Introduction
Facial lacerations are a common complaint in the emergency or primary care setting, and the ear presents a unique challenge due to its structure. The ear is particularly susceptible to lacerations, avulsions, and blunt trauma due to the prominent position of the ears overlying a bony surface. Additionally, the unique composition and relatively tenuous blood supply to the structures of the pinna create challenges and considerations unique to ear laceration repair.
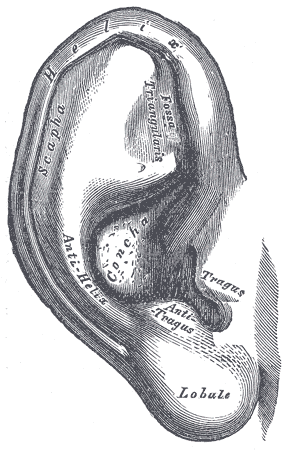
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
An understanding of the ear's anatomy is imperative if the clinician wishes to repair an ear laceration adequately. Most ear lacerations occur on the exposed auricle, also known as the pinna. This is the area of skin-covered cartilage that forms the vast majority of the external ear and which is most prone to injury, although lacerations sometimes extend into the external auditory canal or preauricular areas. The lobule does not have underlying cartilage but rather is made up of fibro adipose tissue surrounded by skin. The cartilage that makes up the auricle is relatively avascular, dependent upon a watershed blood supply, and in continuity with the cartilage of the external auditory canal. The cartilage relies on the perichondrium, the connective tissue that covers the cartilage, for its blood supply. In the absence of trauma, the perichondrium is tightly adherent to the underlying cartilage but has an areolar layer allowing some motion between the perichondrium and overlying skin. The skin of the ear has a dual blood supply, with the anterior portion of the auricle supplied by branches of the superficial temporal artery while the posterior auricular artery supplies the posterior aspect of the pinna as well as the skin overlying the mastoid. Both arteries branch off of the external carotid artery. The posterior auricle also receives some blood supply from collateral branches of the occipital artery. The innervation of the ear is slightly more complicated. The superior and anterior/medial aspects of the auricle are innervated by the auriculotemporal nerve, which is a branch of the trigeminal nerve. The inferior and posterior/lateral aspects of the auricle are dually innervated by the lesser occipital and greater auricular nerves, which arise from the C2 and C3 roots of the cervical plexus. The vagus nerve innervates the majority of the concha with some scattered innervation from the facial nerve. The external auditory canal, including the tympanic membrane, is innervated by branches of the auriculotemporal nerve, the facial nerve, the glossopharyngeal nerve, and the vagus nerve. [1]
Indications
Ideally, ear lacerations should be repaired at the time of presentation, so long as the patient is not presenting more than 24 hours after the injury occurred. If the auricular cartilage is exposed, the ear must be repaired to reduce the risk of complications such as infection, chondritis, necrosis, or deformities such as "cauliflower ear." Delayed closure or a staged repair should be considered in patients who present after 24 hours, patients with evidence of infection about the laceration, patients with relatively devascularized portions of the pinna, and patients at increased risk for infection, for example, patients with uncontrolled diabetes mellitus. Emergency clinicians should refer the patient to otolaryngology or plastic surgery if the patient has an avulsion of the auricle, lacerations extending into the external auditory canal, lacerations associated with internal or middle ear damage, or lacerations concurrent with a skull base fracture. Partial avulsion injuries can be repaired by the primary or emergency clinician as long as there are a wide pedicle and adequate capillary refill at the most distal segment of injury. Narrow pedicle injuries need surgical attention due to the tenuous blood supply.
Contraindications
An overtly infected wound is the primary contraindication to the primary repair of an ear laceration. The physician should also be alert to signs of more serious concurrent injury, such as nausea and vomiting, ataxia, hemotympanum, cerebrospinal fluid (CSF) otorrhea, Battle's sign, or facial nerve dysfunction. These are more common in high-velocity injuries and poly-trauma patients.
Equipment
As with any laceration, the primary materials for repair of a complex ear laceration include forceps, needle drivers, suture, sterile field drapes, buffered lidocaine, 1.5-inch, small-gauge needles (27 to 30 gauge) and syringes for anesthesia, scalpel/scissors, and sterile gauze. For cartilage/perichondrium repair, consider using synthetic, absorbable, sterile, surgical sutures composed of a copolymer made from 90% glycolide and 10% L-lactide or a sterile, synthetic, absorbable monofilament suture made from the polyester (including Monocryl or PDS suture). These will retain tensile strength for at least 30 days and have minimal tissue reactivity. The overlying auricular skin may be closed with 5-0 or 6-0 sutures. Absorbable versus nonabsorbable sutures for skin closure is a physician preference and may depend on the reliability of the patient and the availability of follow up for suture removal, which should occur in 5-7 days.
