Introduction
The skin is the largest organ in the body, covering its entire external surface. The skin has 3 layers—the epidermis, dermis, and hypodermis, which have different anatomical structures and functions (see Image. Cross Section, Layers of the Skin). The skin's structure comprises an intricate network that serves as the body's initial barrier against pathogens, ultraviolet (UV) light, chemicals, and mechanical injury. This organ also regulates temperature and the amount of water released into the environment.
Skin thickness varies by body region and is influenced by the thickness of the epidermal and dermal layers. Hairless skin in the palms of the hands and soles of the feet is the thickest due to the presence of the stratum lucidum, an extra layer in the epidermis. Regions lacking this extra layer are considered thin skin. Of these regions, the back has the thickest skin because it has a thick epidermis.[1][2][3] The skin's barrier function makes it susceptible to various inflammatory and infectious conditions. In addition, wound healing, sensory changes, and cosmesis are significant surgical concerns. Understanding the skin's anatomy and function is crucial for managing conditions across all medical fields.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
Epidermis
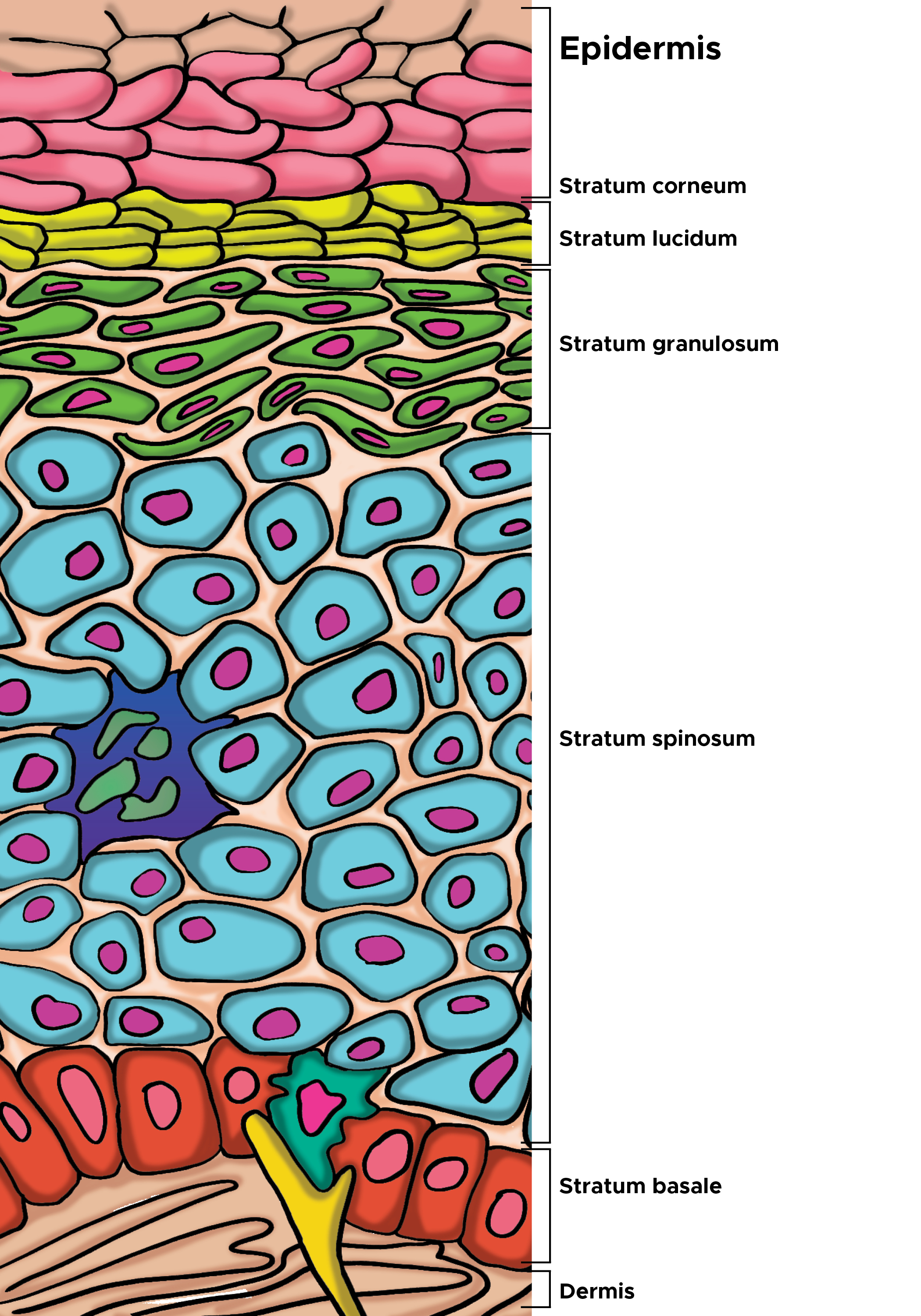
The epidermis, the skin's outermost layer, is composed of several strata and various cell types crucial for its function.
