Introduction
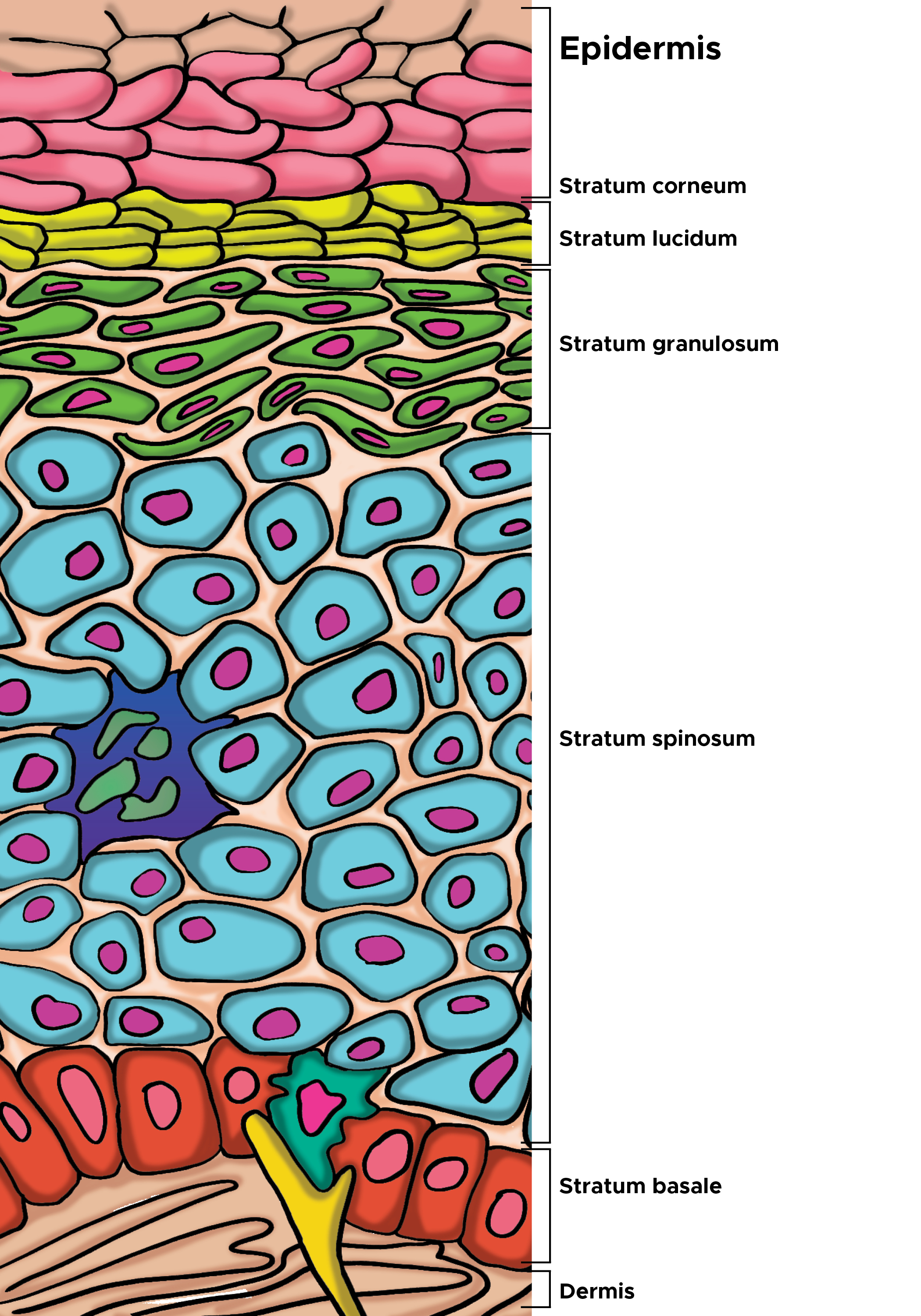
The dermis is a connective tissue layer sandwiched between the epidermis and subcutaneous tissue. The dermis is a fibrous structure composed of collagen, elastic tissue, and other extracellular components that include vasculature, nerve endings, hair follicles, and glands. The role of the dermis is to support and protect the skin and deeper layers, assist in thermoregulation, and aid in sensation. Fibroblasts are the primary cells within the dermis, but histiocytes, mast cells, and adipocytes also play important roles in maintaining the normal structure and function of the dermis (see Image. Illustration of Cells of the Epidermis).
