Definition/Introduction
The oculocephalic reflex (doll's eyes reflex) is an application of the vestibular-ocular reflex (VOR) used for neurologic examination of cranial nerves 3, 6, and 8, the reflex arc including brainstem nuclei, and overall gross brainstem function. It is often used to examine patients in the neurologic critical care setting and may have utility to assess neonates, anesthetized patients, or dizzy patients.[1][2][3][4][5] The reflex derives its name from the characteristic doll's eyes appearance that a patient has if the reflex is positive.[6]
The oculocephalic reflex is performed by holding a patient’s eyelids open and moving their head from side to side. The examination should only be performed on patients with a stable cervical spine without c-spine precautions. With the patient's eyelids open, the examiner briskly rotates the patient's head from side to side while the examiner observes the patient’s eyes. The examiner observes a positive oculocephalic reflex when the patient moves their eyes opposite of the rotation of their head, such that their eyes stay looking forward (like a doll’s eyes). The examiner observes a negative oculocephalic reflex when the patient’s eyes stay midline and do not move while the examiner rotates the head. A similar examination is performable for vertical eye movements.[6] Note that the designation of "positive" (eyes moving in the opposite direction of head movement indicating an intact brainstem function) or "negative" (eyes moving towards the same direction of head movement indicating severe brainstem dysfunction) doll's eyes reflex is an oversimplification and that some eye movement with nystagmus can occur in pathologic states.[7] The reflex is suppressed in a conscious adult with normal neurologic function but is active in a comatose patient with gross brainstem function, absent if there is damage to the reflex arc.[6]
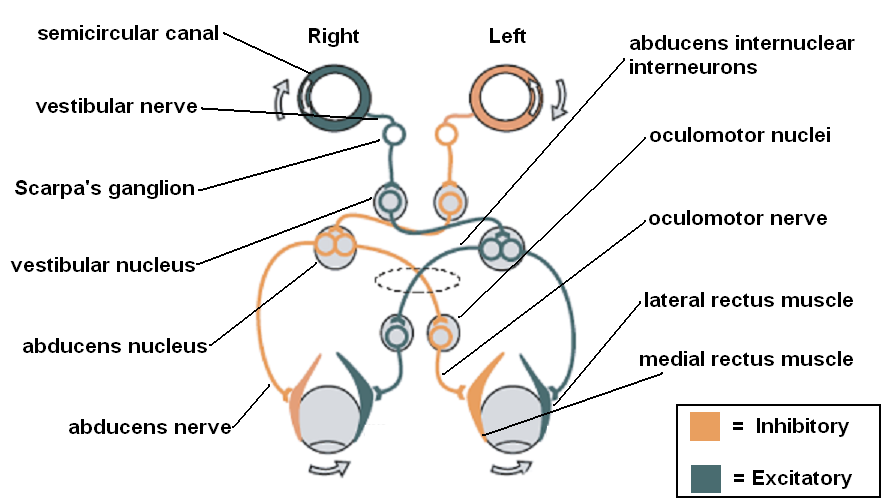
The reflex arc in the doll's eyes reflex has had extensive research. The vestibulo-ocular reflex (VOR) arc consists of a series of brainstem nuclei and the nerves connecting them as well as the vestibular system and the extra-ocular muscles of the eye. In the most simplified version of the reflex arc, angular rotation of the head causes endolymph in the horizontal semi-circular canals to rotate opposite to the direction of the head; this causes the ipsilateral vestibular nerve to activate the ipsilateral vestibular nucleus and the contralateral vestibular nerve to inhibit the contralateral vestibular nucleus. Both vestibular nuclei then activate or inhibit both abducens nuclei, which sends signals to the corresponding ipsilateral lateral rectus and contralateral oculomotor nucleus through the medial longitudinal fasciculus. The oculomotor nuclei then activate or inhibit the corresponding ipsilateral medial recti. Ultimately, the reflex gets elicited if all components of the arc are intact, and a conscious state does not suppress the reflex.[8]
Issues of Concern
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Issues of Concern
The examiner should not perform the reflex on those patients with head or neck injuries that could be further injured by the reflex technique.
