Anatomy, Abdomen and Pelvis: Deep Perineal Space
Anatomy, Abdomen and Pelvis: Deep Perineal Space
Introduction
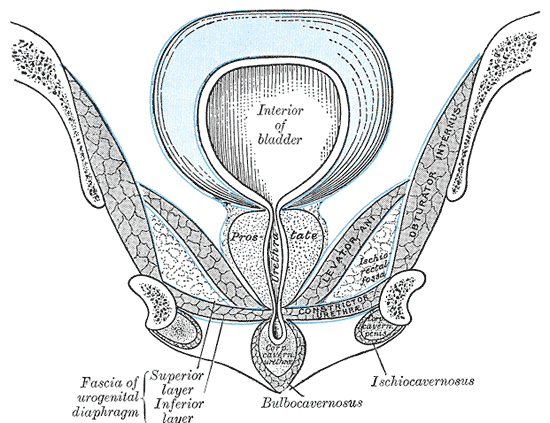
The perineum divides into an anterior urogenital triangle and a posterior anal triangle. The urogenital triangle of the perineum is divided into two pouches or spaces by a robust fibrous sheet known as the perineal membrane. This membrane is stretched across the urogenital triangle, attached laterally to the ischiopubic rami. The deep perineal pouch is superior to the perineal membrane, and the superficial perineal pouch is inferior.
The deep perineal pouch is in the urogenital triangle of the perineum below the pelvic diaphragm. It presents as a triangular, trilaminar space with sphincter urethrae [external urethral sphincter], deep transverse perineal, and compressor urethrae [in females]. The fibromuscular structures of the pouch often go by the name of the urogenital diaphragm.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
Anatomic Boundaries:
Superior: by the superior fascia of the urogenital diaphragm, a continuation of the inferior fascia of the pelvic diaphragm
Inferior: by the inferior fascia of urogenital diaphragm widely known as the perineal membrane
Lateral: by the lower part of the obturator fascia and the bony outlet of the pelvis [conjoint ischiopubic ramus]
Contents of the deep perineal pouch in both sexes:
A part of the urethra, sphincter urethrae, branches of internal pudendal artery branches and pudendal nerve branch that supplies the external genitalia
Contents of the deep perineal pouch in males:
- The muscular components sphincter urethrae and deep transverse perinei with perineal membrane together are known as the urogenital diaphragm. a detailed description of these structures is given in the muscles section below
- Membranous urethra: the part of the urethra passing through the deep perineal pouch is called membranous urethra and this is the narrowest and least distensible part of the urethra in males. It is approximately 1.5 cm in length and traverses through the perineal membrane 2 to 3 cm behind the pubic symphysis
- Bulbourethral glands of Cowper are present on either side of the membranous urethra and their ducts pierce the perineal membrane posterolateral to the urethra and finally open into the urethra to empty their secretions into the membranous urethra during sexual arousal prior to ejaculation. Thick clear mucous secretions of the gland neutralize the acidic urine in the urethra and act as a lubricant for the semen passage.[1]
Contents of the deep perineal pouch in females:
- Urethra: in females, the urethra is approximately 4 cm in length, it passes through the perineal membrane and opens as the external urethral orifice in the vestibule above the vaginal opening
- Vagina: is situated behind the urethra. The perineal membrane in females is divided by urethra and vagina into two halves. At the hymenal ring level, the lateral walls of the vagina attach to the perineal membrane
- The muscle external urethral sphincter is detailed below in the muscles section, and the arteries and nerves are detailed in the corresponding sections
Embryology
Development of the anatomic structures in the deep perineal pouch: Membranous urethra develops from the definitive urogenital sinus, the sphincteric musculature around the membranous urethra develops from the surrounding mesenchymal condensation. Bulbourethral glands develop as the sprouting of the definitive urogenital sinus that forms as the membranous urethra.[2]
Blood Supply and Lymphatics
Distal to the perineal branch the internal pudendal artery gives artery which supplies the urethral sphincter.
In males, the internal pudendal gives off the penile arteries, the artery to the bulb, arteries to the crura, cavernosal arteries or deep arteries of the penis and the dorsal artery of the penis. The bulbourethral gland receives supply by branches from the artery to the bulb of the penis and common penile artery.
In females, its branches include the artery to the bulb of the vestibule, the dorsal artery of the clitoris and deep artery of the clitoris.
Lymphatics drain into external and internal iliac nodes.
Nerves
Pudendal nerve branches are present in the pouch: In females, the dorsal nerves of the clitoris and in males, dorsal nerves of the penis. A perineal branch of the pudendal nerve supplies external urethral sphincter.
Muscles
Urogenital diaphragm: is the name given to deep transverse perineal and sphincter urethrae with inferior fascia is known as the urogenital diaphragm. The superior fascia of the urogenital diaphragm is a continuation of the inferior fascia of the levator ani (pelvic diaphragm), and inferior fascia is the perineal membrane.[3] Many studies have disputed the use of term urogenital diaphragm and started using the term perineal membrane for the 3-dimensional musculofascial expansion across the urogenital triangle. It attaches laterally to the pubic arch and posteriorly attaches to the perineal body.[4][5]
In males:
Deep transverse perineal muscle: situated in the posterior part. It emerges from the inner aspect of the ischial tuberosities of the pelvic girdle and extends towards the midline to attach to the perineal body. The superior and inferior fasciae of the urogenital diaphragm are continuous behind the transverse perineal muscle.
