Introduction
Elbow trauma is a common complaint in the acute care setting. In general, these injuries encompass a vast array of patterns, from mild soft tissue injuries and contusions to complex osseoligamentous injury patterns and terrible triad injuries. In the adult patient, most of these acute injuries occur secondary to high-energy mechanisms such as falls from height or motor vehicle accidents (MVAs). Older patients, however, are at risk for elbow injuries and traumatic fractures following low-energy falls. The latter occurs secondary to many factors, including deconditioning, decreased agility and balance, poor vision, decreased muscle mass, and osteopenia or osteoporosis. As such, the approach to treating elbow trauma may vary considerably based on medical history and physical exam.
Anatomy is important for clinicians treating elbow trauma because of the complexity of range of motion (ROM), ligamentous support, and articulations. The elbow joint is one of the most complex joints in the human body, comprised of 3 distinct articulations: ulnohumeral, radiohumeral, and proximal radioulnar joints.[1] The anterior aspect of the proximal ulna (ie, the trochlear notch or semilunar notch) articulates with the trochlea of the distal humerus on the medial side of the elbow joint. The capitellum, a distinct ossification center at the lateral distal humerus, articulates with the radial head. The radial neck and the proximal radial metaphyseal region include the radial tuberosity, the attachment site of the distal biceps tendon. The ulnar collateral ligament (UCL) and lateral collateral ligament (LCL) complex play an important role in stabilizing the joint to valgus and varus stress throughout the arc of motion. Moreover, these ligaments contribute to the physiologic rotational stability of the elbow joint. The transition between the upper arm and the forearm is the region of the antecubital fossa, which contains the radial nerve, brachial artery, and median nerve.[2][3]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Traumatic Injuries
Traumatic injuries range from simple contusions to more complex osseoligamentous fracture-dislocation patterns. The latter is often seen after a fall on an outstretched hand while the forearm is supinated and the elbow is either partially flexed or fully extended. Direct trauma to the elbow, which often occurs from a fall directly onto the olecranon, can yield various types of fracture- and fracture-dislocation patterns. Additionally, isolated soft tissue injuries can range from mild contusions, sprains, and strains to more significant soft tissue-based injuries requiring clinical attention, such as deep penetrating lacerations or gunshot injuries (GSIs) resulting in traumatic arthrotomies. While simple elbow dislocations often resolve following nonoperative management, some patients develop recurrent dislocations or subluxation episodes. These patients commonly present with painful clicking and weakness.
In summary:
- Soft tissue injuries range from mild, superficial soft tissue injuries (eg, simple contusions, strains, or sprains) to traumatic arthrotomies following GSIs or penetrating lacerations.
- The osseoligamentous spectrum of injury encompasses fractures, fracture-dislocations, ligamentous injuries, and simple versus complex dislocation patterns.
- "Simple" refers to no associated fracture accompanying the dislocation
- "Complex" refers to an associated fracture accompanying the dislocation
- Terrible triad elbow injuries comprise 3 areas
Attritional Injuries
Another form of elbow injury is the subacute-to-chronic variety that occurs secondary to repetitive motions, eventually leading to various tendinosis conditions. These include lateral epicondylitis (tennis elbow) and chronic partial UCL injuries or strains, commonly seen in athletes and present similarly to ligamentous tears in the knee joint.[6] Attritional injuries encompass subacute or chronic presentations following various repetitive motion mechanisms. The injury type is often seen in athletes involved in any upper extremity sport-related activity requiring repetitive motions (eg, baseball pitchers, tennis players). Manual laborers with repetitive occupational demands are prone. Patients with a general complaint of elbow pain undergo an evaluation based on the anatomic region of the elbow.[AAFP. Approach to Elbow Pain]
Pediatric Considerations
Elbow trauma in children most commonly occurs via sports or after falls. The radiographic assessment can be challenging given the characteristic sequence of ossification center appearance and fusion.
