Anatomy, Abdomen and Pelvis: Genitofemoral Nerve
Anatomy, Abdomen and Pelvis: Genitofemoral Nerve
Introduction
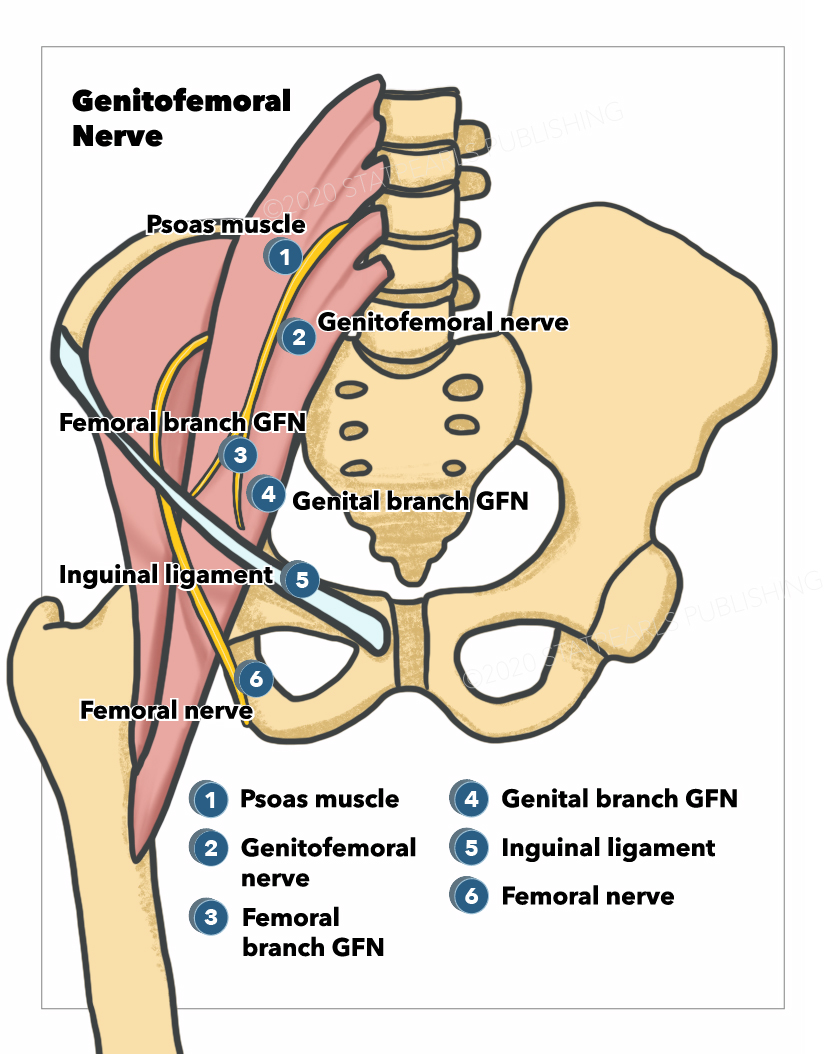
The genitofemoral nerve arises from the lumbar plexus (see Image. Genitofemoral Nerve) and supplies sensation to the skin of the anterior scrotal area in males, mons pubis in women, and the upper segment of the anterior thigh in both males and females. While distinct from the femoral nerve, the genitofemoral nerve originates from the upper lumbar segments L1 to L2. The nerve then descends inferiorly, piercing the psoas major muscle before emerging on its anterior surface. The nerve then traverses the retroperitoneum, descending over the anterior surface of the psoas muscle. The nerve continues inferiorly, ultimately separating into two divisions- the femoral and the genital branches. When the genitofemoral nerve reaches the groin area, it enters the deep inguinal ring coursing through the inguinal canal.[1][2] In men, the nerve continues inferiorly and supplies the skin of the scrotum. In women, the genitofemoral nerve runs alongside the round ligament of the uterus and terminates superior to the mons pubis and labia majora. Further, after crossing the inguinal ligament, the genitofemoral nerve travels adjacent to the external iliac artery, supplying sensation to the anterior upper thigh.[3]
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The genitofemoral nerve supplies sensation via the femoral branch and motor innervation via the genital branch. The cremasteric reflex is a function of genitofemoral nerve innervation, as it supplies sensation to the superior medial aspect of the thigh. In at least 50% of individuals, there is some variation in the course of the genitofemoral nerve as it travels within the retroperitoneum and ultimately enters into the inguinal canal. Variation is also found at the level of its bifurcation into genital and femoral branches.