Layers of the epidermis: From the deepest to the most superficial, the epidermal layers are the stratum basale, stratum spinosum, stratum granulosum, stratum lucidum, and stratum corneum. The stratum basale, also known as stratum germinativum, is separated from the dermis by the basement membrane (basal lamina) and attached to it by hemidesmosomes. The cells in this layer are cuboidal to columnar, mitotically active stem cells that constantly produce keratinocytes. This layer also contains melanocytes. The stratum spinosum, comprising 8 to 10 cell layers, is also called the prickle cell layer. This layer contains irregular, polyhedral cells with cytoplasmic processes, sometimes called spines, that extend outward and contact neighboring cells by desmosomes. Dendritic cells can be found in this layer.[4][5]
The stratum granulosum has 3 to 5 cell layers and contains diamond-shaped cells with keratohyalin and lamellar granules. Keratohyalin granules contain keratin precursors that aggregate, cross-link, and form bundles. The lamellar granules contain the glycolipids secreted to the cell surfaces, functioning as an adhesive to maintain cellular cohesion. The stratum lucidum comprises 2 to 3 cell layers and is present in thicker skin on the palms and soles. This thin and clear layer consists of eleidin, a transformation product of keratohyalin. The stratum corneum has 20 to 30 cell layers and occupies the uppermost epidermal layer. The stratum corneum is composed of keratin and dead keratinocytes (anucleate squamous cells) that form horny scales. This layer has the most variable thickness, especially in callused skin. Dead keratinocytes release defensins within this layer, which are part of our first line of immune defense mechanisms.[6][7]
Cells of the epidermis: The epidermal cells include keratinocytes, melanocytes, and Langerhans and Merkel cells (see Image. Cells of the Epidermis). Keratinocytes are the predominant cells of the epidermis, originating from the basal layer. These cells produce keratin and lipids essential for forming the epidermal water barrier. Keratinocytes also contribute to calcium regulation by enabling UVB light absorption in the skin, which is critical for vitamin D activation. Melanocytes derive from neural crest cells and primarily synthesize melanin, the main skin pigment component. These cells are found between stratum basale cells. UVB light stimulates melanin secretion, protecting against further UV radiation exposure and acting as a built-in sunscreen. Melanin forms during the conversion of tyrosine to dihydroxyphenylalanine by the enzyme tyrosinase. Melanin then travels from cell to cell, relying on the long processes connecting the melanocytes to the neighboring epidermal cells. Melanin granules from melanocytes transit through the lengthy processes to the cytoplasm of basal keratinocytes. This transfer occurs through cytocrine secretion, where keratinocytes phagocytose the tips of melanocyte processes.
Langerhans cells are dendritic cells that act as the skin's first-line cellular immune defenders and are crucial for antigen presentation. Special stains allow visualization of these cells in the stratum spinosum. Langerhans cells are of mesenchymal origin, derived from CD34-positive bone marrow stem cells, and are part of the mononuclear phagocytic system. These cells contain Birbeck granules and tennis racket-shaped cytoplasmic organelles. Langerhans cells express major histocompatibility complex (MHC) I and MHC II molecules, uptake antigens in the skin, and transport them to the lymph nodes. Merkel cells are oval-shaped modified epidermal cells found in the stratum basale, directly above the basement membrane. These cells serve as mechanoreceptors for light touch and are found in the palms, soles, and oral and genital mucosa, with the highest concentration in the fingertips. Merkel cells bind to adjoining keratinocytes through desmosomes and contain intermediate keratin filaments. The cell membranes of Merkel cells interact with free nerve endings in the skin.
Dermis
The dermis is connected to the epidermis by the basement membrane. The dermis consists of 2 connective tissue layers, papillary and reticular, which merge without clear demarcation. The papillary layer is the upper dermal layer, which is thinner and composed of loose connective tissue that contacts the epidermis. The reticular layer is the deeper layer, which is thicker and less cellular. This layer consists of dense connective tissue composed of collagen fiber bundles. The dermis houses the sweat glands, hair, hair follicles, muscles, sensory neurons, and blood vessels.