Commonly encountered pediatric elbow fractures include (but are not limited to):
- Supracondylar fractures
- Most common in children
- Peak ages 5 to 10 and rarely occur at ages greater than 15
- Extension type (98%): fall on an outstretched hand with fully extended or hyperextended arm
- Type 1: minimal or no displacement
- Type 2: slightly displaced fracture, posterior cortex intact
- Type 3: displaced fracture, posterior cortex broken
- Flexion type: blow directly to a flexed elbow
- Type 1: minimal or no displacement
- Type 2: slightly displaced fracture, anterior cortex intact
- Type 3: displaced fracture, anterior cortex broken
- Lateral condyle fractures
- Medial epicondyle fractures
- Radial head and neck fractures
- Usually, the indirect mechanism (such as a fall on an outstretched hand) and the radial head being driven into capitellum
- Olecranon fractures
- Subluxated radial head (nursemaid elbow)
- Accounts for 20% of all upper extremity injuries in children
- Peak age 1 to 4
- Occurs more frequently in girls than boys
- Mechanism of injury: sudden longitudinal pull on the forearm with the forearm pronated [2]
Epidemiology
Elbow trauma in young adults usually occurs in the setting of sports and following either an acute avulsion injury, ligamentous injury, or insidiously and progressively with chronic repetitive trauma. Weight lifters often sustain sprains and strains injury to the elbow, accounting for 2.6% of all bodily sprains and strains.[7] Sports commonly associated with elbow trauma are those with high impact (skateboarding, inline-skating, skiing) and those involved in overarm-throwing sports such as cricket, baseball, and tennis. Overarm-throwing sports are usually associated with UCL insufficiency.[8]
The epidemiology of elbow trauma in children is interesting due to a trend toward earlier fusion of the joint in girls compared to boys. In girls, most physical fractures occur at the ages of 9 to 12 and 12 to 15 in boys. When examined for specific ages, the boy-to-girl ratio for the incidence of physical fractures varied from 1 to 1 in children aged 11 or younger and 7 to 1 in children older than 11. About 15% of all pediatric fractures are epicondylar fractures, and the peak age incidence is around 6. Elbow dislocation in children is not as common as a fracture; fractures account for 3% to 5% of all pediatric elbow injuries, mostly the posterolateral type. Peak incidence occurs during adolescence in ages 12 to 13.[2][9]
History and Physical
Patients will present acutely with varying degrees of swelling and deformity. Pain and limited ROM are expected. A comprehensive physical examination includes examination from the shoulder to the hand of the ipsilateral extremity. Case reports highlight presentations of some combination of forearm, elbow, and humeral fractures. One such report included the presence of an ipsilateral elbow dislocation, humeral shaft fracture, and shoulder dislocation following high-energy trauma.
The examiner should perform and document relevant findings, including:
- Skin integrity: critical when assessing for the presence of an open fracture and/or traumatic arthrotomy
- Presence of swelling or effusion
- Comprehensive neurovascular examination
How the patient carries their arm may guide the diagnosis. Noting the patient's age, preexisting medical conditions, medication list, and previous history of injury guide the clinician's assessment of the severity of the injury.[10]
Bony Injuries
Supracondylar fractures include the flexion and extension type. In the flexion type, the patient supports the injured forearm with the other arm and elbow in 90º flexion. Loss of the olecranon prominence may be seen. In the extension type, the patient holds the arm at their side in a S-type configuration.
Soft Tissue Injuries
Elbow dislocations include posterior and anterior types. Posterior elbow locations include abnormal prominence of the olecranon. Anterior dislocations include loss of the olecranon prominence. If radial head subluxation is suspected, the elbow is slightly flexed, and the pronated forearm resists movement at the elbow.
Sensory and Motor Testing of the Nerves
A two-point discrimination over the tip of the index finger tests median nerve sensory function. Motor function is tested by asking the patient to make an "OK" sign with the thumb and index finger and abduction of the thumb that is innervated by the recurrent branch. Ulnar nerve sensory function is tested by two-point discrimination of the pinky finger. Motor function is tested by asking the patient to abduct the index finger against resistance applied by the clinician. Neurovascular injuries could also include the anterior interosseous nerve, radial nerve, and brachial artery.
Compartment Syndrome
Acute compartment syndrome can usually develop over a few hours after a serious injury. Some symptoms of acute compartment syndrome are:
- A new persistent deep pain
- Pain that seems greater than expected for the severity of the injury
- Numbness and tingling in the limb
- Swelling, tightness and bruising
Besides acute compartment syndrome, chronic compartment syndrome may develop. Symptoms of chronic compartment syndrome include worsening pain or cramping in the affected muscle within a half-hour of starting an exercise. Symptoms typically go away with rest, and muscle function remains normal. Volkmann ischemic contracture, compartment syndrome of the forearm, could be considered if signs and symptoms are localized more distally.