Blood Supply and Lymphatics
The genitofemoral nerve is formed in the psoas muscle's midsection by the branches' union from the anterior rami of L1 and L2 nerve roots. The nerve then courses inferiorly within the psoas muscle and finally emerges on the anterior surface of the muscle distally. The nerve then descends inferiorly in the retroperitoneum along the psoas major muscle and courses deeper and on the left to the gonadal vessels, ureter, and the ileocolic vein and artery. Just before the nerve reaches the inguinal ligament, the right and left genitofemoral nerves perforate the psoas fascia and divide into the femoral and genital branches.
Nerves
The genital branch of the genitofemoral nerve enters the inguinal canal via the deep inguinal ring. In men, the genital branch supplies the scrotal skin and cremaster (see Image. The Sacral and Coccygeal Nerves). In women, the genital branch is accompanied by the round ligament of the uterus and supplies sensation to the labia majora and mons pubis. The femoral branch of the genitofemoral nerve travels beneath the inguinal ligament in the lateral muscular compartment, where the femoral nerve courses through into the leg. The femoral branch enters the cribriform fascia of the greater saphenous vein opening and supplies the skin of the thigh's anterior, upper, and medial aspects.
Physiologic Variants
Cadaveric studies have reported significant variation in the course of the genitofemoral nerve in over half of the specimens. While most specimens exhibit a predictable bifurcation pattern of the nerve in the mid-substance of the psoas muscle, a recent study noted that the genitofemoral nerve prematurely bifurcates in the upper portion of the psoas muscle about 20% of the time. Also, the femoral and genital branches do not form a common trunk within the psoas muscle and remain as distinct nerves as they course in the retroperitoneum.
Surgical Considerations
Inguinal hernia repair
During surgery to repair an inguinal hernia, one has to visualize the genitofemoral nerve, which is found within the deep inguinal ring. If damaged, the patient will complain of pain in the scrotal area and anterior thigh. The injury can result in genitofemoral neuralgia, causing morbidity as no good treatment currently exists. For exam purposes, one must differentiate between the genitofemoral and ilioinguinal nerves, which can be injured during surgery.[4][5][6]
Lumbar spinal interbody fusion
During lumbar spine surgical procedures, the surgeon must know the anatomic relationships between the lumbar plexus and the intervertebral disc at all levels. This concept is particularly relevant when performing lateral interbody fusion by minimally invasive retroperitoneal trans-psoas approaches. Ventral nerve roots of the lumbar plexus are particularly vulnerable during psoas muscle retraction. Surgeons must be aware of the "safe working zone" about the particular level of interest regarding the level of pathology being treated. This "safe zone" is typically located between the lumbar nerve's anterior border and the sympathetic trunk's posterior border. The genitofemoral nerve appears to be solely responsible for narrowing this safe zone, with its most significant anatomic impact being recognized at the L2 to L3 level.
Clinical Significance
The genitofemoral nerve can be injured during surgery in several ways:
- This can be lacerated during injury to the groin and can occur with penetrating trauma, a knife wound, or surgical exploration of the groin. In some cases, during surgery on the saphenous vein for varicose vein ligation, retractors can cause abrasive injury.
- The genitofemoral nerve can also be injured in the inguinal canal, usually during inguinal hernia repair. In most cases, the injury goes unnoticed during surgery and is diagnosed in the postoperative period when the patient complains of pain.
- The genitofemoral nerve can also be injured during a motor vehicle accident. The lower back injury may result in an extension of the back while the patient is seated.
- Lifting heavy objects can also cause injury to the genitofemoral nerve.
- When there is spinal stenosis of the L1 or L2 segments, compression fracture, or metastatic lesions to the lumbar spine, the nerve roots, which give rise to the genitofemoral nerve, can be injured.
- Psoas abscess which may occur after an open pelvic fracture or a retroperitoneal hematoma, is also known to cause irritation of the genitofemoral nerve.