Hypodermis
The hypodermis, also known as the subcutaneous fascia, is located beneath the dermis. This layer is the deepest skin layer and contains adipose lobules, sensory neurons, blood vessels, and scanty skin appendages, such as hair follicles.
Functions
The skin's comprehensive roles highlight its complexity and importance in maintaining overall health and well-being. These roles are discussed below.[8][9]
Barrier function: The skin has multiple protective roles, acting as a barrier against various external threats. The skin shields the body from excessive water loss or absorption, invasion by microorganisms, mechanical and chemical trauma, and UV light damage. The cell envelope establishes the epidermal water barrier, a layer of insoluble proteins on the inner surface of the plasma membrane. This barrier is formed through the cross-linking of small proline-rich proteins. Larger proteins such as cystatin, desmoplakin, and filaggrin contribute to the barrier's robust mechanics. The lipid envelope is a hydrophobic layer attached to the outer surface of the plasma membrane. Keratinocytes in the stratum spinosum produce keratohyalin granules and lamellar bodies containing a mixture of glycosphingolipids, phospholipids, and ceramides assembled within Golgi bodies. The contents of lamellar bodies are then secreted through exocytosis into the extracellular spaces between the stratum granulosum and corneum.
Immunological defense: The skin plays a crucial role in both adaptive and innate immunity. In adaptive immunity, antigen-presenting cells initiate T-cell responses, leading to increased levels of helper T cells, such as TH1, TH2, or TH17. In innate immunity, the skin produces various peptides with antibacterial and antifungal properties. The skin-associated lymphoid tissue is a significant component of the immune system, aiding in preventing infections, as even minor skin breaks can lead to infection. Langerhans cells are part of the adaptive immune system, presenting foreign antigens encountered in the skin to T cells.
Regulation of homeostasis: The skin plays a vital role in maintaining body temperature and water balance. This organ regulates heat exchange with the environment, particularly through the blood vessels and sweat glands. The skin manages the rate and amount of water evaporation and absorption.
Endocrine and exocrine functions: Keratinocytes produce vitamin D by converting 7-dehydrocholesterol under UV light exposure. These cells also express the vitamin D receptor and contain enzymes that activate vitamin D, essential for the proliferation and differentiation of keratinocytes. The skin's exocrine functions include temperature control by perspiration and skin protection by sebum production. Sweat and sebaceous glands are crucial to these functions.
Sensory functions: The skin is equipped with nociceptors that allow for the sensation of touch, heat, cold, and pain, facilitating interaction with the environment. The skin's sensory roles are essential for an individual's movement, protection, and interaction with the environment.
Diagnostic indicator: Skin characteristics such as pigmentation, smoothness, elasticity, and turgor provide insights into an individual's overall health status. Skin assessment is often a crucial part of a person's physical examination.[10][11]
Cell division, desquamation, and shedding in the skin: Cell division occurs in the stratum basale. Basal cells (young keratinocytes) begin the synthesis of keratinous tonofilaments, which are grouped into bundles called tonofibrils. Older keratinocytes are then pushed into the stratum spinosum after mitosis. Skin cells begin to produce keratohyalin granules with intermediate-associated proteins, filaggrin, and trichohyalin in the upper part of the spinous layer. This process helps aggregate keratin filaments and convert granular cells into cornified cells, known as keratinization. Cells also produce lamellar bodies during this stage.