Clinical features of acute compartment syndrome
The initial suspicion of a diagnosis of acute compartment syndrome (ACS) is mainly clinical. Some classic features include pain, pallor, pulselessness, pressure, paraesthesia, poikilothermia, and paralysis. If the patient has all the features, this could indicate a late diagnosis and irreversible damage because some features, such as paralysis, occur very late in the pathogenesis of ACS. Therefore, a serial assessment is needed to detect a more severe clinical state.
Research has the predictive values of the cardinal features. To calculate the predictive value, Bayes used the following features of ACS: pain, paraesthesia, paresis, and pain on passive movement. All features were more specific than they were sensitive: the mean specificity is 0.97 (range 0.97 to 0.98), and the mean sensitivity is 0.16 (range 0.13 to 0.19). The positive predictive values ranged from 0.11 to 0.15, and all negative predictive values were 0.98. The low positive predictive value suggests that these symptoms are poor indicators of ACS.[11]
When ACS is suspected, a definitive diagnosis involves obtaining the intracompartmental pressure. The assessment is completed through direct, invasive monitoring. When obtaining intracompartmental pressures, a catheter is placed within 5 cm of the fracture level, with the transducer secured at the level of the measured compartment. Keeping the catheter tip outside the actual fracture site is important. If placed within the fracture, levels are falsely high. Failure to place the transducer at the same height as the catheter tip will cause a false high or low, depending upon the position. When the first pressure is normal, but ACS is suspected, a compartment recheck is needed, followed by another pressure assessment.[12] Although beyond the scope of this activity, heightened suspicion is appropriate during the assessment of pediatric patients and infants. Child abuse should be ruled out when applicable.[2]
Evaluation
Radiographic Studies
- Anteroposterior (AP) elbow
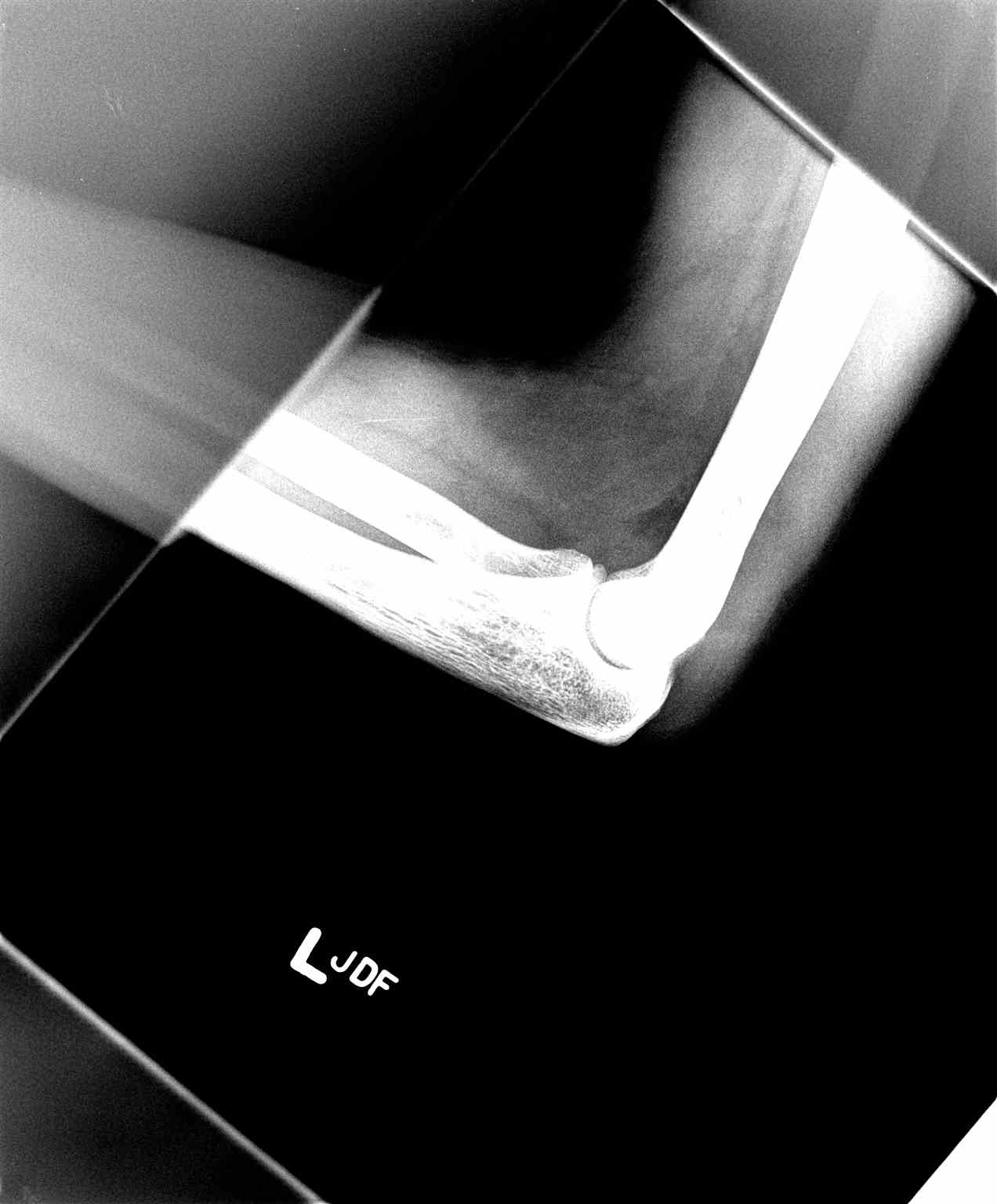
- Lateral elbow (see Image. Lateral Elbow Radiograph)
- Oblique views (optional, depending on fracture/injury)
- Traction view (optional, can facilitate the assessment of comminuted fracture patterns)
- Ipsilateral shoulder-to-wrist orthogonal views: especially in the setting of high-energy trauma or when exam and evaluation are limited
- Fat pad sign:
- Seen with intra-articular injuries