Structure
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure
The dermis is a connective tissue layer of mesenchymal origin located deep in the epidermis and superficial to the subcutaneous fat layer.[1] The composition of the dermis is mainly fibrous, consisting of collagen and elastic fibers. Between the fibrous components lies an amorphous extracellular "ground substance" containing glycosaminoglycans, such as hyaluronic acid, proteoglycans, and glycoproteins. The dermis is divided into 2 layers: the papillary dermis and the reticular dermis. The papillary dermis is the superficial layer, lying deep into the epidermis. The papillary dermis is composed of loose connective tissue that is highly vascular. The reticular layer is the deep layer, forming a thick layer of dense connective tissue that constitutes the bulk of the dermis.
Collagen is the principal component of the dermis. Specifically, type I and type III collagen are found in abundance. Elastic fibers also play an important structural role within the dermis. Elastic fibers are composed of elastin and fibrillin microfibrils. In contrast to collagen, the biochemical configuration of elastin allows for gliding, stretching, and recoiling of fibers.[2] The reticular dermis comprises thick elastic fibers. Two subtypes of elastic fibers are worth further discussion: elaunin and oxytalan fibers.[3] Elaunin fibers are horizontally arranged elastic fibers found near the junction of the papillary and reticular dermis. Oxytalan fibers are perpendicular elastic fibers found in the papillary dermis.[4] The dermis houses blood vessels, nerve endings, hair follicles, and glands. There are many cell types found within the connective tissue of the dermis, including fibroblasts, macrophages, adipocytes, mast cells, Schwann cells, and stem cells.[5] Fibroblasts are the principal cells of the dermis. Mast cells are typically found surrounding dermal capillaries.
Function
Skin Support and Protection
The structure of the dermis provides a connective tissue framework for strength, flexibility, and protection of the deeper anatomical structures. Collagen and extracellular components like hyaluronic acid fortify the skin and facilitate an anchor for the epidermis via hemidesmosomes and other adhesive basement membrane zone (BMZ) components.[6] Oxytalan fibers may also play a role in anchoring the epidermis. Elastic tissue also helps support the skin and provides flexibility. The blood vessels in the dermis are crucial for the maintenance of the epidermis and epidermal appendages. Nutrients via blood support the epidermis, hair follicles, and sweat glands. The vascular network further permits the dermis to host an inflammatory response via the recruitment of neutrophils, lymphocytes, and other inflammatory cells. The dermal blood supply also plays a role in temperature regulation discussed below.
Thermoregulation
Vasoactive dermal vessels regulate body temperature. Specialized structures called glomus bodies also take part in thermoregulation through AV shunt formation.[7] Glomus bodies are complexes of glomus cells, vessels, and smooth muscle cells that predominate in the digits, palms, and soles.[8] Although often within the dermis, eccrine sweat glands are ectoderm-derived epidermal appendages that invaginate into the deeper tissue of the dermis and subcutaneous layer.[9]
Sensation
Several mechanoreceptors are present in the dermis. Nerve endings in the dermis surround hair follicles. These nerve endings sense hair movement and act as mechanoreceptors, allowing sensation to extend beyond the skin's surface. Deep pressure receptors also exist. Pacinian corpuscles are large, lamellar, ovoid structures found in the deep dermis and they provide deep pressure and vibratory sensation. Meissner's corpuscles, located in the dermal papillae of the papillary dermis, respond to low-frequency stimuli. Meissner's corpuscles are concentrated in glabrous (hairless) skin.[10]
Cells of the Dermis and Their Function
The dermis contains many cell types. Fibroblasts, the principal cell of the dermis, handle the synthesis of collagen, elastic and reticular fibers, and extracellular matrix material. Histiocytes are tissue macrophages present within the connective tissue that assist the immune system. Mast cells are inflammatory cells located in the perivascular areas of the dermis. Mast cells secrete vasoactive and proinflammatory mediators important in inflammatory reactions, collagen remodeling, and wound healing.[11] Dermal adipocytes are a distinct cell population from the subcutaneous adipose tissue. Dermal adipocytes not only provide insulation and energy storage but also assist in hair follicle regeneration and wound healing.[12][13]
Tissue Preparation
The dermis is examined using a standard skin biopsy. The tissue sample should first be fixated with formalin to preserve tissue structure. After fixation, the specimen is dehydrated with an alcohol (eg, ethanol) to remove water. The alcohol agent is then cleared using xylol. After, the tissue sample is embedded in paraffin. After hardening of the paraffin medium, a microtome slices the specimen. The tissue specimen may be stained according to hematoxylin and eosin (H&E) staining protocols.