Preparation
Care should be taken to clean the area around the ear laceration as well as possible prior to initiating the repair. Sterile saline should be used to irrigate the wound with 50 to 100 mL of solution per centimeter of the wound. Anesthetizing the ear with a regional auricular block may provide the patient with greater comfort prior to irrigation, as well as avoiding tissue distortion of the laceration edges. After the wound has been cleaned, a sterile drape should be applied to isolate the field. If necessary, the physician may need to debride or excise macerated or devitalized tissue to create clean wound margins that will hold a suture before attempting the repair.
Technique or Treatment
Physicians should anesthetize the area about the laceration prior to initiating the repair. Anesthesia may be achieved with a regional auricular block or by injecting an anesthetic into or around the wound edges. One advantage of using a regional block is that wound edges will not be distorted by the installation of the anesthetic, and such a block will provide total anesthesia to the majority of the ear, except concha and meatus. To perform a regional auricular block, the physician will instill an anesthetic in a box or diamond shape around the ear. This will be performed by injecting an anesthetic in the shape of a "V," one inferior to the ear, and an inverted "V" superior to the ear. Start by inserting the needle inferior to the ear near the lobule, aiming toward the mastoid process. Withdraw the needle while instilling 1 mL of anesthetic per inch of tissue in a subcutaneous plane to avoid anesthetizing the facial nerve. Using the same technique, insert the needle from the same starting point toward the skin anterior to the tragus and instill an anesthetic while withdrawing the needle. Next, the physician will inject an anesthetic in an inverted "V," starting from the skin superior to the ear, again aiming towards the mastoid, followed by installation of a line of anesthetic from the starting point above the ear towards the skin anterior to the tragus. Allow 5 to 10 minutes for complete anesthesia to occur, and be certain to test the patient's sensation prior to initiating the repair.
Once the patient's wound has been cleaned, prepped, and the area anesthetized, the repair can now begin. Resection of tissue should be minimized, with only obviously devascularized tissues resected prior to repair. The key tenets of repairing a complex ear laceration are properly aligning the cartilage to maintain aesthetics and making sure that overlying skin can adequately cover the cartilage. The cartilage itself is avascular and relies on coverage by the skin to receive its blood supply. To start the repair, make sure that the skin can cover the exposed cartilage. If the skin cannot stretch to cover the cartilage, up to a 5-millimeter triangular wedge of cartilage through the helix can be excised without significantly affecting ear shape/aesthetics and function; anything larger than this may require local flaps for coverage or a staged repair. Small ear lacerations can be sutured with simple interrupted or running sutures through the overlying skin. When there is significant cartilage involvement and deformity of the ear, it is imperative that cartilage is realigned with deep sutures, such as 5-0 Monocryl to reapproximate the injured cartilage in a separate layer. Ideally, sutures should be thrown through the outer perichondrium, rather than through the entirety of the cartilage itself, as the cartilage has a greater tendency to pull through or tear. That said, sutures through the cartilage itself can be used if needed, and horizontal mattress sutures are less prone to cutting/tearing of the cartilage. Deep suture knots should be buried. Try to use as few deep sutures as possible to get a good alignment, as each deep suture acts as a foreign body and increases the likelihood of infection. Next, the physician should close the overlying skin with 5-0 or 6-0 simple interrupted sutures at 2- to 3-millimeter intervals. [2]
Once the laceration has been repaired, it is important to apply a pressure dressing to the ear to prevent hematoma formation. Several modalities can be used. One common method is to apply a petroleum-soaked gauze to the area over the laceration, usually about the antihelix or scapha, and into the helix, and pack it tightly against the adjacent skin. Next, apply a wad of gauze over the entire ear and hold the gauze in place with a gauze bandage wrapped around the patient's head. Another option is to use a series of simple interrupted "quilting" sutures in a through-and-through fashion. This can be done by piercing the posterior aspect of the auricle with a suture and then advancing 1 centimeter superiorly before going back through the anterior aspect of the auricle, tying the knot posteriorly. Space these sutures out by a few millimeters and cover the entire ear surface that may be at risk of hematoma formation. This may also be accomplished in the form of mattress sutures. Bolstering is another option for the prevention of hematoma formation whereby a bolster is stitched against the anterior surface of the auricle. Lastly, a plaster mold of the surface of the auricle can be made to compress the skin surface and prevent hematomas; however, this is more time-intensive and may not be practical in an emergent setting. The bolster and any non-absorbable sutures should be removed in 5-7 days. At this time, no robust data support the routine use of prophylactic antibiotics in ear lacerations, including those with exposed cartilage prior to repair, however, in practice, they are routinely prescribed as the potential outcomes of a wound infection are devastating, and should cover Pseudomonas. [3][4][5]
If a full-thickness laceration leaves only a small pedicle of skin attaching the avulsed portion to the remainder of the ear, consultation with an otolaryngologist or plastic surgeon for repair is indicated. This can be managed either as described above, with meticulous, multi-layer repair, or via staged repair. A staged repair often involves de-epithelializing the avulsed segment and burying it in a postauricular pocket to allow for re-vascularization of the cartilage. A second procedure elevates this construct back onto the pinna and often a posterior skin graft is required. [6] Complete avulsions of the ear can also be treated in this way, though attempts at microvascular re-implantation at the time of injury have also been described. [7]
Complications
As with all lacerations, scarring, infection, pain, and the need for additional repair are potential complications. Chondritis and hematoma formation are complications specific to ear lacerations. Patients should be reevaluated 24 to 48 hours after the repair to assess for the development of these complications. The vast majority of chondritis is provoked by Pseudomonas aeruginosa and should be treated with ciprofloxacin.[8] Lacerations of the external auditory canal put the patient at risk for canal stenosis and acute otitis externa.