- The anterior fat pad is a narrow radiolucent strip anterior to the humerus. This indicates joint effusion or injury perpendicular to the anterior humeral cortex (sail sign).
- The posterior fat pad is normally not visible and indicates effusion or injury.
- In adults, posterior fat pad sign without other obvious fractures implies radial head fracture.
- In children, the fat pad implies supracondylar fracture.
- Ultrasound is less considered for traumatic injuries but has specific uses for quick assessments or trauma complicated by sepsis.[13][14]
Advanced imaging
Computerized tomography (CT) scans are often a consideration in the setting of comminuted fracture patterns for pre-operative surgical planning. Magnetic resonance imaging (MRI) can be an option in evaluating soft tissue and ligamentous injury or when suspecting stress or occult fractures (see Image. Elbow Fracture on Lateral Radiograph).[2][15][16]
Pediatric Patients
- Fractures in children often occur through unossified cartilage, making radiographic interpretation confusing.
- A line of mensuration drawn down the anterior surface of the humerus should always bisect the capitellum in lateral view.
- If any bony relationship appears vague on radiographs, obtain a comparison view of the contralateral elbow.
- Suspect nonaccidental trauma if history does not indicate injury.
- Ossification centers: the pneumonic CRITOE identifies vulnerable anatomical locations
- Capitellum: 3 to 6 months
- Radial head: 3 to 5 years
- Medial (Internal) epicondyle: 5 to 7 years
- Trochlea: 9 to 10 years
- Olecranon: 9 to 10 years
- Lateral Epicondyle
- Bilateral radiographic imaging is essential in pediatric cases.
- The nurse elbow can be reduced spontaneously when the patient supinates the arm.[17]
Treatment / Management
Mild soft tissue injuries are generally manageable with rest, ice, nonsteroidal anti-inflammatory drugs (NSAIDs), and priority of ROM. The pitfall in managing elbow injuries is that the joint gets stiff quickly. Depending on patient characteristics, formal physical therapy may be recommended to ensure a positive functional outcome (see Image. Imaging Compared to Simple Dislocation). Most fracture patterns with displacement require surgical management with open reduction internal fixation (ORIF), followed by physical therapy postoperatively. Nondisplaced fractures can be treated with a splint initially, and in general, a displacement greater than 2 mm in most fracture patterns requires referral for operative consideration.