Histochemistry and Cytochemistry
Immunofluorescence of tissue samples is an important diagnostic tool in autoimmune blistering diseases such as bullous pemphigoid and dermatitis herpetiformis. For example, linear deposition of immunoglobulin (Ig) G and complement (C3) along the dermoepidermal junction is characteristic of bullous pemphigoid. Granular deposits of IgA in the dermal papillae are characteristic of dermatitis herpetiformis.[14]
Microscopy, Light
Light microscopic analysis of H&E-stained samples delineates the epidermis, dermis, and subcutaneous adipose. The epidermis is easily visualized due to the presence of basophilic keratinocytes. Scanning across the tissue sample, one can appreciate the alternating dermal papillae and rete ridges. Dermal papillae are the protrusions of dermal connective tissue into the epidermal layer. Rete ridges are the extensions of the epidermis into the dermal layer. This undulating pattern is more apparent in the thick skin of the hands and palms. There is no clear line of distinction between the papillary and reticular dermis. Collagen patterns are mostly horizontal throughout. The superficial papillary dermis possesses thinner elastic fibers compared to the thicker elastic fibers of the reticular dermis. The papillary dermis is composed of loose connective tissue (LCT) and is highly vascular. The reticular dermis shows thick collagen bundles and forms the bulk of the dermal layer.
Hair follicles, glands, and ducts can be seen throughout the epidermis, dermis, and hypodermis. A higher magnification view can further distinguish sebaceous, apocrine, and eccrine sweat glands. Meissner's corpuscles and Pacinian corpuscles can also be distinguished by light microscopy. Pacinian corpuscles in the deep dermis or hypodermis have an onion-like appearance on cross-sectional views. Meissner corpuscles are seen in the dermal papillae as oblong structures with neurons in a spiral orientation surrounded by a fibrous capsule.[10] Polarizing light microscopy is useful in the diagnosis of depositional diseases such as amyloidosis and gout. Tissue samples stained with Congo red dye may be examined under polarized light, producing a characteristic apple-green birefringence of protein deposits in amyloidosis.[15] Similarly, polarized light microscopy is used to differentiate urate crystal and calcium deposition.[16]
Microscopy, Electron
Electron microscopy (EM) can be used to visualize the ultrastructural features of the skin. Most importantly, EM has been used to visualize the basement membrane zone of the dermoepidermal junction. EM shows ultrastructural components of hemidesmosomes, the lamina lucida (LL), the lamina densa (LD), and various anchoring fibrils.[17]
Pathophysiology
There are numerous diseases that affect the skin. The following discussion describes some common and uncommon diseases that affect the dermis. This discussion is not all-inclusive but demonstrates the importance of understanding the normal structure and function of the genetic diseases that can affect dermal structure and function. Ehlers-Danlos syndrome is a group of genetic connective tissue disorders caused by various mutations in collagen. The mutations in dermal collagen result in skin hypermobility and fragility. Osteogenesis imperfecta is a genetic disorder of type I collagen, causing decreased dermal collagen and impaired skin elasticity.[18] Marfan syndrome is another genetic condition caused by a defect in the FBN1 gene encoding the fibrillin-1 protein. While skin complaints are not required for diagnosis, patients are prone to the development of striae distensae (stretch marks) due to rapid growth phases in adolescence.[19] These 3 genetic disorders, along with other inherited diseases, may rarely cause reactive elastosis perforans serpingosa, in which transepithelial elimination of elastic fibers manifests clinically as papules in an annular or serpiginous pattern.[20]
