Introduction
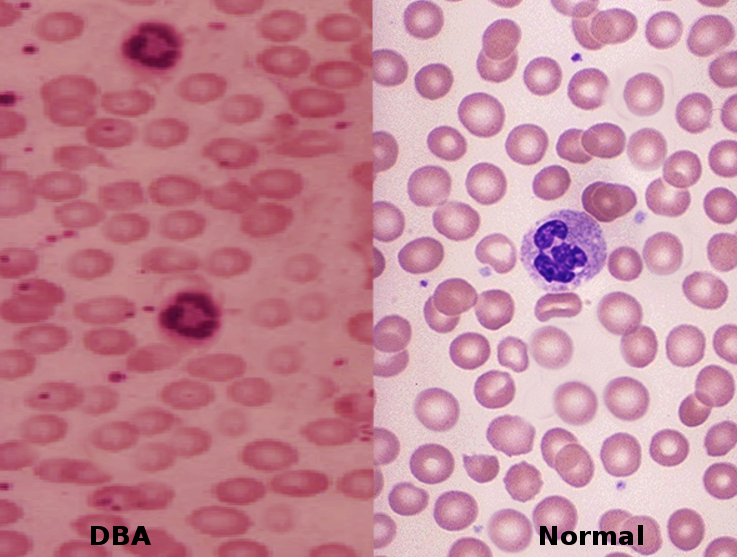
Anemia is a lower hemoglobin level than the normal range for each age group. Generally, anemia is classified into 3 categories based on red blood cells' mean corpuscular volume (MCV). Iron deficiency anemia is the most common type worldwide in all age groups.[1] However, here we talk about a rare type of anemia with genetic etiology. Diamond Blackfan anemia (DBA) is a congenital type characterized by pure red cell aplasia and associated with congenital bone abnormalities. It is a chronic macrocytic-normocytic anemia. DBA is a heterogeneous genetic disease inherited as an autosomal dominant inheritance in 40 to 45% of cases. The remainder, 55 to 60% of cases, typically present sporadically.[2][3][4] See Image. Diamond Blackfan Anemia. There are also cases noted with autosomal recessive inheritance with less frequency. Hydrops may occur but very rarely.[2]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Often, DBA occurs as a result of a genetic mutation. The most common mutation involves a ribosomal protein on chromosome 11. However, research has also noted mutations of transcription factor GATA1 in newer studies.[2][3][5][4] Ribosomal gene mutations are more common and present in about 60 to 70% of DBA cases.[2][3][5][4] It involves the gene that codes for both small and large ribosomal protein units, including but not limited to RPL5, RPL11, RPS 7, RPS 17, RPS 24, RPS 10, RPS 19, and RPS 26. In some families, mutations in RPL3, RPL7, RPL14, RPL19, RPL26, RPL36, RPL23A, RPL35, RPS 15, RPS 8, RPS27A, RPL35, and RPL18 gene has occurred.[2][3][6][4] despite a significant genetic component to DBA, 30 to 35% of cases remain genetically indeterminate.[2][7][4] Defective ribosomal protein biosynthesis initiates apoptosis of erythroid progenitor cells through p53 activation and stabilization, leading to erythroid failure. This mechanism is known as ‘ribosomal stress.'[2] Up to 50% of DBA cases have a heterozygous mutation of the ribosomal gene with loss of function.[2]
Epidemiology
DBA is a rare disease with an incidence rate of 1 in 500,000 live births. Onset generally is within the first year of life. The incidence of DBA is similar among different ethnicities and genders.[2][7]
Pathophysiology
DBA is a chronic macrocytic-normochromic anemia with low reticulocytes, normal platelets, and normal WBCs in the bone marrow. Laboratory workup is significant for elevated MCV and erythrocyte adenosine deaminase (eADA). Persistently elevated hemoglobin F is commonly seen in patients with DBA as well.[2][5][4]
Of all the ribosomal protein genes, RPS19, which codes a small ribosomal protein unit, is the most commonly involved mutated gene occurring in approximately 25% of cases of DBA.[2][4] Various mutations are present in more than 50% of RPS mutations. Among the types of mutations in the RPS gene are deletions, insertions, nonsense, splice sites, and frameshift changes. These mutations result in a deficiency of RPS19 protein, known as 'haploinsufficiency.'[2][4] Up to 50% of DBA cases have a heterozygous mutation of the ribosomal gene with loss of function in a single copy of the gene.[2] RPS19 plays an essential role in 18S rRNA maturation and 40S synthesis. RPS19 mutation causes decreased production of RPS19 and 40S ribosomal subunits by reducing translation initiation. With the decreased initiation of translation of the gene, there is a negative impact on normal primary hematopoietic progenitor cell differentiation and production due to increased apoptosis.[2][4] The overexpression of exogenous RPS19 can compensate for the deficiency of RPS19; this helps explain the haploinsufficiency phenomenon and suggests that DBA might be treatable by augmentation of the RPS gene.[2][4]