Keratinocytes continue to move into the stratum granulosum afterward, where they become flattened and diamond-shaped. The cells accumulate keratohyalin granules mixed between tonofibrils. Keratinocytes then continue to the stratum corneum, flattening and losing organelles and nuclei. The keratohyalin granules turn tonofibrils into a homogenous keratin matrix. Cornified cells reach the surface and are desquamated when desmosomes disintegrate. The proteinase activity of kallikrein-related serine peptidase is triggered by lowered pH near the surface. The processes of skin shedding and desquamation vary slightly by body region. Hairless skin comprises more layers, with the addition of the stratum lucidum. Thus, keratinocytes in body regions with hairless skin go through more layers before reaching the surface.[12][13]
Embryology
The epidermis is derived from ectodermal tissue. The dermis and hypodermis are derived from mesodermal tissue from somites. The mesoderm is also responsible for the formation of Langerhans cells. Neural crest cells, responsible for specialized sensory nerve endings and melanocyte formation, migrate into the epidermis during epidermal development.[14][15]
Blood Supply and Lymphatics
Blood vessels and lymphatic vessels are found in the skin's dermal layer. Blood supply to the skin comprises 2 plexuses—one between the papillary and reticular dermal layers and another between the dermis and subcutaneous tissues. Blood supply to the epidermis is through the superficial arteriovenous plexus (subepidermal/papillary plexus). These vessels are important for temperature regulation. The body regulates temperature by increasing blood flow to the skin, transferring heat from the body to the environment. The autonomic nervous system controls the changes in blood flow. Sympathetic stimulation results in vasoconstriction, resulting in heat retention. Conversely, vasodilation leads to heat loss. Vasodilation is the body's response to increased body temperature, resulting from inhibiting the sympathetic centers in the posterior hypothalamus. In contrast, decreased body temperature causes vasoconstriction.[16][17]
Nerves
Nerves of the skin include both somatic and autonomic nerves. The somatic sensory system transmits pain (nociception), temperature, light touch, discriminative touch, vibration, pressure, and proprioception sensations to the central nervous system. Specialized cutaneous receptors and end organs mediate perception, including Merkel disks and Pacinian, Meissner, and Ruffini corpuscles. Autonomic innervation controls vasculature tone, hair root pilomotor stimulation, and sweating. The free nerve endings extend into the epidermis and are responsible for sensing pain, heat, and cold. These sensory structures are most numerous in the stratum granulosum layer and around most hair follicles. Merkel disks sense light touch and reaches the stratum basale layer. The other nerve endings are found in the deeper portions of the skin and include the Pacinian, Meissner, and Ruffini corpuscles. The Pacinian corpuscles sense deep pressure. The Meissner corpuscles sense low-frequency stimulation at the level of the dermal papillae. The Ruffini corpuscles sense pressure.[18][19][20]
Muscles
The arrector pili muscles are bundles of smooth muscle fibers attached to the connective tissue sheath of hair follicles. Contraction of these muscles pulls the hair follicle outward, erecting the hair. The arrector pili also compress the sebaceous glands, facilitating sebum secretion. Hair does not exit perpendicularly but at an angle. The erection of hair, known as piloerection, produces goosebumps, giving the skin a bumpy appearance when exposed to cold temperatures.[21] Studies show that piloerection contributes to thermoregulation and stem cell growth.[22]
Surgical Considerations
Langer lines, also known as cleavage lines, are topological lines used to define skin tension. These lines correspond to the alignment of collagen and elastic fibers in the reticular dermis. Less scarring occurs if surgical incisions are made along these lines.[23]
Clinical Significance
The skin's clinical significance spans all medical disciplines. A few are discussed below.
Dermatomes
Dermatomes are skin segments divided based on afferent nerve distribution, numbered according to spinal vertebral levels. Spinal nerves comprise 8 cervical, 12 thoracic, 5 lumbar, 5 sacral, and 1 coccygeal nerve. Diseases such as shingles caused by varicella-zoster infection manifest pain and rashes in dermatomal patterns. Dermatomes also aid in localizing spinal injuries.
Squamous Cell Carcinoma
Squamous cell carcinoma is a malignancy arising from mutated keratinocytes, typically due to UV damage in individuals with type I or II skin types. These individuals typically have light skin, blue or green eyes, and red or blonde hair and burn without tanning. The lesions often appear as scaly, flaky, thick red patches that may bleed. Some squamous cell carcinoma tumors resemble warts. This type of skin cancer can metastasize. Squamous cell carcinoma often arises from actinic keratoses—premalignant lesions with cutaneous horns developing from chronic UV damage.[24]
Basal Cell Carcinoma
Basal cell carcinoma is a malignant neoplasm of the basal layers of the epidermis. Unlike squamous cell carcinoma, it is much less likely to metastasize. This type of skin cancer is more common in sun-exposed areas, often appearing as pearly papules on the face, with telangiectasias and a great tendency to ulcerate.