Cushing syndrome, chronic glucocorticoid use, and pregnancy are other conditions causing striae distensae. Glucocorticoids inhibit fibroblasts, thus disrupting the synthesis of collagen and ECM material. Histology of striae distensae reveals flattening of the epidermis with loss of rete ridges and changes in the architecture of collagen bundles coupled with elastin degeneration throughout the dermis.[21] The overactivity of fibroblasts has been implicated in many skin-related diseases. Myofibroblasts, expressing alpha-smooth muscle actin (a-SMA), have been implicated in both hypertrophic scars and keloids.[22][23] A careful histopathological examination is required to differentiate among keloids, hypertrophic scars, dermatofibromas, dermatofibrosarcoma protuberans, and scleroderma due to similar histopathologic findings.[24] Lichen sclerosis is an inflammatory disorder involving abnormal fibroblast function in the papillary dermis, causing fibrosis of the superficial dermis and epidermis.[25] Acanthosis nigricans results from increased growth factor receptor signaling causing proliferation of epidermal keratinocytes and dermal fibroblasts, leading to hyperkeratosis and papillomatosis ("peaks and valleys") on histopathology.[26][27] Researchers have also observed persistent activation of fibroblasts in the dermis in morphea and nephrogenic systemic fibrosis.[28]
Aging and chronic sun exposure can weaken the dermis. Solar elastosis is due to chronic ultraviolet (UV) radiation exposure, resulting in damage to elastic fibers. Histology reveals basophilic degeneration of elastic fibers in the dermis.[29] The reduction of connective tissue in aging, usually with concomitant UV damage, causes actinic purpura (i.e., senile purpura), where the dermis cannot support its vasculature. As a result, minor trauma can lead to extravasation of blood.[30] Similar manifestations may be seen in chronic glucocorticoid users. Glomus tumors can also occur within the dermis and deeper tissues, especially within the digits and palms where glomus bodies are concentrated.[31]
Urticaria is an inflammatory dermatosis characterized by vascular hyperpermeability, causing superficial dermal edema with resultant lymphatic dilation. The pathogenesis of urticaria often involves degranulation of mast cells and immunoglobulin E-dependent pathways; however, this is not true for all cases.[32] Mastocytosis describes a spectrum of rare diseases involving an increase in mast cells within the skin and other organs. Urticaria pigmentosa is the most common cutaneous form of mastocytosis and predominately occurs in childhood.[33] Granulomatous diseases such as sarcoidosis, granuloma annulare, necrobiosis lipoidica, and mycobacterial infections (tuberculosis, leprosy) involve histiocytes within the dermis. Mycobacterium leprae infects Schwann cells of peripheral nerves, leading to diminished or absent cutaneous sensation in leprosy.[34] Lymphocytic infiltration of the dermis causes diseases such as polymorphous light eruption, a common photosensitive dermatosis.[35] Cutaneous manifestations of hematologic malignancy, such as leukemia cutis, also involve leukocytic infiltration into the skin layers. Sweet syndrome is a rare condition associated with neutrophilia and neutrophilic infiltration into the reticular dermis.[36] Other disorders involve the deposition of foreign material within the dermis, such as cholesterol in xanthelasma and protein fibrils in amyloidosis.[37] Burns and ulcers are important to consider as the depth of burn or wound involvement affects patient diagnosis and management. Partial-thickness burns, also known as second-degree burns, destroy the epidermis and extend into the dermis.[38] Similarly, stage II pressure ulcers, as described by the NPUAP, expose the dermis.[39]
Clinical Significance
The clinical significance of the microanatomy and function of the dermis is a broad and complex topic. Below is a brief list of diseases that involve the dermis. Please note many of these diseases can affect other cutaneous layers and organs of the body. Understanding the normal anatomy and physiology of the dermis is paramount in mastering the cutaneous manifestations of the diseases listed below.
