Definition/Introduction
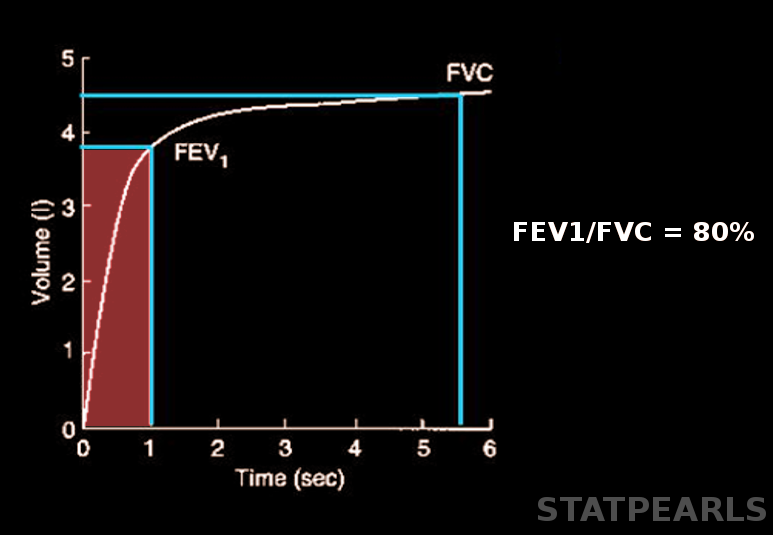
Forced expiratory volume (FEV) refers to the air an individual can exhale during a forced breath in t seconds. (see Image. Forced Expiratory Volume). [1] It is usually represented as FEV, followed by a subscript that indicates the number of seconds of the measurement's duration. For instance, forced expiratory volume in 1 second (FEV1) is the maximum air the subject can forcibly expel during the first second following maximal inhalation.[2] Similarly, forced expiratory volume in 6 seconds (FEV6) is the volume of forcibly exhaled air measured during 6 seconds.[3]
Issues of Concern
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Issues of Concern
Spirometry is a test used to measure the ability of a person to inhale and exhale air respective to time. Forced expiratory volume (FEV) is one of the main results of spirometry.[1] Age and gender are the major factors that affect the average values of FEV in healthy individuals. Height, weight, and ethnicity are some of the other influencing factors.[4][5] FEV values greater than 80% of the predicted average are considered normal.[6] Other factors that can affect the results include decreased patient effort, poor inhalation, inability to follow directions, and some medical conditions that prevent successful spirometry. A weak effort correlates with an overestimation of FEV1.[7]
Clinical Significance
Forced expiratory volume in the first second (FEV1) can be useful to categorize the severity of obstructive lung diseases, such as asthma and chronic obstructive pulmonary disease (COPD). Expressing FEV1 as a percentage of the predicted value in a patient is a means by which to express this severity.[8][9][10]
FEV1 can also be helpful in the interpretation of the reversibility test, also known as the bronchodilator test. This test assesses the bronchodilator response in a patient with obstructive lung disease. It involves the administration of a bronchodilator, such as an anticholinergic agent or a short-acting beta-2 agonist. An increase in the FEV1 of greater than or equal to 12%, or greater than or equal to 200 mL, after bronchodilator use is considered a positive bronchodilator response. A positive response typically presents in reversible airway obstruction, such as asthma. In contrast, nonreversible obstruction, as seen in COPD, may not show a positive response to the administration of a bronchodilator.[8][10][11]
The ratio of FEV1 to FVC (FEV1/FVC, also known as FEV1%) can help distinguish obstructive and restrictive lung diseases. In obstructive diseases, FEV1 reduction is due to the increased airway resistance to expiratory flow. A reduction in the FVC may also present because of premature airway closure in expiration; however, it is not affected as much as FEV1 and, thus, is not decreased in the same proportion as FEV1, which can lead to a reduced value of FEV1/FVC, of less than 70%.[9] On the other hand, in restrictive lung diseases, such as chest wall deformities and idiopathic pulmonary fibrosis, the FVC may be decreased more as compared to FEV1, thus giving an FEV1/FVC ratio of more than 70%.[12] Forced expiratory volume in 6 seconds (FEV6) has been proposed as a valid alternative for forced vital capacity (FVC) in diagnosing airflow obstruction in elderly individuals.[3][13][14]
Media
(Click Image to Enlarge)
References
Ponce MC, Sankari A, Sharma S. Pulmonary Function Tests. StatPearls. 2024 Jan:(): [PubMed PMID: 29493964]
Matarese A, Sardu C, Shu J, Santulli G. Why is chronic obstructive pulmonary disease linked to atrial fibrillation? A systematic overview of the underlying mechanisms. International journal of cardiology. 2019 Feb 1:276():149-151. doi: 10.1016/j.ijcard.2018.10.075. Epub 2018 Oct 25 [PubMed PMID: 30446289]
Level 3 (low-level) evidencePan MM, Zhang HS, Sun TY. [Value of forced expiratory volume in 6 seconds (FEV(6)) in the evaluation of pulmonary function in Chinese elderly males]. Zhonghua yi xue za zhi. 2017 May 30:97(20):1556-1561. doi: 10.3760/cma.j.issn.0376-2491.2017.20.011. Epub [PubMed PMID: 28592061]