Melanoma
Melanoma is a highly invasive malignant melanocyte tumor that is fatal but rarer than skin squamous cell carcinoma and basal cell carcinoma. This neoplasm's high metastatic potential is significantly mediated by lesion depth. Melanoma can be found anywhere on the body and is typically irregularly pigmented but can be amelanotic.[25]
Langerhans Cell Histiocytosis
Langerhans cell histiocytosis is a type of cancer in which Langerhans cells accumulate in the body and form granulomas, often in the bones, causing bone pain. These granulomas can also appear in the skin, producing rashes, erythematous papules, or blisters (see Image. Histology, Trichodysplasia Spinulosa). Notably, Langerhans cell histiocytosis can affect the pituitary gland, leading to diabetes insipidus, infertility, or other endocrine disorders due to hormone deficiencies. Pancytopenia is a potentially fatal Langerhans cell histiocytosis complication, manifesting with anemia, thrombocytopenia, and leukocytopenia, caused by overcrowding of Langerhans cells in the bone marrow.[26]
Merkel Cell Carcinoma
Merkel cell carcinoma is an uncommon cancer of the Merkel cells. This tumor is categorized as a neuroendocrine small cell carcinoma. Clinically, Merkel cell carcinoma often presents as a painless, solitary cutaneous or subcutaneous nodule, sometimes with a cystic appearance. The nodule can be red, pink, violet, blue, or skin-colored. Lesions may ulcerate or have satellite lesions. Merkel cell carcinoma is typically smaller than 20 mm at diagnosis but shows rapid tumor growth over a few months.[27]
Pemphigus Vulgaris
Pemphigus vulgaris is an autoimmune disease that targets the desmosomes, the intercellular proteins connecting keratinocytes. Desmosome degradation results in acantholysis and the formation of easily ruptured blisters within the epidermis. The disease is characterized by a positive Nikolsky sign, where the epidermis peels away upon rubbing.
Bullous Pemphigoid
Bullous pemphigoid is a blistering disease that affects older adults, causing tense subepidermal blisters. The condition is caused by antibodies targeting hemidesmosomes, which connect the epidermis to the dermis at the basement membrane. This condition is not acantholytic and does not show a positive Nikolsky sign.[28]
Scalded Skin Syndrome
Scalded skin syndrome arises from the effects of the exfoliative toxin released by Staphylococcal aureus. The condition manifests as generalized skin exfoliation with a positive Nikolsky sign, a severely burned (intensely red) appearance, and fever.[29][30]
Drug Reactions
Various drug reactions manifest in the skin, including erythema multiforme and the syndromes of drug reaction with eosinophilia and systemic symptoms, Stevens-Johnson, and toxic epidermal necrolysis. These conditions are often associated with certain medications, including sulfa-containing drugs, nonsteroidal anti-inflammatory drugs, and antiepileptics.[31][32]
Other Issues
The epidermis contains much of our normal flora, with the microbiome varying by body region. The microorganisms inhabiting our skin surfaces are nonpathogenic and can be commensal or mutualistic. The bacteria that tend to predominate are Staphylococcus epidermidis and S aureus, Cutibacterium acnes, Corynebacterium, Streptococcus, Candida, and Clostridium perfringens. However, infections may occur when the protective skin barrier is altered or breached.[33]
Media
(Click Image to Enlarge)

Histology, Trichodysplasia Spinulosa. The left column shows hematoxylin and eosin staining of healthy skin (A1) and trichodysplasia spinulosa lesional skin (B1) at low power. At high power, healthy (A2) and trichodysplasia spinulosa (B2) epidermis and hair follicles (A3 and B3) are depicted. An enlarged and dysmorphic hair follicle is evident in B3, containing eosinophilic granular protein deposits in the cytoplasm of cells (arrowheads in inset) with abrupt cornification in the follicle center. Bars represent 100 µm.
Kazem S, van der Meijden E, Wang RC, et al. Polyomavirus-associated trichodysplasia spinulosa involves hyperproliferation, pRB phosphorylation and upregulation of p16 and p21. PLoS ONE. 2014;9(10):e108947. doi: 10.1371/journal.pone.0108947.