Structural Disorders
- Structural disorders of the dermis include inherited and acquired diseases of collagen, elastic tissue, and fibroblasts.
- Solar elastosis
- Actinic, or senile, purpura
- Striae
- Scars, hypertrophic scars, and keloids
- Burns or wounds (eg, puncture or laceration)
- Dermatofibroma and dermatofibrosarcoma protuberans
- Morphea
- Nephrogenic systemic fibrosis
- Genetic diseases (eg, Ehlers-Danlos syndrome, osteogenesis imperfecta, and Marfan's syndrome)
Inflammatory and Autoimmune Disorders
- Autoimmune blistering diseases (eg, dermatitis herpetiformis)
- Drug eruption
- Granulomatous disease (eg, sarcoidosis, granuloma annulare, mycobacterial infections)
- Lichen sclerosis
- Leukemia cutis
- Mastocytosis (eg, urticaria pigmentosa)
- Polymorphous light eruption
- Sweet syndrome
- Urticaria and eczematous dermatitis
Depositional Disorders
- Cutaneous depositional diseases involve the deposition of endogenous or exogenous substances in the dermis or subcutaneous tissue.[40] The respective deposited substance is listed in parentheses.
- Amyloidosis (protein)
- Calcinosis cutis (calcium)
- Gout (uric acid)
- Myxedema (mucopolysaccharides)
- Xanthoma/xanthelasma (cholesterol)
Media
(Click Image to Enlarge)
References
Lopez-Ojeda W, Pandey A, Alhajj M, Oakley AM. Anatomy, Skin (Integument). StatPearls. 2024 Jan:(): [PubMed PMID: 28723009]
Green EM, Mansfield JC, Bell JS, Winlove CP. The structure and micromechanics of elastic tissue. Interface focus. 2014 Apr 6:4(2):20130058. doi: 10.1098/rsfs.2013.0058. Epub [PubMed PMID: 24748954]
Cotta-Pereira G, Guerra Rodrigo F, Bittencourt-Sampaio S. Oxytalan, elaunin, and elastic fibers in the human skin. The Journal of investigative dermatology. 1976 Mar:66(3):143-8 [PubMed PMID: 1249442]
Uitto J, Li Q, Urban Z. The complexity of elastic fibre biogenesis in the skin--a perspective to the clinical heterogeneity of cutis laxa. Experimental dermatology. 2013 Feb:22(2):88-92. doi: 10.1111/exd.12025. Epub 2012 Oct 23 [PubMed PMID: 23088642]
Level 3 (low-level) evidenceProst-Squarcioni C, Fraitag S, Heller M, Boehm N. [Functional histology of dermis]. Annales de dermatologie et de venereologie. 2008 Jan:135(1 Pt 2):1S5-20. doi: 10.1016/S0151-9638(08)70206-0. Epub [PubMed PMID: 18442658]
Hashmi S, Marinkovich MP. Molecular organization of the basement membrane zone. Clinics in dermatology. 2011 Jul-Aug:29(4):398-411. doi: 10.1016/j.clindermatol.2011.01.009. Epub [PubMed PMID: 21679867]
Level 3 (low-level) evidenceSethu C, Sethu AU. Glomus tumour. Annals of the Royal College of Surgeons of England. 2016 Jan:98(1):e1-2. doi: 10.1308/rcsann.2016.0005. Epub [PubMed PMID: 26688416]
Friske JE, Sharma V, Kolpin SA, Webber NP. Extradigital glomus tumor: a rare etiology for wrist soft tissue mass. Radiology case reports. 2016 Sep:11(3):195-200. doi: 10.1016/j.radcr.2016.04.001. Epub 2016 May 17 [PubMed PMID: 27594949]
Level 3 (low-level) evidenceCui CY, Schlessinger D. Eccrine sweat gland development and sweat secretion. Experimental dermatology. 2015 Sep:24(9):644-50. doi: 10.1111/exd.12773. Epub 2015 Jul 14 [PubMed PMID: 26014472]