Zakaria R, Harif N, Al-Rahbi B, Aziz CBA, Ahmad AH. Gender Differences and Obesity Influence on Pulmonary Function Parameters. Oman medical journal. 2019 Jan:34(1):44-48. doi: 10.5001/omj.2019.07. Epub [PubMed PMID: 30671183]
Gao C, Zhang X, Wang D, Wang Z, Li J, Li Z. Reference values for lung function screening in 10- to 81-year-old, healthy, never-smoking residents of Southeast China. Medicine. 2018 Aug:97(34):e11904. doi: 10.1097/MD.0000000000011904. Epub [PubMed PMID: 30142794]
Shapira U, Krubiner M, Ehrenwald M, Shapira I, Zeltser D, Berliner S, Rogowski O, Shenhar-Tsarfaty S, Bar-Shai A. Eosinophil levels predict lung function deterioration in apparently healthy individuals. International journal of chronic obstructive pulmonary disease. 2019:14():597-603. doi: 10.2147/COPD.S192594. Epub 2019 Mar 7 [PubMed PMID: 30880949]
Derom E, van Weel C, Liistro G, Buffels J, Schermer T, Lammers E, Wouters E, Decramer M. Primary care spirometry. The European respiratory journal. 2008 Jan:31(1):197-203. doi: 10.1183/09031936.00066607. Epub [PubMed PMID: 18166597]
Gallucci M, Carbonara P, Pacilli AMG, di Palmo E, Ricci G, Nava S. Use of Symptoms Scores, Spirometry, and Other Pulmonary Function Testing for Asthma Monitoring. Frontiers in pediatrics. 2019:7():54. doi: 10.3389/fped.2019.00054. Epub 2019 Mar 5 [PubMed PMID: 30891435]
Devasahayam J, LaFreniere K, Naik R. Chronic Emphysema. StatPearls. 2024 Jan:(): [PubMed PMID: 30969732]
Pahal P, Avula A, Sharma S. Emphysema. StatPearls. 2024 Jan:(): [PubMed PMID: 29489292]
Fortis S, Comellas A, Make BJ, Hersh CP, Bodduluri S, Georgopoulos D, Kim V, Criner GJ, Dransfield MT, Bhatt SP, COPDGene Investigators–Core Units: <italic>Administrative Center</italic>, COPDGene Investigators–Clinical Centers: <italic>Ann Arbor VA</italic>. Combined Forced Expiratory Volume in 1 Second and Forced Vital Capacity Bronchodilator Response, Exacerbations, and Mortality in Chronic Obstructive Pulmonary Disease. Annals of the American Thoracic Society. 2019 Jul:16(7):826-835. doi: 10.1513/AnnalsATS.201809-601OC. Epub [PubMed PMID: 30908927]
Carsin AE, Fuertes E, Schaffner E, Jarvis D, Antó JM, Heinrich J, Bellisario V, Svanes C, Keidel D, Imboden M, Weyler J, Nowak D, Martinez-Moratalla J, Gullón JA, Sanchez Ramos JL, Caviezel S, Beckmeyer-Borowko A, Raherison C, Pin I, Demoly P, Cerveri I, Accordini S, Gislason T, Toren K, Forsberg B, Janson C, Jogi R, Emtner M, Gómez Real F, Raza W, Leynaert B, Pascual S, Guerra S, Dharmage SC, Probst-Hensch N, Garcia-Aymerich J. Restrictive spirometry pattern is associated with low physical activity levels. A population based international study. Respiratory medicine. 2019 Jan:146():116-123. doi: 10.1016/j.rmed.2018.11.017. Epub 2018 Dec 15 [PubMed PMID: 30665509]
Chen G, Jiang L, Wang L, Zhang W, Castillo C, Fang X. The accuracy of a handheld "disposable pneumotachograph device" in the spirometric diagnosis of airway obstruction in a Chinese population. International journal of chronic obstructive pulmonary disease. 2018:13():2351-2360. doi: 10.2147/COPD.S168583. Epub 2018 Aug 2 [PubMed PMID: 30122915]
Reyes-García A, Torre-Bouscoulet L, Pérez-Padilla R. CONTROVERSIES AND LIMITATIONS IN THE DIAGNOSIS OF CHRONIC OBSTRUCTIVE PULMONARY DISEASE. Revista de investigacion clinica; organo del Hospital de Enfermedades de la Nutricion. 2019:71(1):28-35. doi: 10.24875/RIC.18002626. Epub [PubMed PMID: 30810541]
Alotaibi N, Borg BM, Abramson MJ, Paul E, Zwar N, Russell G, Wilson S, Holland AE, Bonevski B, Mahal A, George J. Different Case Finding Approaches to Optimise COPD Diagnosis: Evidence from the RADICALS Trial. International journal of chronic obstructive pulmonary disease. 2023:18():1543-1554. doi: 10.2147/COPD.S371371. Epub 2023 Jul 20 [PubMed PMID: 37492489]
Level 3 (low-level) evidenceBhatt SP, Kim YI, Wells JM, Bailey WC, Ramsdell JW, Foreman MG, Jensen RL, Stinson DS, Wilson CG, Lynch DA, Make BJ, Dransfield MT. FEV(1)/FEV(6) to diagnose airflow obstruction. Comparisons with computed tomography and morbidity indices. Annals of the American Thoracic Society. 2014 Mar:11(3):335-41. doi: 10.1513/AnnalsATS.201308-251OC. Epub [PubMed PMID: 24450777]