Simple elbow dislocations (ie, no associated fracture) can be managed with closed reduction and sling immobilization for 10 to 14 days to prioritize ROM. The treating medical team should be guided by the initial post-reduction examination, including documented ROM and neurovascular status upon successful reduction of the joint. Performing this examination in the acute setting can help guide the duration of joint immobilization in a sling and the possibility of developing posterolateral rotatory instability (PLRI) that presents chronically with painful clicking, weakness, and instability during physical exertion. These patients require operative intervention to mitigate the risk of a poor outcome.[2][9](B3)
Emergency Treatment and Procedures
- Orthopedic consultation is the standard, but nondisplaced, stable fractures can be splinted 24 to 48 hours after orthopedic follow-up.
- Fractures generally requiring orthopedic consultation:
- Transcondylar, intercondylar, condylar, epicondylar fractures
- Fractures involving articular surfaces such as capitellum or trochlea
- Terrible triad
- Supracondylar fractures:
- Emergency clinicians can handle type 1 with 24 to 48 hours of orthopedic follow-up
- The elbow may be flexed and splinted with a posterior splint
- Types 2 and 3 require an immediate orthopedic consult
- Reduce type 2 and 3 in the emergency department when the fracture is associated with vascular compromise
- Anterior dislocation: Reduce immediately if vascular structures are compromised. Then, flex to 90º and place the posterior splint.
- Posterior dislocation: Reduce immediately if vascular structures are compromised. Then, flex 90º and place the posterior splint.
- Radial head fracture: Minimally displaced fractures may need aspiration to remove hemarthrosis. Instill bupivacaine and immobilize. Other types should undergo an orthopedic consult.
- Radial head subluxation
- In one continuous motion, supinate and flex the elbow while placing slight pressure on the radial head.
- The hyperpronation technique is possibly more effective. When grasping the patient’s elbow, the wrist is hyper-pronated until a palpable click is felt.
- A palpable click will often accompany the reduction.
- If the exam suggests fracture, but the radiograph is negative, splint and have the patient follow up in 24 to 48 hours for re-evaluation.[18]
Medications
- Conscious sedation is often necessary for reductions, given the traction on a joint with neurovascular structures.
- Ibuprofen: 600 to 800 mg (pediatric: 5 to 10 mg/kg) PO TID
- Naprosyn: 250 to 500 mg (pediatric: 10 to 20 mg/kg) PO BID
- Tylenol with codeine: 1 or 2 tabs (pediatric 0.5 to 1 mg/kg codeine) PO: do not exceed acetaminophen 4 g/24 hours
- Morphine sulfate: 0.1 mg/kg IV
- Hydromorphone: 5 mg/acetaminophen 300 mg
- Hydrocodone/acetaminophen: 1 to 2 tabs PO
Attritional injuries management modalities
Treatment for repetitive trauma, such as lateral epicondylitis or tendonitis, demonstrates successful outcomes with nonoperative management modalities.
These include but are not limited to:
- Rest, ice, and NSAIDs
- Physical therapy when appropriate
- Eccentric exercises for lateral epicondylitis
- Corticosteroid injection, when applicable
- Platelet-rich plasma (PRP) considerations
Disposition
The disposition criteria for admission include vascular injuries, open fractures requiring operative reduction, or internal fixation. Patients with extensive swelling or ecchymosis require observation and elevation to monitor or decrease the risk of compartment syndrome. Discharge criteria depend on whether any stable fractures or reduced dislocations have deteriorated. Orthopedic follow-up is indicated within 24 to 48 hours. Uncomplicated soft tissue injuries can continue to be managed supportively.[21](B3)
Follow-Up
Prolonged elbow immobilization can cause stiffness in the patient, so the main goal is to restore the ROM as soon as possible. The Mayo Elbow Performance Score (MEPS) has recently demonstrated strong reliability in measuring outcomes after surgery.[22](B3)
Differential Diagnosis
The following diagnoses should be considered:
- Fracture
- Dislocation
- Sprain
- Strain
- Ligamentous insufficiencies (eg, UCL)
- Bursitis
- Tendinopathic conditions (acute or chronic)
The differential for pediatric patients should include:
- Child abuse
- Distal humeral physeal injuries
- Nursemaid elbow
- Fracture(s)
- Avulsions
- Monteggia fracture-dislocations
- Physeal injuries/reactions
Prognosis
The treated fracture usually has a good prognosis. Some patients may demonstrate loss of terminal extension about 10° to 15°, but this is not clinically significant. Dislocation can cause nerve or vascular compression; early management minimizes the complication. Patients with bursitis have a good prognosis. A systemic infection may result from infectious bursitis, but the risk is low.[23]
Complications
The most common complications are neurovascular following fracture and dislocation. Transient ulnar neuropathy incidence is 10%. Another less common complication is median nerve entrapment. Vascular complications such as reduction or obliteration of the radial pulse may occur. Prolonged immobilization of the elbow can cause stiffness and terminal extension loss, which can be problematic, especially in children and athletes.[2][15]
Deterrence and Patient Education
Patients are encouraged to follow instructions and post-injury or post-operative rehabilitation protocols as the treating clinician dictates. Also, in complex elbow injury patterns and traumatic fracture-dislocations (ie, terrible triad elbow injuries), managing patient expectations is important. Nearly all patients experience post-recovery loss of ROM. Thus, ROM should be emphasized as an indicator of prognosis.