(Click Image to Enlarge)
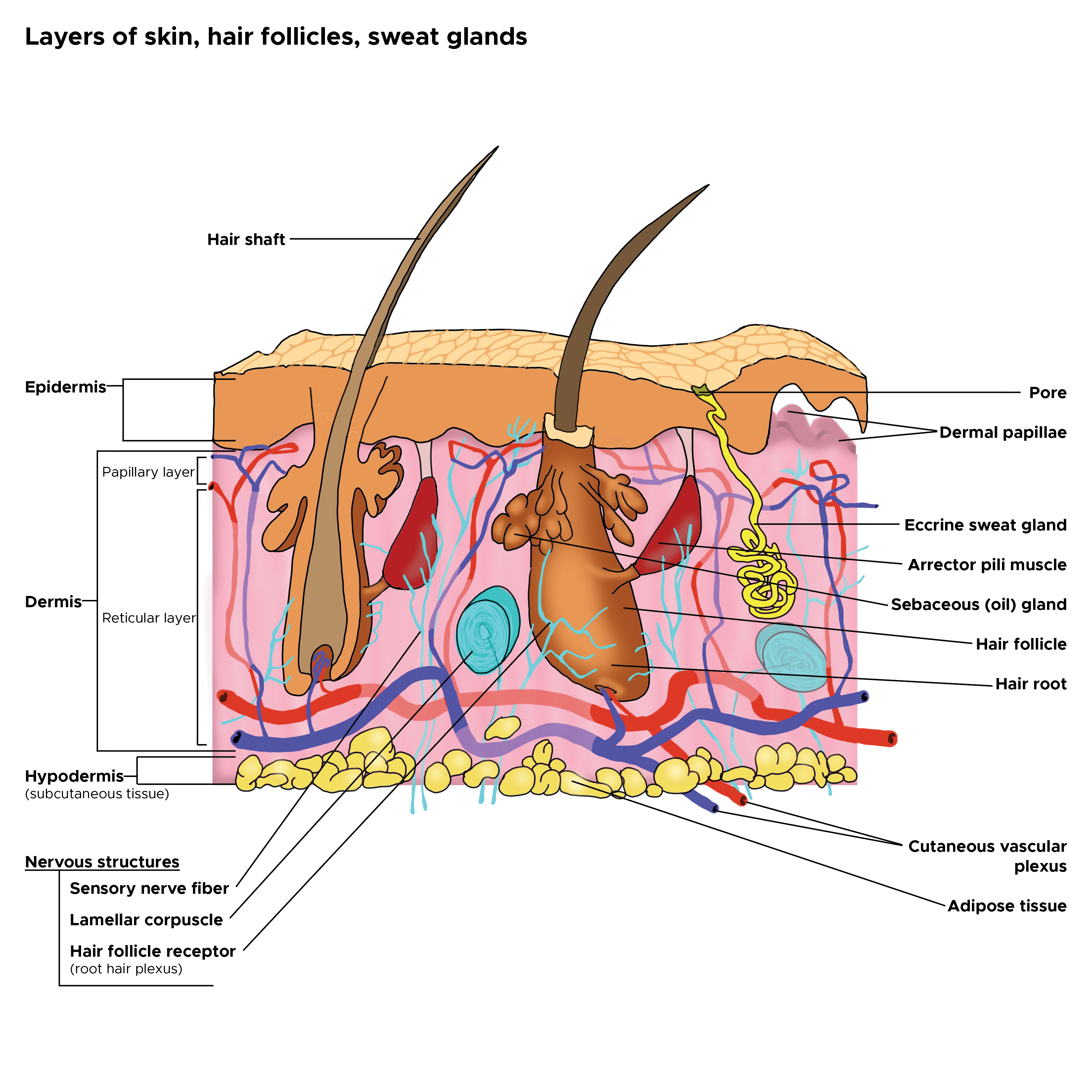
Cross Section, Layers of the Skin. This is a cross-section view of the hair follicles, hair roots and shafts, sweat glands, pores, epidermis, dermis, and hypodermis. The papillary and reticular layers are also included. The eccrine sweat gland is located in the arrector pili muscles, and the sebaceous oil glands are located in the reticular layer.