As per the ‘ribosomal stress’ mechanism, ribosomal deficiency activates and stabilizes p53, subsequently initiating apoptosis to cause bone marrow failure by terminating cell lines. Murine double minute (MDM2) is a ringer figure ubiquitin ligase that controls the level and activity of p53. When interacting with the normal ribosomal protein, MDM2 enhances p53 degradation.[2] In DBA, ribosomal stress causes many free RPS to build up due to disrupted ribosomal biosynthesis. These free RPS, such as RPL5, RPL11, RPL23, RPS27, and RPS7, bind with MDM2 to stabilize p53, leading to apoptosis, cell cycle arrest, and eventually erythroid hypoplasia.[2] DBA also results from non-Rp gene mutations such as GATA1. GATA1 encodes for transcription factors.[2][5][4] It plays an essential part in erythroid differentiation. GATA1 mutation of G to C transversion on the X chromosome leads to substituting leucine for valine. This mutation affects the splicing process of GATA1 and causes termination of GATA1, which plays a crucial role in the differentiation of erythroid cells. GATA1 mutation ultimately acts by a global translation blockade.[2][5][4]
History and Physical
In 90% of patients, DBA starts before 12 months of age. It commonly presents with congenital bony malformations (50% of the cases) and growth retardation (30% of cases).[3] The median age of presentation and diagnosis is 2 months of age.[2][3] Children usually first present with lethargy and pallor. Patients usually present with severe macrocytic anemia and normochromic anemia, along with erythroid aplasia due to congenital bone marrow failure. Typically, platelet and leukocyte counts are in the normal range; however, there have been patients with low leukocyte and high platelet counts. Patients can have significantly low reticulocyte counts.[2] DBA is also associated with elevated fetal hemoglobin levels, erythropoietin, and eADA activities.[2][7][5][4]
DBA presents a broad spectrum of phenotypes, from mild to severe. Physical abnormalities are present in 50% of cases.[2][3] The most common congenital physical abnormalities are thumb and upper extremity malformations, craniofacial anomalies, and short stature. The patient may also have a snub nose and wide-spaced eyes. The characteristic DBA anomalies include a distinct facial appearance and triphalangeal thumbs.[2][3][4] PRL5 mutation has associations with cleft lip or soft palate, while RPL11 largely correlates with thumb abnormalities but is also seen in cleft lip or palate cases.[2][3][4] Other physical anomalies include urogenital, atrial septal, and ventricular septal defects.[2][3][7]
Diagnostic Criteria for Classical DBA
- Age of onset less than 12 months
- Macrocytic anemia without other significant cytopenias
- Reticulocytopenia
- Bone marrow with normal cellularity with a lack of erythroid precursor [3][7][8]
Major Supporting Criteria
- Gene mutation described in DBA
- Positive family history
Minor Supporting Criteria
- Elevated ADA activity
- Congenital anomalies described in classical DBA
- Elevated HbF
- There is no evidence of another inherited bone marrow failure syndrome
Evaluation
After meeting the clinical criteria for diagnosis, lab tests help direct physicians toward making a correct diagnosis. Erythropoietin levels are elevated in DBA due to a lack of EPO receptors in the setting of erythroid aplasia. Other biological tests may include immune phenotyping and Igg/IgA agglutinin titer.[9] For molecular diagnosis, the first step is to characterize the phenotype with a bone marrow evaluation. Molecular tests are done to identify a heterozygous pathogenic variant in genes commonly involved in DBA.
Three types of molecular testing include serial single-gene testing and multigene panel. Parvovirus B19 is a common cause of bone marrow failure, making it mandatory to have parvovirus B19 serology or blood parvovirus B19 PCR done in patients where DBA is suspected.[9] Common hematological workup includes complete blood count with differential, hemoglobin F, ADA, erythropoietin level, reticulocyte count, and peripheral blood smear.