Enhancing Healthcare Team Outcomes
While ear lacerations may appear simple, the unique anatomy and relative hypovascularity of the ear lead to several unique challenges with which the clinician must be familiar. Thus, when patients present to the emergency department, it is important to have a very low threshhold to consult with the plastic surgeon or the otolaryngologist. The emergency department physician and nurse practitioner may irrigate the wound and confirm tetanus status, but if there is any question as to the severity of the wound or potential need fo staged procedures, the wound should not be closed until seen by the specialist. A poorly repaired ear laceration can lead to hematoma formation, nerve damage, flap necrosis, and asymmetry that may be irreversible. [9][1][10]
Media
(Click Image to Enlarge)
References
Osetinsky LM, Hamilton GS 3rd, Carlson ML. Sport Injuries of the Ear and Temporal Bone. Clinics in sports medicine. 2017 Apr:36(2):315-335. doi: 10.1016/j.csm.2016.11.005. Epub [PubMed PMID: 28314420]
Lavasani L, Leventhal D, Constantinides M, Krein H. Management of acute soft tissue injury to the auricle. Facial plastic surgery : FPS. 2010 Dec:26(6):445-50. doi: 10.1055/s-0030-1267718. Epub 2010 Nov 17 [PubMed PMID: 21086230]
Greywoode JD, Pribitkin EA, Krein H. Management of auricular hematoma and the cauliflower ear. Facial plastic surgery : FPS. 2010 Dec:26(6):451-5. doi: 10.1055/s-0030-1267719. Epub 2010 Nov 17 [PubMed PMID: 21086231]
Roy S, Smith LP. A novel technique for treating auricular hematomas in mixed martial artists (ultimate fighters). American journal of otolaryngology. 2010 Jan-Feb:31(1):21-4. doi: 10.1016/j.amjoto.2008.09.005. Epub 2009 Mar 26 [PubMed PMID: 19944894]
Level 2 (mid-level) evidenceGiles WC, Iverson KC, King JD, Hill FC, Woody EA, Bouknight AL. Incision and drainage followed by mattress suture repair of auricular hematoma. The Laryngoscope. 2007 Dec:117(12):2097-9 [PubMed PMID: 17921905]
Level 2 (mid-level) evidenceGailey AD, Farquhar D, Clark JM, Shockley WW. Auricular avulsion injuries and reattachment techniques: A systematic review. Laryngoscope investigative otolaryngology. 2020 Jun:5(3):381-389. doi: 10.1002/lio2.372. Epub 2020 Apr 14 [PubMed PMID: 32596480]
Level 1 (high-level) evidenceLin PY, Chiang YC, Hsieh CH, Jeng SF. Microsurgical replantation and salvage procedures in traumatic ear amputation. The Journal of trauma. 2010 Oct:69(4):E15-9. doi: 10.1097/TA.0b013e3181bbd644. Epub [PubMed PMID: 20938253]
Fisher CG, Kacica MA, Bennett NM. Risk factors for cartilage infections of the ear. American journal of preventive medicine. 2005 Oct:29(3):204-9 [PubMed PMID: 16168869]
Level 2 (mid-level) evidenceMenon A, G A. Traumatic Partial Avulsion of Pinna Reconstruction with Limberg Flap. World journal of plastic surgery. 2018 May:7(2):231-234 [PubMed PMID: 30083508]
Brown DJ, Jaffe JE, Henson JK. Advanced laceration management. Emergency medicine clinics of North America. 2007 Feb:25(1):83-99 [PubMed PMID: 17400074]