Clinical Significance
There are several areas of clinical practice where the doll's eyes reflex has significance:
- Vestibular lesions - Lesions to the vestibular nerve or vestibular nuclei have been shown to impair the ipsilateral doll's eyes reflex.[7]
- Assessing dizziness - The doll's eyes reflex can assess dizziness in the office with rapid vestibular-ocular reflex testing. An abnormal response would show refixation saccades. Found to be 39% sensitive and 97% specific.[4]
- Psychiatric patients - Schizophrenic and bipolar patients can show abnormal smooth pursuit eye movements (SPEMs), both vertical and horizontal. However, there is evidence that these patients should show an intact doll's eyes reflex.[9]
- Intensive care units - The doll's eyes reflex (oculocephalic response) in critically ill intensive care patients can independently predict altered mental status (delirium, coma, confusion) after cessation of sedation.[1]
- Neonates - Most neonates exhibit an unsuppressed doll's eyes reflex before 11.5 weeks; this can serve as a neonatal milestone in neurologic development.[10][2]
- Anesthesia - There appears to be some utility in assessing the doll's eyes reflex in ophthalmologic surgery.[3]
- Nursing - Like other reflexes, nursing staff can receive training on evaluating the doll's eyes reflex in select patients.[11]
Nursing, Allied Health, and Interprofessional Team Interventions
The nurses should know how to elicit the reflex and its prognostic implications. Also, it would be wise to remind the doctor whether a cervical spine injury has been cleared before the reflex is being elicited in a trauma patient.
Media
(Click Image to Enlarge)
References
Sharshar T, Porcher R, Siami S, Rohaut B, Bailly-Salin J, Hopkinson NS, Clair B, Guidoux C, Iacobone E, Sonneville R, Polito A, Aboab J, Gaudry S, Morla O, Amouyal G, Azuar J, Allary J, Vieillard-Baron A, Wolff M, Cariou A, Annane D, Paris-Ouest Study Group on Neurological Effect of Sedation (POSGNES). Brainstem responses can predict death and delirium in sedated patients in intensive care unit. Critical care medicine. 2011 Aug:39(8):1960-7. doi: 10.1097/CCM.0b013e31821b843b. Epub [PubMed PMID: 21532477]
Level 2 (mid-level) evidenceSnir M, Hasanreisoglu M, Goldenberg-Cohen N, Friling R, Katz K, Nachum Y, Benjamini Y, Herscovici Z, Axer-Siegel R. Suppression of the oculocephalic reflex (doll's eyes phenomenon) in normal full-term babies. Current eye research. 2010 May:35(5):370-4. doi: 10.3109/02713680903576708. Epub [PubMed PMID: 20450249]
Wong RV, Craddock MK, Whitten ME. Using the oculocephalic reflex to assess effective retrobulbar anesthesia. Ophthalmic surgery. 1993 May:24(5):339-42 [PubMed PMID: 8515952]
Harvey SA, Wood DJ. The oculocephalic response in the evaluation of the dizzy patient. The Laryngoscope. 1996 Jan:106(1 Pt 1):6-9 [PubMed PMID: 8544630]
Somisetty S, M Das J. Neuroanatomy, Vestibulo-ocular Reflex. StatPearls. 2024 Jan:(): [PubMed PMID: 31424881]
Pullen RL. Checking for oculocephalic reflex. Nursing. 2005 Jun:35(6):24 [PubMed PMID: 15931097]
Foster CA, Foster BD, Spindler J, Harris JP. Functional loss of the horizontal doll's eye reflex following unilateral vestibular lesions. The Laryngoscope. 1994 Apr:104(4):473-8 [PubMed PMID: 8164488]
Ito M. Cerebellar control of the vestibulo-ocular reflex--around the flocculus hypothesis. Annual review of neuroscience. 1982:5():275-96 [PubMed PMID: 6803651]
Level 3 (low-level) evidenceLipton RB, Levin S, Holzman PS. Horizontal and vertical pursuit eye movements, the oculocephalic reflex, and the functional psychoses. Psychiatry research. 1980 Oct:3(2):193-203 [PubMed PMID: 6947312]
Sheth RD, Bodensteiner JB, Riggs JE. The unmodulated oculocephalic reflex: clinical feature of the persistent vegetative state in the neonate. Journal of child neurology. 1996 May:11(3):255-6 [PubMed PMID: 8734036]
Level 3 (low-level) evidenceZegeer LJ. Oculocephalic and vestibulo-ocular responses: significance for nursing care. The Journal of neuroscience nursing : journal of the American Association of Neuroscience Nurses. 1989 Feb:21(1):46-55 [PubMed PMID: 2523440]