Definition/Introduction
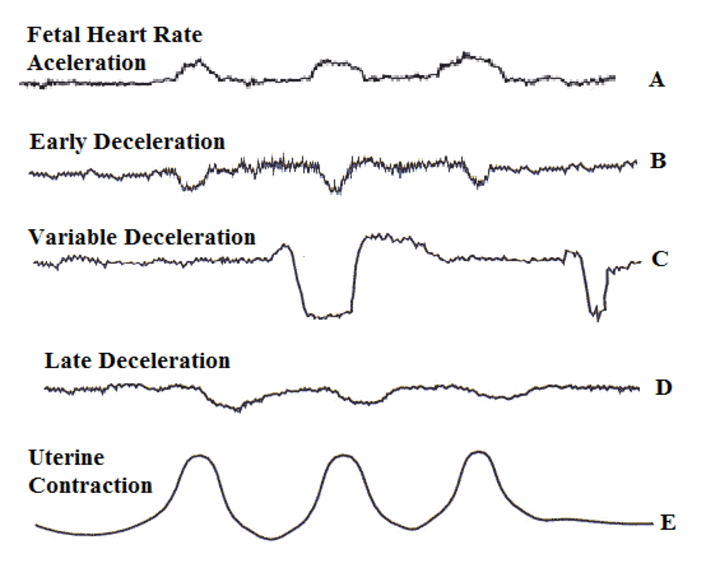
Decelerations are temporary decreases in the fetal heart rate (FHR) during labor. Hon and Quilligan first described three types of decelerations (early, variable, and late) in 1967 based on the shape and timing of decelerations relative to uterine contractions.[1] Intrapartum FHR monitoring allows for the identification of changes associated with fetal distress that allows for early intervention.
Early deceleration is defined as a symmetrical decrease and return of fetal heart rate (FHR) that is associated with a uterine contraction. The decrease is gradual and defined by the onset of deceleration to a nadir of 30 seconds or longer, with the nadir occurring at the same time as the peak of the uterine contraction. In most instances, the onset, nadir, and recovery of the deceleration coincide with the onset, peak, and end of the contraction.[2]
Issues of Concern
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Issues of Concern
An early deceleration always occurs in association with the uterine contraction. Doppler studies have shown that uterine contractions are associated with increased intrauterine pressure and a linear fall in maternal uterine artery blood flow.[3] Decelerations generally appear to be a critical fetal adaptation to intermittent hypoxia to help reduce myocardial work and oxygen requirements.[4][5] Early decelerations, however, had been suggested to represent a non-hypoxic reflex as the result of increased intracranial pressure.[1][6] Multiple studies of head compression in fetal sheep concluded the decelerations to result from a Cushing response secondary to reduced cerebral blood flow and increased intracranial pressure.[7] There is no evidence that mechanical compression of the fetal head by uterine contractions causes cerebral ischemia, neurologic injury, or perinatal stroke.[8] Variable decelerations are caused by direct cord compression, which leads to fetal hypertension, which in turn leads to a decreased fetal heart rate. Late decelerations following the uterine contraction result from uteroplacental insufficiency.
Clinical Significance
Early decelerations are very common and are a benign finding. Early decelerations appear to represent an autonomic response mediated by vagal activation in response to changes in intracranial pressure and cerebral blood flow during a uterine contraction.[6] Fetuses experiencing early decelerations have normal SpO values[9] as well as a low fetal base deficit.[10]
As early decelerations are not associated with decreased fetal oxygenation or metabolic acidosis, they do not require any treatment. However, it is crucial to continue to monitor FHR tracings throughout labor to recognize any patterns that may be a concern regarding changes in the acid-base status of the fetus.
The three-tiered fetal heart rate interpretation system is as follows[2]:
Category I (Must include all of the following):
- Baseline rate: 110 to 160 beats per minute
- Baseline FHR variability: moderate
- Late or variable decelerations absent
- Early decelerations: present or absent
- Accelerations: present or absent
Category II
- All FHR tracings not categorized as Category I or III.