Zimmerman A, Bai L, Ginty DD. The gentle touch receptors of mammalian skin. Science (New York, N.Y.). 2014 Nov 21:346(6212):950-4. doi: 10.1126/science.1254229. Epub [PubMed PMID: 25414303]
Level 3 (low-level) evidenceWilgus TA, Wulff BC. The Importance of Mast Cells in Dermal Scarring. Advances in wound care. 2014 Apr 1:3(4):356-365 [PubMed PMID: 24757590]
Level 3 (low-level) evidenceKruglikov IL, Scherer PE. Dermal Adipocytes: From Irrelevance to Metabolic Targets? Trends in endocrinology and metabolism: TEM. 2016 Jan:27(1):1-10. doi: 10.1016/j.tem.2015.11.002. Epub 2015 Nov 29 [PubMed PMID: 26643658]
Driskell RR, Jahoda CA, Chuong CM, Watt FM, Horsley V. Defining dermal adipose tissue. Experimental dermatology. 2014 Sep:23(9):629-31. doi: 10.1111/exd.12450. Epub [PubMed PMID: 24841073]
Level 3 (low-level) evidenceJindal A, Rao R, Bhogal BS. Advanced Diagnostic Techniques in Autoimmune Bullous Diseases. Indian journal of dermatology. 2017 May-Jun:62(3):268-278. doi: 10.4103/ijd.IJD_196_17. Epub [PubMed PMID: 28584369]
Lee DY, Kim YJ, Lee JY, Kim MK, Yoon TY. Primary localized cutaneous nodular amyloidosis following local trauma. Annals of dermatology. 2011 Nov:23(4):515-8. doi: 10.5021/ad.2011.23.4.515. Epub 2011 Nov 3 [PubMed PMID: 22148024]
Level 3 (low-level) evidenceGaviria JL, Ortega VG, Gaona J, Motta A, Medina Barragán OJ. Unusual Dermatological Manifestations of Gout: Review of Literature and a Case Report. Plastic and reconstructive surgery. Global open. 2015 Jul:3(7):e445. doi: 10.1097/GOX.0000000000000420. Epub 2015 Aug 10 [PubMed PMID: 26301134]
Level 3 (low-level) evidenceYurchenco PD, Patton BL. Developmental and pathogenic mechanisms of basement membrane assembly. Current pharmaceutical design. 2009:15(12):1277-94 [PubMed PMID: 19355968]
Level 3 (low-level) evidenceHansen B, Jemec GB. The mechanical properties of skin in osteogenesis imperfecta. Archives of dermatology. 2002 Jul:138(7):909-11 [PubMed PMID: 12071818]
Pepe G, Giusti B, Sticchi E, Abbate R, Gensini GF, Nistri S. Marfan syndrome: current perspectives. The application of clinical genetics. 2016:9():55-65. doi: 10.2147/TACG.S96233. Epub 2016 May 9 [PubMed PMID: 27274304]
Level 3 (low-level) evidenceLee SH, Choi Y, Kim SC. Elastosis perforans serpiginosa. Annals of dermatology. 2014 Feb:26(1):103-6. doi: 10.5021/ad.2014.26.1.103. Epub 2014 Feb 17 [PubMed PMID: 24648695]
Level 3 (low-level) evidenceUd-Din S, McGeorge D, Bayat A. Topical management of striae distensae (stretch marks): prevention and therapy of striae rubrae and albae. Journal of the European Academy of Dermatology and Venereology : JEADV. 2016 Feb:30(2):211-22. doi: 10.1111/jdv.13223. Epub 2015 Oct 20 [PubMed PMID: 26486318]
Baum J, Duffy HS. Fibroblasts and myofibroblasts: what are we talking about? Journal of cardiovascular pharmacology. 2011 Apr:57(4):376-9. doi: 10.1097/FJC.0b013e3182116e39. Epub [PubMed PMID: 21297493]
Lee JY, Yang CC, Chao SC, Wong TW. Histopathological differential diagnosis of keloid and hypertrophic scar. The American Journal of dermatopathology. 2004 Oct:26(5):379-84 [PubMed PMID: 15365369]