External urethral sphincter: in males sphincter urethrae at the level of the membranous urethra is made of striated muscle and encircles the urethra. This circular sphincter composed of the smooth and striated muscle surrounding urethra forms a strong sphincter. The circular smooth muscle part of this sphincter is situated between the longitudinal smooth muscle coat of the ureter and striated muscle of the rhabdosphincter[2]. The somatic innervation is by the perineal branch of the pudendal nerve, and autonomic innervation is from the sacral plexus and pelvic splanchnic nerves.
In females
External urethral sphincter: in females, external sphincter of the urethra is more complex than in males. It is more proper to call this as the urogenital sphincter. It includes a circular sphincter around the urethra (the urethral sphincter). Another sphincter, the compressor urethrae, has fibers anterior to the urethra and passes laterally to attach to the connective tissue near the inner surface of the ischiopubic ramus.[5][6]
Surgical Considerations
In urology clinics, the urethra is divided into the anterior and posterior urethra by the perineal membrane. The part of urethra above the perineal membrane is called the posterior urethra, and the portion below the perineal membrane (the penile urethra) is called the anterior urethra.[7] Sphincteroplasty of sphincter urethrae is a procedure performed for some urinary incontinence patients.
Clinical Significance
The fibromuscular structures of the deep perineal pouch provide sphincteric and supportive roles for the urogenital organs of the pelvis. The membranous urethra is easily injured if enough external force is applied, even though it has both longitudinal and circumferential support and protection from the pelvic ring. In pelvic trauma, the membranous urethra is at the risk of injury because of its proximity with pubic bones, disruption of urinary continence may occur in these cases. The male urethra is more susceptible to damage than females in pelvic trauma.[8] Failure of the urethral sphincter also results in urinary incontinence, which could result in females secondary to neuromuscular damage to the sphincter or its supporting membrane during childbirth.[7] Bulbourethral glands of Cowper can be affected by congenital or acquired pathologies. Cowper's syringocele is cystic dilatation of the duct of the gland. Infections, calcification, and neoplasms can affect the gland.[1]
Other Issues
Views in recent literature:
The term urogenital diaphragm is the term in current use for the urethral sphincter complex that is packed by a superior fascia and an inferior fascia in many of the descriptions, but this description has come under scrutiny by some authors. Some studies questioned the existence of the superior fascia as the striated sphincter urethrae are not confined to only to the deep perineal space, it even extends upwards along the urethra. The tough fibrous inferior fascia existence is undisputedly acknowledged. The term "perineal membrane" introduced by Oelrich (1983) is in current use as a replacement for the urogenital diaphragm. The fibromuscular layer complex below the pelvic diaphragm is now called by many as perineal membrane.[5]
The perineal membrane divides into two parts, a ventral portion, and a dorsal portion. The dorsal portion has a transverse fibrous sheet attached to the perineal body and lateral wall of the vagina. The ventral portion has many structures that are the sphincter complex of the ureter. It is a 3-dimensional complex structure rather than the previous description of the urogenital diaphragm sandwiched between two fasciae.[9]
Media
(Click Image to Enlarge)
References
Chughtai B, Sawas A, O'Malley RL, Naik RR, Ali Khan S, Pentyala S. A neglected gland: a review of Cowper's gland. International journal of andrology. 2005 Apr:28(2):74-7 [PubMed PMID: 15811067]
Level 3 (low-level) evidenceOelrich TM. The urethral sphincter muscle in the male. The American journal of anatomy. 1980 Jun:158(2):229-46 [PubMed PMID: 7416058]
Klutke CG, Siegel CL. Functional female pelvic anatomy. The Urologic clinics of North America. 1995 Aug:22(3):487-98 [PubMed PMID: 7645151]
Mirilas P, Skandalakis JE. Urogenital diaphragm: an erroneous concept casting its shadow over the sphincter urethrae and deep perineal space. Journal of the American College of Surgeons. 2004 Feb:198(2):279-90 [PubMed PMID: 14759786]
Oelrich TM. The striated urogenital sphincter muscle in the female. The Anatomical record. 1983 Feb:205(2):223-32 [PubMed PMID: 6846873]
Jung J, Ahn HK, Huh Y. Clinical and functional anatomy of the urethral sphincter. International neurourology journal. 2012 Sep:16(3):102-6. doi: 10.5213/inj.2012.16.3.102. Epub 2012 Sep 30 [PubMed PMID: 23094214]
Rahn DD,Roshanravan SM, Pathophysiology of urinary incontinence, voiding dysfunction, and overactive bladder. Obstetrics and gynecology clinics of North America. 2009 Sep; [PubMed PMID: 19932410]
Ingram MD, Watson SG, Skippage PL, Patel U. Urethral injuries after pelvic trauma: evaluation with urethrography. Radiographics : a review publication of the Radiological Society of North America, Inc. 2008 Oct:28(6):1631-43. doi: 10.1148/rg.286085501. Epub [PubMed PMID: 18936026]
Stein TA, DeLancey JO. Structure of the perineal membrane in females: gross and microscopic anatomy. Obstetrics and gynecology. 2008 Mar:111(3):686-93. doi: 10.1097/AOG.0b013e318163a9a5. Epub [PubMed PMID: 18310372]