(2):148-50 [PubMed PMID: 25215166]
Level 3 (low-level) evidence