Treatment / Management
Corticosteroids are the first-line treatment of DBA. However, due to the long-term side effects of corticosteroids, patients with DBA often require chronic blood transfusions and concurrent iron chelation therapy.[2][3][5] A patient who is responsive to steroid therapy but with intolerable side effects requires chronic blood transfusions with a goal hemoglobin of 8 g/dl and requires a blood transfusion every 35 weeks.[2] Frequent monitoring of serum ferritin helps decide if iron chelation therapy is needed. Generally, iron chelation is started after 12 to 15 units of blood transfusions if serum ferritin concentration increases to 1000 to 1500 microgram/L or if hepatic iron concentration increases to 6 to 7 mg of the dry weight of liver tissue.[2][3][5] When iron chelation is required, deferasirox and desferrioxamine are the therapeutic choices. Deferiprone is not a recommendation due to its adverse effect on neutropenia.
The mechanism of action of corticosteroids remains obscure, but it seems to have a nonspecific anti-apoptotic effect on erythroid progenitors.[2] Metoclopramide can be used as a supplement to steroid therapy to decrease steroid dose and, therefore, the side effects.[4] Clinical trials also suggest leucine as a supplemental therapy to steroids.[4]
DBA may also receive treatment with hematopoietic stem cell transplantation (HSCT). This approach is the only treatment that cures the hematological manifestation of DBA; the procedure proves to be risky if a matched sibling donor is not available.[3][7][6][4] HSCT has a high success rate in patients under 10 years of age treated with an HLA-identical donor. It is indicated as an alternative to chronic blood transfusions if the patient becomes non-responsive to chronic blood transfusions or develops side effects of iron overload.[2][3] However, HSCT also has side effects to take into consideration, including infection and graft versus host disease.[2][6](B3)
According to recent literature, gene therapy and gene editing may be potential future treatments for DBA.[6][10] The difference between gene therapy and allogeneic HSCT is the source of stem cells. In gene therapy, the source of stem cells is in the patient’s normal HSCs; then, a normal copy of the mutated gene can be inserted into the patient's cells. In allogeneic HSCT, normal stem cells come from a donor.[10] Since the RPS19 gene presents in 25% of DBA cases, gene therapy may benefit patients with the mutation; this involves replacing the normal copy of gene RPS19 to rid the patient of DBA symptoms.[2][10][4] The viral vector system is the most common method for gene therapy, achieving a high success rate and safety profile.[6][10] About 20 to 25% of DBA patients undergo spontaneous remission.[5]
Differential Diagnosis
DBA has a unique quantitative defect in erythropoiesis rather than hematopoiesis, as seen in other bone marrow failure syndromes (BMF).[9] Various BMF syndromes include Fanconi anemia, Shwachman Bodian Diamond syndrome, cartilage-hair dysplasia, and dyskeratosis congenital.[9].
Genetic Conditions with BMF
- Transient erythroblastopenia of childhood (TEC) is a type of acquired anemia of unknown etiology, which usually (over 80%) presents at 1 year of age, while DBA usually (90%) presents before 1 year of age. Another distinguishing feature of TEC is only 10% of patients have elevated eADA, and anemia is normocytic.
- Fanconi anemia is bone marrow failure syndrome with pancytopenia and physical abnormalities usually present within the first decade of life.
- Shwachman-Diamond syndrome is a clinical syndrome characterized by exocrine pancreatic dysfunction with malabsorption, single or multi-lineage cytopenia, growth failure, bone abnormality, and susceptibility to myelodysplastic syndrome (MDS) and acute myeloid leukemia (AML).
- Pearson syndrome is a maternally inherited mDNA mutation characterized by sideroblastic anemia of childhood, exocrine pancreatic failure, liver failure, renal tubular defects, and pancytopenia. Death generally occurs in infancy due to progressive liver failure and severe metabolic acidosis.
- Dyskeratosis congenita is a genetically inherited disorder with a wide spectrum of severity. It is a telomere biology disorder with the classic triad of lacy reticular pigmentation of the upper chest and/or neck, dysplastic nails, and oral leukoplakia. These patients have an increased risk of MDS, BMF, or AML.
- Cartilage-hair dysplasia is an autosomal recessive inherited disorder with a high incidence in the Amish and Finnish populations. It is characterized by anemia, macrocytosis, defective T cell-mediated immune response, short tubular bone, and fine, sparse blond hair.