Enhancing Healthcare Team Outcomes
A thorough evaluation of elbow trauma by the treating clinician and consulting team is vital for optimal patient outcomes. Radiographic evaluation of elbow trauma is essential in the acute setting, and a firm understanding of anatomy, radiographic landmarks, and common injuries is necessary. Radiography and MRI are vital diagnostic tools for chronic elbow overuse injuries. Narrowing the diagnosis and not delaying treatment can reduce unwanted complications. Appropriate management requires an interprofessional approach to achieve optimal patient outcomes.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Fliegel BE, Ekblad J, Varacallo M. Anatomy, Shoulder and Upper Limb, Elbow Annular Ligament. StatPearls. 2024 Jan:(): [PubMed PMID: 30860729]
Iyer RS, Thapa MM, Khanna PC, Chew FS. Pediatric bone imaging: imaging elbow trauma in children--a review of acute and chronic injuries. AJR. American journal of roentgenology. 2012 May:198(5):1053-68. doi: 10.2214/AJR.10.7314. Epub [PubMed PMID: 22528894]
Wilps T, Kaufmann RA, Yamakawa S, Fowler JR. Elbow Biomechanics: Bony and Dynamic Stabilizers. The Journal of hand surgery. 2020 Jun:45(6):528-535. doi: 10.1016/j.jhsa.2020.01.016. Epub 2020 Apr 13 [PubMed PMID: 32299691]
van Riet RP. Assessment and decision making in the unstable elbow: management of simple dislocations. Shoulder & elbow. 2017 Apr:9(2):136-143. doi: 10.1177/1758573216686533. Epub 2017 Jan 29 [PubMed PMID: 28405226]
Ohl X, Siboni R. Surgical treatment of terrible triad of the elbow. Orthopaedics & traumatology, surgery & research : OTSR. 2021 Feb:107(1S):102784. doi: 10.1016/j.otsr.2020.102784. Epub 2021 Jan 9 [PubMed PMID: 33333276]
Gehrman MD, Grandizio LC. Elbow Ulnar Collateral Ligament Injuries in Throwing Athletes: Diagnosis and Management. The Journal of hand surgery. 2022 Mar:47(3):266-273. doi: 10.1016/j.jhsa.2021.11.026. Epub [PubMed PMID: 35246298]
Burekhovich SA, Newman JM, Shah NV, Onuoha KO, Le C, Persaud CS, Naziri Q, Sodhi N, Chaudhri M, Joseph NS, Basu NN, Urban WP, Zikria BA. Epidemiology and Trends of Weightlifting-Related Sprains and Strains that Presented to Emergency Departments in the United States. Journal of long-term effects of medical implants. 2018:28(2):111-117. doi: 10.1615/JLongTermEffMedImplants.2018026168. Epub [PubMed PMID: 30317960]
Saper MG, Pierpoint LA, Liu W, Comstock RD, Polousky JD, Andrews JR. Epidemiology of Shoulder and Elbow Injuries Among United States High School Baseball Players: School Years 2005-2006 Through 2014-2015. The American journal of sports medicine. 2018 Jan:46(1):37-43. doi: 10.1177/0363546517734172. Epub 2017 Oct 19 [PubMed PMID: 29048928]
Gupta G, Makadia AS, Shah MM. An Unreported Variant of Convergent Dislocation of Elbow. Journal of orthopaedic case reports. 2018 Nov-Dec:8(6):79-81. doi: 10.13107/jocr.2250-0685.1268. Epub [PubMed PMID: 30915301]
Level 3 (low-level) evidenceAiyer A, Varacallo M, Boateng H, Reid JS. Humeral Shaft Fracture with Ipsilateral Anterior Shoulder Dislocation and Posterior Elbow Dislocation: A Case Report and Review of the Literature. JBJS case connector. 2014 Sep 10:4(3):e77. doi: 10.2106/JBJS.CC.M.00310. Epub [PubMed PMID: 29252297]