Contributed by C Rowe
(Click Image to Enlarge)
References
Bonifant H, Holloway S. A review of the effects of ageing on skin integrity and wound healing. British journal of community nursing. 2019 Mar 1:24(Sup3):S28-S33. doi: 10.12968/bjcn.2019.24.Sup3.S28. Epub [PubMed PMID: 30817191]
Herskovitz I, Macquhae F, Fox JD, Kirsner RS. Skin movement, wound repair and development of engineered skin. Experimental dermatology. 2016 Feb:25(2):99-100. doi: 10.1111/exd.12916. Epub [PubMed PMID: 26660718]
PDQ Cancer Genetics Editorial Board. Genetics of Skin Cancer (PDQ®): Health Professional Version. PDQ Cancer Information Summaries. 2002:(): [PubMed PMID: 26389333]
Ravara B, Hofer C, Kern H, Guidolin D, Porzionato A, De Caro R, Albertin G. Dermal papillae flattening of thigh skin in Conus Cauda Syndrome. European journal of translational myology. 2018 Nov 2:28(4):7914. doi: 10.4081/ejtm.2018.7914. Epub 2018 Dec 13 [PubMed PMID: 30662702]
Rzepka K, Schaarschmidt G, Nagler M, Wohlrab J. [Epidermal stem cells]. Journal der Deutschen Dermatologischen Gesellschaft = Journal of the German Society of Dermatology : JDDG. 2005 Dec:3(12):962-73 [PubMed PMID: 16405712]
Level 3 (low-level) evidenceKarim N, Phinney BS, Salemi M, Wu PW, Naeem M, Rice RH. Human stratum corneum proteomics reveals cross-linking of a broad spectrum of proteins in cornified envelopes. Experimental dermatology. 2019 May:28(5):618-622. doi: 10.1111/exd.13925. Epub [PubMed PMID: 30916809]
Brown TM, Krishnamurthy K. Histology, Dermis. StatPearls. 2024 Jan:(): [PubMed PMID: 30570967]
O'Connell RL, Rusby JE. Anatomy relevant to conservative mastectomy. Gland surgery. 2015 Dec:4(6):476-83. doi: 10.3978/j.issn.2227-684X.2015.02.06. Epub [PubMed PMID: 26645002]
Andersson T, Ertürk Bergdahl G, Saleh K, Magnúsdóttir H, Stødkilde K, Andersen CBF, Lundqvist K, Jensen A, Brüggemann H, Lood R. Common skin bacteria protect their host from oxidative stress through secreted antioxidant RoxP. Scientific reports. 2019 Mar 5:9(1):3596. doi: 10.1038/s41598-019-40471-3. Epub 2019 Mar 5 [PubMed PMID: 30837648]
Losquadro WD. Anatomy of the Skin and the Pathogenesis of Nonmelanoma Skin Cancer. Facial plastic surgery clinics of North America. 2017 Aug:25(3):283-289. doi: 10.1016/j.fsc.2017.03.001. Epub 2017 May 30 [PubMed PMID: 28676156]
Slominski AT, Manna PR, Tuckey RC. On the role of skin in the regulation of local and systemic steroidogenic activities. Steroids. 2015 Nov:103():72-88. doi: 10.1016/j.steroids.2015.04.006. Epub 2015 May 16 [PubMed PMID: 25988614]
Sanz-Gómez N, Freije A, Gandarillas A. Keratinocyte Differentiation by Flow Cytometry. Methods in molecular biology (Clifton, N.J.). 2020:2109():83-92. doi: 10.1007/7651_2019_237. Epub [PubMed PMID: 31123997]
Wagner T, Beer L, Gschwandtner M, Eckhart L, Kalinina P, Laggner M, Ellinger A, Gruber R, Kuchler U, Golabi B, Tschachler E, Mildner M. The Differentiation-Associated Keratinocyte Protein Cornifelin Contributes to Cell-Cell Adhesion of Epidermal and Mucosal Keratinocytes. The Journal of investigative dermatology. 2019 Nov:139(11):2292-2301.e9. doi: 10.1016/j.jid.2019.04.019. Epub 2019 May 24 [PubMed PMID: 31129056]
Fenner J, Silverberg NB. Skin diseases associated with atopic dermatitis. Clinics in dermatology. 2018 Sep-Oct:36(5):631-640. doi: 10.1016/j.clindermatol.2018.05.004. Epub 2018 Jun 1 [PubMed PMID: 30217275]
Hall BK. Germ layers, the neural crest and emergent organization in development and evolution. Genesis (New York, N.Y. : 2000). 2018 Jun:56(6-7):e23103. doi: 10.1002/dvg.23103. Epub 2018 Apr 10 [PubMed PMID: 29637683]
Denkler KA, Denkler C. The Direction of Optimal Skin Incisions Derived from Striae Distensae. Plastic and reconstructive surgery. 2015 Jul:136(1):120e-121e. doi: 10.1097/PRS.0000000000001343. Epub [PubMed PMID: 26111326]