Category III (Includes either):
- Absent baseline FHR variability and any of the following:
- Recurrent late decelerations
- Recurrent variable decelerations
- Bradycardia
- Sinusoidal pattern
Category I FHR tracings are normal and require no specific action. Continued FHR monitoring per the American College of Obstetricians and Gynecologists (ACOG) recommendations allows the team to be vigilant for more concerning FHR tracings. Category II tracings are indeterminate and require an evaluation and continued surveillance and reevaluation. Category III tracings are associated with abnormal fetal acid-base status and require prompt evaluation.
Nursing, Allied Health, and Interprofessional Team Interventions
Current data do not show a clear benefit to the use of continued fetal monitoring over intermittent auscultation, thus either is acceptable for uncomplicated patients. The ACOG recommends continuous FHR monitoring for high-risk patients, such as those with known intrauterine growth restriction or preeclampsia. When using continuous FHR monitoring during labor, recommendations are that nurses and physicians review it frequently. In a patient without complications, the recommendation is that it be reviewed every 30 minutes in the first stage of labor and every 15 minutes during the second stage. In high-risk patients, the tracing requires a review every 15 minutes in the first stage and every 5 minutes in the second stage.[2] [Level V]
Media
References
Hon EH, Quilligan EJ. The classification of fetal heart rate. II. A revised working classification. Connecticut medicine. 1967 Nov:31(11):779-84 [PubMed PMID: 5625136]
. ACOG Practice Bulletin No. 106: Intrapartum fetal heart rate monitoring: nomenclature, interpretation, and general management principles. Obstetrics and gynecology. 2009 Jul:114(1):192-202. doi: 10.1097/AOG.0b013e3181aef106. Epub [PubMed PMID: 19546798]
Level 1 (high-level) evidenceJanbu T, Nesheim BI. Uterine artery blood velocities during contractions in pregnancy and labour related to intrauterine pressure. British journal of obstetrics and gynaecology. 1987 Dec:94(12):1150-5 [PubMed PMID: 3322373]
Fletcher AJ, Gardner DS, Edwards CM, Fowden AL, Giussani DA. Development of the ovine fetal cardiovascular defense to hypoxemia towards full term. American journal of physiology. Heart and circulatory physiology. 2006 Dec:291(6):H3023-34 [PubMed PMID: 16861695]
Level 3 (low-level) evidenceWestgate JA, Wibbens B, Bennet L, Wassink G, Parer JT, Gunn AJ. The intrapartum deceleration in center stage: a physiologic approach to the interpretation of fetal heart rate changes in labor. American journal of obstetrics and gynecology. 2007 Sep:197(3):236.e1-11 [PubMed PMID: 17826402]
Ball RH, Parer JT. The physiologic mechanisms of variable decelerations. American journal of obstetrics and gynecology. 1992 Jun:166(6 Pt 1):1683-8; discussion 1688-9 [PubMed PMID: 1615975]
Fodstad H, Kelly PJ, Buchfelder M. History of the cushing reflex. Neurosurgery. 2006 Nov:59(5):1132-7; discussion 1137 [PubMed PMID: 17143247]
Level 3 (low-level) evidenceRaju TN, Nelson KB, Ferriero D, Lynch JK, NICHD-NINDS Perinatal Stroke Workshop Participants. Ischemic perinatal stroke: summary of a workshop sponsored by the National Institute of Child Health and Human Development and the National Institute of Neurological Disorders and Stroke. Pediatrics. 2007 Sep:120(3):609-16 [PubMed PMID: 17766535]
Puertas A, Navarro M, Velasco P, Montoya F, Miranda JA. Intrapartum fetal pulse oximetry and fetal heart rate decelerations. International journal of gynaecology and obstetrics: the official organ of the International Federation of Gynaecology and Obstetrics. 2004 Apr:85(1):12-7 [PubMed PMID: 15050461]
Hon EH, Khazin AF. Observations on fetal heart rate and fetal biochemistry. I. Base deficit. American journal of obstetrics and gynecology. 1969 Nov 1:105(5):721-9 [PubMed PMID: 5823892]