Level 3 (low-level) evidenceMabvuure NT, Malahias M, Hindocha S, Khan W, Juma A. Acute compartment syndrome of the limbs: current concepts and management. The open orthopaedics journal. 2012:6():535-43. doi: 10.2174/1874325001206010535. Epub 2012 Nov 30 [PubMed PMID: 23248724]
Duckworth AD, McQueen MM. The Diagnosis of Acute Compartment Syndrome: A Critical Analysis Review. JBJS reviews. 2017 Dec:5(12):e1. doi: 10.2106/JBJS.RVW.17.00016. Epub [PubMed PMID: 29206684]
Hultman KL, Goldman BH, Nazarian LN, Ciccotti MG. Ultrasound Examination Techniques for Elbow Injuries in Overhead Athletes. The Journal of the American Academy of Orthopaedic Surgeons. 2021 Mar 15:29(6):227-234. doi: 10.5435/JAAOS-D-20-00935. Epub [PubMed PMID: 33273401]
Blanco P, Menéndez MF, Figueroa L, Provasi J, Blaivas M. Ultrasound-aided diagnosis of septic arthritis of the elbow in the emergency department. Journal of ultrasound. 2022 Jun:25(2):315-318. doi: 10.1007/s40477-020-00506-2. Epub 2020 Jul 15 [PubMed PMID: 32671656]
Burnier M, Barlow JD, Sanchez-Sotelo J. Shoulder and Elbow Fractures in Athletes. Current reviews in musculoskeletal medicine. 2019 Mar:12(1):13-23. doi: 10.1007/s12178-019-09530-0. Epub [PubMed PMID: 30706285]
Alidina S, Alidina J, Souza F, Kalandiak S, Subhawong TK. Radiographic Evaluation of Elbow Fractures. Seminars in musculoskeletal radiology. 2021 Aug:25(4):529-537. doi: 10.1055/s-0041-1731083. Epub 2021 Oct 27 [PubMed PMID: 34706382]
Chauvin NA, Gustas-French CN. Magnetic resonance imaging of elbow injuries in children. Pediatric radiology. 2019 Nov:49(12):1629-1642. doi: 10.1007/s00247-019-04454-w. Epub 2019 Nov 4 [PubMed PMID: 31686169]
Gottlieb M. Managing Elbow Dislocations. Annals of emergency medicine. 2022 Nov:80(5):460-464. doi: 10.1016/j.annemergmed.2022.04.029. Epub 2022 Jun 16 [PubMed PMID: 35717272]
Dines JS, Williams PN, ElAttrache N, Conte S, Tomczyk T, Osbahr DC, Dines DM, Bradley J, Ahmad CS. Platelet-Rich Plasma Can Be Used to Successfully Treat Elbow Ulnar Collateral Ligament Insufficiency in High-Level Throwers. American journal of orthopedics (Belle Mead, N.J.). 2016 Jul-Aug:45(5):296-300 [PubMed PMID: 27552453]
Pitzer ME, Seidenberg PH, Bader DA. Elbow tendinopathy. The Medical clinics of North America. 2014 Jul:98(4):833-49, xiii. doi: 10.1016/j.mcna.2014.04.002. Epub [PubMed PMID: 24994055]
Heifner JJ, Mercer DM. Improved Understanding of Traumatic Complex Elbow Instability. Journal of the American Academy of Orthopaedic Surgeons. Global research & reviews. 2023 Sep 1:7(9):. doi: 10.5435/JAAOSGlobal-D-23-00041. Epub 2023 Sep 22 [PubMed PMID: 37747701]
Level 3 (low-level) evidenceBaessler A, Eason RR, Joyce MR, Dibaba DT, Wan JY, Azar FM, Brolin TJ, Throckmorton TW. Reliability Testing of the Mayo Elbow Performance Score in Post-operative Patients. Journal of surgical orthopaedic advances. 2022 Winter:31(4):229-232 [PubMed PMID: 36594979]
Level 3 (low-level) evidencePangia J, Rizvi TJ. Olecranon Bursitis. StatPearls. 2024 Jan:(): [PubMed PMID: 29262058]