Schlader ZJ, Vargas NT. Regulation of Body Temperature by Autonomic and Behavioral Thermoeffectors. Exercise and sport sciences reviews. 2019 Apr:47(2):116-126. doi: 10.1249/JES.0000000000000180. Epub [PubMed PMID: 30632999]
Iizaka S. Skin hydration and lifestyle-related factors in community-dwelling older people. Archives of gerontology and geriatrics. 2017 Sep:72():121-126. doi: 10.1016/j.archger.2017.05.016. Epub 2017 Jun 7 [PubMed PMID: 28624752]
Stecco C, Pirri C, Fede C, Fan C, Giordani F, Stecco L, Foti C, De Caro R. Dermatome and fasciatome. Clinical anatomy (New York, N.Y.). 2019 Oct:32(7):896-902. doi: 10.1002/ca.23408. Epub 2019 May 28 [PubMed PMID: 31087420]
Iheanacho F, Vellipuram AR. Physiology, Mechanoreceptors. StatPearls. 2024 Jan:(): [PubMed PMID: 31082112]
Murphrey MB, Agarwal S, Zito PM. Anatomy, Hair. StatPearls. 2024 Jan:(): [PubMed PMID: 30020684]
Shwartz Y, Gonzalez-Celeiro M, Chen CL, Pasolli HA, Sheu SH, Fan SM, Shamsi F, Assaad S, Lin ET, Zhang B, Tsai PC, He M, Tseng YH, Lin SJ, Hsu YC. Cell Types Promoting Goosebumps Form a Niche to Regulate Hair Follicle Stem Cells. Cell. 2020 Aug 6:182(3):578-593.e19. doi: 10.1016/j.cell.2020.06.031. Epub 2020 Jul 16 [PubMed PMID: 32679029]
Lemperle G, Knapp D, Tenenhaus M. Minimal Scar Formation After Orthopaedic Skin Incisions Along Main Folding Lines. The Journal of bone and joint surgery. American volume. 2019 Mar 6:101(5):392-399. doi: 10.2106/JBJS.18.00331. Epub [PubMed PMID: 30845033]
Tenea D, Dinkel J, Becker JC, van der Walt E. Merkel Cell Carcinoma of the Head in a Young African Albino Woman with HIV/HTLV-1 Coinfection Associated with Multiple Squamous Cell Carcinomas. Case reports in dermatology. 2019 Jan-Apr:11(1):113-122. doi: 10.1159/000499898. Epub 2019 Apr 30 [PubMed PMID: 31143109]
Level 3 (low-level) evidencePDQ Adult Treatment Editorial Board. Melanoma Treatment (PDQ®): Patient Version. PDQ Cancer Information Summaries. 2002:(): [PubMed PMID: 26389388]
PDQ Pediatric Treatment Editorial Board. Langerhans Cell Histiocytosis Treatment (PDQ®): Patient Version. PDQ Cancer Information Summaries. 2002:(): [PubMed PMID: 26389196]
Siqueira SOM, Campos-do-Carmo G, Dos Santos ALS, Martins C, de Melo AC. Merkel cell carcinoma: epidemiology, clinical features, diagnosis and treatment of a rare disease. Anais brasileiros de dermatologia. 2023 May-Jun:98(3):277-286. doi: 10.1016/j.abd.2022.09.003. Epub 2023 Mar 2 [PubMed PMID: 36870886]
Izumi K, Bieber K, Ludwig RJ. Current Clinical Trials in Pemphigus and Pemphigoid. Frontiers in immunology. 2019:10():978. doi: 10.3389/fimmu.2019.00978. Epub 2019 May 3 [PubMed PMID: 31130959]
Jordan KS. Staphylococcal Scalded Skin Syndrome: A Pediatric Dermatological Emergency. Advanced emergency nursing journal. 2019 Apr/Jun:41(2):129-134. doi: 10.1097/TME.0000000000000235. Epub [PubMed PMID: 31033660]
Cribier B. Kératoses actiniques : diagnostic anatomoclinique: Clinicopathologic diagnosis of actinic keratosis. Annales de dermatologie et de venereologie. 2019 May:146 Suppl 2():IIS10-IIS15. doi: 10.1016/S0151-9638(19)30200-5. Epub [PubMed PMID: 31133224]
Vern-Gross TZ, Kowal-Vern A. Erythema multiforme, Stevens Johnson syndrome, and toxic epidermal necrolysis syndrome in patients undergoing radiation therapy: a literature review. American journal of clinical oncology. 2014 Oct:37(5):506-13. doi: 10.1097/COC.0b013e31825d5835. Epub [PubMed PMID: 22892429]
Abulatan IT, Ben-David SG, Morales-Colon LA, Beason E, Fakoya AO. A Compilation of Drug Etiologies of Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis. Cureus. 2023 Nov:15(11):e48728. doi: 10.7759/cureus.48728. Epub 2023 Nov 13 [PubMed PMID: 38094551]
Sander MA, Sander MS, Isaac-Renton JL, Croxen MA. The Cutaneous Microbiome: Implications for Dermatology Practice. Journal of cutaneous medicine and surgery. 2019 Jul/Aug:23(4):436-441. doi: 10.1177/1203475419839939. Epub 2019 Apr 2 [PubMed PMID: 30938174]