Jumper N, Paus R, Bayat A. Functional histopathology of keloid disease. Histology and histopathology. 2015 Sep:30(9):1033-57. doi: 10.14670/HH-11-624. Epub 2015 Apr 22 [PubMed PMID: 25900252]
Nair PA. Vulvar Lichen Sclerosus et Atrophicus. Journal of mid-life health. 2017 Apr-Jun:8(2):55-62. doi: 10.4103/jmh.JMH_13_17. Epub [PubMed PMID: 28706405]
Puri N. A study of pathogenesis of acanthosis nigricans and its clinical implications. Indian journal of dermatology. 2011 Nov:56(6):678-83. doi: 10.4103/0019-5154.91828. Epub [PubMed PMID: 22345770]
Brady MF, Rawla P. Acanthosis Nigricans. StatPearls. 2024 Jan:(): [PubMed PMID: 28613711]
Piera-Velazquez S, Louneva N, Fertala J, Wermuth PJ, Del Galdo F, Jimenez SA. Persistent activation of dermal fibroblasts from patients with gadolinium-associated nephrogenic systemic fibrosis. Annals of the rheumatic diseases. 2010 Nov:69(11):2017-23. doi: 10.1136/ard.2009.127761. Epub 2010 Jun 22 [PubMed PMID: 20570839]
Heng JK, Aw DC, Tan KB. Solar elastosis in its papular form: uncommon, mistakable. Case reports in dermatology. 2014 Jan:6(1):124-8. doi: 10.1159/000362589. Epub 2014 Apr 24 [PubMed PMID: 24926253]
Level 3 (low-level) evidenceCeilley RI. Treatment of Actinic Purpura. The Journal of clinical and aesthetic dermatology. 2017 Jun:10(6):44-50 [PubMed PMID: 28979656]
Mravic M, LaChaud G, Nguyen A, Scott MA, Dry SM, James AW. Clinical and histopathological diagnosis of glomus tumor: an institutional experience of 138 cases. International journal of surgical pathology. 2015 May:23(3):181-8. doi: 10.1177/1066896914567330. Epub 2015 Jan 22 [PubMed PMID: 25614464]
Level 3 (low-level) evidenceDeacock SJ. An approach to the patient with urticaria. Clinical and experimental immunology. 2008 Aug:153(2):151-61. doi: 10.1111/j.1365-2249.2008.03693.x. Epub [PubMed PMID: 18713139]
Macri A, Cook C. Urticaria Pigmentosa. StatPearls. 2024 Jan:(): [PubMed PMID: 29494109]
Bhat RM, Prakash C. Leprosy: an overview of pathophysiology. Interdisciplinary perspectives on infectious diseases. 2012:2012():181089. doi: 10.1155/2012/181089. Epub 2012 Sep 4 [PubMed PMID: 22988457]
Level 3 (low-level) evidenceOakley AM, Ramsey ML. Polymorphic Light Eruption. StatPearls. 2024 Jan:(): [PubMed PMID: 28613636]
Soto R, Levy Y, Krause JR. Sweet syndrome and its association with hematopoietic neoplasms. Proceedings (Baylor University. Medical Center). 2015 Jan:28(1):62-4 [PubMed PMID: 25552802]
Level 3 (low-level) evidenceNair PA, Singhal R. Xanthelasma palpebrarum - a brief review. Clinical, cosmetic and investigational dermatology. 2018:11():1-5. doi: 10.2147/CCID.S130116. Epub 2017 Dec 18 [PubMed PMID: 29296091]
Schaefer TJ, Szymanski KD. Burn Evaluation and Management. StatPearls. 2024 Jan:(): [PubMed PMID: 28613492]
Bhattacharya S, Mishra RK. Pressure ulcers: Current understanding and newer modalities of treatment. Indian journal of plastic surgery : official publication of the Association of Plastic Surgeons of India. 2015 Jan-Apr:48(1):4-16. doi: 10.4103/0970-0358.155260. Epub [PubMed PMID: 25991879]
Level 3 (low-level) evidenceTouart DM, Sau P. Cutaneous deposition diseases. Part I. Journal of the American Academy of Dermatology. 1998 Aug:39(2 Pt 1):149-71; quiz 172-4 [PubMed PMID: 9704823]