Other Issues
Genitofemoral neuralgia is a relatively common pain syndrome observed in men and women. The patient typically presents with unilateral pain in the lower abdomen. Rarely the pain may be bilateral. The pain is sometimes referred to as the groin area (because of the path of the genital nerve) and the upper medial thigh (because of the femoral branch). The pain varies in intensity from moderate to severe and is worsened by movements that cause lower back extension. In most patients, palpation of the lower abdomen in the inguinal region can reproduce the pain. In most cases, the cause is compression of the nerve in the inguinal canal, usually after open hernia surgery. The diagnosis is often difficult in patients who have not had surgery.[7][8]
The prognosis of patients who suffer entrapment or injury to the genitofemoral nerve is guarded. If the nerve is entrapped in the inguinal canal after inguinal hernia surgery, one may try decompression, but often the scarring makes visualization of the nerve difficult. In patients with a lacerated nerve, many pain-relieving modalities have been used, but none works effectively. Some patients respond to nerve blocks, but most patients require long-term anticonvulsants and opiates for pain relief.
Media
(Click Image to Enlarge)
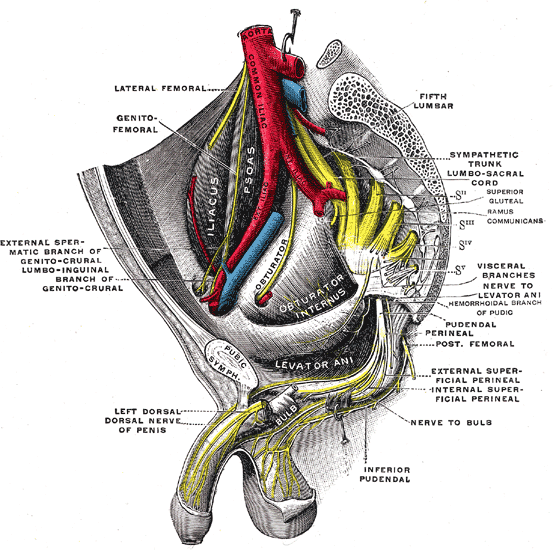
Sacral and Coccygeal Nerves. The illustration depicts the sacral plexus of the right side, pelvic area, coccyx, dorsal nerve of the penis, nerve to bulb, and genitofemoral nerve.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
References
Mahabadi N, Lew V, Kang M. Anatomy, Abdomen and Pelvis: Femoral Sheath. StatPearls. 2024 Jan:(): [PubMed PMID: 29494010]
Benes J, Nádvornik P, Dolezel J. Abdominoinguinal pain syndrome treated by centrocentral anastomosis. Acta neurochirurgica. 2000:142(8):887-91 [PubMed PMID: 11086827]
Level 3 (low-level) evidenceLee KS, Sin JM, Patil PP, Hanna AS, Greenberg JA, Zea RD, Brace CL. Ultrasound-Guided Microwave Ablation for the Management of Inguinal Neuralgia: A Preliminary Study with 1-Year Follow-up. Journal of vascular and interventional radiology : JVIR. 2019 Feb:30(2):242-248. doi: 10.1016/j.jvir.2018.10.031. Epub [PubMed PMID: 30717957]
Iwanaga J, Simonds E, Schumacher M, Kikuta S, Watanabe K, Tubbs RS. Revisiting the genital and femoral branches of the genitofemoral nerve: Suggestion for a more accurate terminology. Clinical anatomy (New York, N.Y.). 2019 Apr:32(3):458-463. doi: 10.1002/ca.23327. Epub [PubMed PMID: 30592097]
Cirocchi R, Henry BM, Mercurio I, Tomaszewski KA, Palumbo P, Stabile A, Lancia M, Randolph J. Is it possible to identify the inguinal nerves during hernioplasty? A systematic review of the literature and meta-analysis of cadaveric and surgical studies. Hernia : the journal of hernias and abdominal wall surgery. 2019 Jun:23(3):569-581. doi: 10.1007/s10029-018-1857-2. Epub 2018 Dec 20 [PubMed PMID: 30570686]
Level 1 (high-level) evidenceMellick LB, Mowery ML, Al-Dhahir MA. Cremasteric Reflex. StatPearls. 2024 Jan:(): [PubMed PMID: 30020720]
Zhu CL, Zhong H, Li CH. [Anatomic application of the genitofemoral nerve in uroandrological surgery]. Zhonghua nan ke xue = National journal of andrology. 2017 Mar:23(3):276-279 [PubMed PMID: 29706052]
Narita M, Jikihara S, Hata H, Matsusue R, Yamaguchi T, Otani T, Ikai I. Surgical experience of laparoscopic retroperitoneal triple neurectomy for a patient with chronic neuropathic inguinodynia. International journal of surgery case reports. 2017:40():80-84. doi: 10.1016/j.ijscr.2017.09.012. Epub 2017 Sep 15 [PubMed PMID: 28942229]
Level 3 (low-level) evidence