- Thrombocytopenia absent radii syndrome presents in the neonatal period or infancy with thrombocytopenia, absent radii, and the presence of bilateral thumbs. Other physical findings include rib, cervical, ulnar, and humeral deformities, cardiac septal defects, gastrointestinal abnormalities, and genitourinary abnormalities. In rare cases, aplastic anemia, multilineage cytopenia, or leukemia have been clinical features.
- Congenital amegakaryocytic thrombocytopenia usually presents at birth or in the neonatal period with severe thrombocytopenia, petechiae, and/or intracranial or intestinal mucosal bleeding. There is no congenital physical finding with this disease. In childhood, these patients may develop pancytopenia, MDS, or leukemia.[3][5]
Acquired conditions with BMF include viral infections (parvovirus B19, viral hepatitis and mononucleosis, and human T-cell lymphotropic virus type 1, HIV-associated pure red cell aplasia), immune-mediated diseases (myasthenia gravis, thymoma, multiple endocrinopathy, and systemic lupus erythematosus), and drugs (antiepileptic drugs, sulfonamide, isoniazid, chloramphenicol, procainamide, azathioprine, and thiamphenicol).[3][4]
Prognosis
The prognosis is relatively good, but complications related to treatment may alter the patient's quality of life.[2] Severe complications as a result of treatment or the development of cancer may reduce life expectancy.[2] Disease severity is determined by the quality of life and response to treatment.[2]
Complications
DBA patients are at high risk of developing a hematological complication in the first year of life. DBA has a high risk of developing AML, MDS, and solid tumors. Other complications like growth failure, organ failure, and infection are related to iron overload due to blood transfusion, chronic steroid use, and HSCT.
Deterrence and Patient Education
Patients with DBA should be monitored with complete blood counts frequently.[3] Periodic bone marrow biopsy or aspiration to evaluate cellularity and morphology helps diagnose any new cytopenia or bone marrow failure.[3] Patients who are steroid-dependent or transfusion-dependent should be monitored for blood pressure and growth as they are at high risk of organ failure; often, an endocrinology consult is necessary.[3] Healthy DBA patients must follow up every 4 to 6 months with history, physical examination, and complete blood count for cancer surveillance.[3] The rapid decline of any cell line indicates bone marrow failure and bone marrow biopsy with cytogenetic studies is required to diagnose chromosomal abnormalities associated with cancer.[3]
Relatives of DBA are at risk of developing DBA, given approximately 40 to 45% of autosomal dominant DBA patients have inherited a pathognomic variant from 1 of the parents. Additionally, X-linked inheritance has been noted.[3] It is appropriate to offer genetic testing if a pathognomic variant is known. The patient may receive an offer for other hematological tests for early diagnosis of DBA and cancer.[3] Approximately 55 to 60% of cases of DBA are found to have a de-novo pathognomic variant; this may be a result of alternate paternity or maternity, including assisted reproduction or adoption.[3]
Enhancing Healthcare Team Outcomes
Although DBA presents in only a small percentage of patients, significant complications can develop. An interprofessional team with an integrated approach to managing DBA is essential for a better outcome. An evidence-based approach is of paramount importance when dealing with patients suffering from DBA. The pharmacist should educate the patient on corticosteroids, the drugs of choice. These drugs have serious side effects that require monitoring. Pharmacists should also verify all dosing and perform medication reconciliation, reporting any concerns to the healthcare team. The hematology nurse must educate the patient about the potential adverse impact of chronic blood transfusions related to iron accumulation. Nurses also must be on the front lines administering these transfusions and must report on the effectiveness or lack thereof of these interventions. The obstetrician and labor & delivery nurses should counsel the patient on pregnancy. DBA patients during pregnancy can trigger a relapse of the condition when one is in remission. Hence, pregnancy should be avoided in a patient with DBA and should remain under high-risk obstetrics care in such circumstances.
To determine renal, liver, and cardiac abnormalities, renal, liver imaging and echocardiograms are recommendations for patients with DBA.[11][12][13] Also, with DBA being autosomal dominant, each child has a 50% probability of inheriting a pathological variant. Hence, prenatal testing is advised in pregnant women in whom a familial pathological variant is present.[3] Because of the constant need for treatment and admissions, the quality of life of many patients is poor, and hence, a mental health nurse should be involved in counseling. Finally, social workers should be involved to ensure the patient has the necessary support and finances to undergo treatment. Open communication between the interprofessional team is necessary for improved outcomes and limiting treatment morbidity. As evident from the above, DBA requires an interprofessional team approach, including physicians, specialists, specialty-trained nurses, psychological professionals, and pharmacists, collaborating across disciplines to achieve optimal patient results.
Media
References
Wang M. Iron Deficiency and Other Types of Anemia in Infants and Children. American family physician. 2016 Feb 15:93(4):270-8 [PubMed PMID: 26926814]
Engidaye G, Melku M, Enawgaw B. Diamond Blackfan Anemia: Genetics, Pathogenesis, Diagnosis and Treatment. EJIFCC. 2019 Mar:30(1):67-81 [PubMed PMID: 30881276]
Adam MP, Feldman J, Mirzaa GM, Pagon RA, Wallace SE, Amemiya A, Sieff C. Diamond-Blackfan Anemia. GeneReviews(®). 1993:(): [PubMed PMID: 20301769]
Da Costa L,O'Donohue MF,van Dooijeweert B,Albrecht K,Unal S,Ramenghi U,Leblanc T,Dianzani I,Tamary H,Bartels M,Gleizes PE,Wlodarski M,MacInnes AW, Molecular approaches to diagnose Diamond-Blackfan anemia: The EuroDBA experience. European journal of medical genetics. 2018 Nov; [PubMed PMID: 29081386]
Khincha PP, Savage SA. Neonatal manifestations of inherited bone marrow failure syndromes. Seminars in fetal & neonatal medicine. 2016 Feb:21(1):57-65. doi: 10.1016/j.siny.2015.12.003. Epub 2015 Dec 24 [PubMed PMID: 26724991]
Aspesi A, Borsotti C, Follenzi A. Emerging Therapeutic Approaches for Diamond Blackfan Anemia. Current gene therapy. 2018:18(6):327-335. doi: 10.2174/1566523218666181109124538. Epub [PubMed PMID: 30411682]
van Dooijeweert B, van Ommen CH, Smiers FJ, Tamminga RYJ, Te Loo MW, Donker AE, Peters M, Granzen B, Gille HJJP, Bierings MB, MacInnes AW, Bartels M. Pediatric Diamond-Blackfan anemia in the Netherlands: An overview of clinical characteristics and underlying molecular defects. European journal of haematology. 2018 Feb:100(2):163-170. doi: 10.1111/ejh.12995. Epub 2017 Dec 1 [PubMed PMID: 29114930]
Level 3 (low-level) evidenceKhurana M,Edwards D,Rescorla F,Miller C,He Y,Sierra Potchanant E,Nalepa G, Whole-exome sequencing enables correct diagnosis and surgical management of rare inherited childhood anemia. Cold Spring Harbor molecular case studies. 2018 Oct; [PubMed PMID: 30275003]
Level 3 (low-level) evidenceDa Costa L, Narla A, Mohandas N. An update on the pathogenesis and diagnosis of Diamond-Blackfan anemia. F1000Research. 2018:7():. pii: F1000 Faculty Rev-1350. doi: 10.12688/f1000research.15542.1. Epub 2018 Aug 29 [PubMed PMID: 30228860]
Li H, Lodish HF, Sieff CA. Critical Issues in Diamond-Blackfan Anemia and Prospects for Novel Treatment. Hematology/oncology clinics of North America. 2018 Aug:32(4):701-712. doi: 10.1016/j.hoc.2018.04.005. Epub 2018 Jun 5 [PubMed PMID: 30047421]
Van Hook JW, Gill P, Cyr D, Kapur RP. Diamond-Blackfan anemia as an unusual cause of nonimmune hydrops fetalis: a case report. The Journal of reproductive medicine. 1995 Dec:40(12):850-4 [PubMed PMID: 8926615]
Level 3 (low-level) evidenceCancado R,Watman NP,Lobo C,Chona Z,Manzur F,Traina F,Park M,Drelichman G,Zarate JP,Marfil L, Assessment of liver and cardiac iron overload using MRI in patients with chronic anemias in Latin American countries: results from ASIMILA study. Hematology (Amsterdam, Netherlands). 2018 Oct [PubMed PMID: 29663858]
Gomes RF, Munerato MC. The Stomatological Complications of Diamond-Blackfan Anemia: A Case Report. Clinical medicine & research. 2016 Jun:14(2):97-102. doi: 10.3121/cmr.2015.1305. Epub 2016 Feb 10 [PubMed PMID: 26864506]
Level 3 (low-level) evidence