Introduction
The gestational sac is a fluid-filled structure surrounding an embryo during the first few weeks of embryonic development. It is the first structure seen in pregnancy by ultrasound as early as 4.5 to 5 weeks of gestational age and is 97.6% specific for the diagnosis of intrauterine pregnancy (IUP).[1]
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
The uterus is a female reproductive organ that can be visualized by transabdominal or transvaginal ultrasound posterior to the bladder and anterior to the colon. Ovaries are paired reproductive organs and can be found lateral to the uterus in the pelvic cavity. The uterus has three parts: the cervix, the body, and the fundus. In non-pregnant females, the uterine cavity collapses. In early pregnancy, by 4.5 to 5 weeks gestation, the gestational sac appears in the central portion of the uterine body, initially measuring 2 to 3 mm in diameter.[2]
Indications
In the absence of any concerning symptoms, first-trimester fetal ultrasound should be performed between 11 and 13 weeks gestation to establish gestational age and assess viability.[3] Early pregnancies with symptoms of abdominal pain, pelvic pain, and vaginal bleeding require evaluation with pelvic ultrasound to differentiate between IUP, pregnancy of unknown location, and ectopic pregnancy.
Equipment
Comprehensive first-trimester two-dimensional obstetric ultrasound includes transabdominal and transvaginal examinations. Curvilinear probe (1 to 6 MHz) is used for the transabdominal approach, while high-frequency (7.5 to 10 MHz) transvaginal probe is the choice for the pelvic portion of the ultrasound.[4]
Technique or Treatment
First, a transabdominal examination takes place, focusing on visualization of the entire uterus as well as adnexa bilaterally. The patient should localize her pain, and the examiner obtains dedicated images of this area. The pelvis undergoes assessment for signs of hemoperitoneum, and, if there is an extrauterine fluid collection identified, the upper abdomen (Morrison’s pouch and paracolic gutters) gets scanned to determine the extent of bleeding. Next, a transvaginal portion of the examination is performed, focusing on further evaluation of the uterus, fallopian tubes, and ovaries.[4] Transvaginal sonography (TVS) produces improved resolution as compared to the transabdominal approach, primarily due to the higher frequencies used and also due to the absence of beam deformation by the anterior abdominal wall. Transvaginal ultrasound also does not require a full bladder.[5] M-mode ultrasonography is considered safe for all stages of pregnancy. Doppler ultrasonography is associated with much higher energy output and is the recommended modality only if clinically indicated.[3]
Mean gestational sac diameter (mGSD) gets calculated by taking an average of measurements obtained in three orthogonal planes. In other words, it can be calculated by adding measurements of the height, width, and length and dividing the sum by 3.[6]
Clinical Significance
Patients with early pregnancy and concerning clinical symptoms of abdominal pain, pelvic pain, or vaginal bleeding must be evaluated by pelvic ultrasonography and human chorionic gonadotropin (B-hCG) serum levels testing, which, in combination, help guide patient management. These two tests assist in differentiation between the IUP, pregnancy of unknown location, and ectopic pregnancy.
Embryonic development between 5 and 7 weeks of gestation follows a predictable pattern, which can be used in early pregnancy to determine the location of pregnancy and gestational age. The first sonographic feature of pregnancy is a gestational sac, appearing at 4.5 to 5 weeks of gestation. A normal gestational sac appears as a round structure in the central echogenic portion of the uterine body, initially measuring 2 to 3 mm in diameter and increasing by 1.13 mm per day. By 5.5 weeks gestation, a thin-walled circular structure, the yolk sac, can be seen within the gestational sac, which reaches approximately 6 mm by the time the yolk sac is visible. By six weeks of gestation, a 1 to 2 mm structure within the yolk sac is visible, which represents the embryo. Embryo size is measured using crown-rump length (CRL) assessment, which is the most accurate gestational age estimation tool in early pregnancy. By eight weeks of gestation, the head, body, and limb buds become apparent.[2][7]
Intrauterine gestational sac identification via ultrasonography has 97.6% specificity for the diagnosis of IUP, while the yolk sac visualization has 100% specificity.[1] A normal-appearing gestational sac is smooth, round, or oval and is in the central portion of the uterus (other locations of the gestational sac should raise concerns for ectopic pregnancy). If intrauterine fluid collection is not round/oval, then a “pseudogestational sac” term can be applied. “Pseudogestational sac” has sharp edges with possible debris within the lumen and can be seen in ectopic pregnancies.[8] In some cases, double sac or intradecidual signs are observable before yolk sac development. Double sac sign and intradecidual sign represent two layers of decidua within the uterine wall and appear as echogenic rings surrounding the gestational sac, which strongly suggest an IUP, but are not always present.[9]
Given the predictability of early embryonic development, the gestational sac diameter of a certain size without an embryo is diagnostic of pregnancy failure. Mean sac diameter (MSD) of 25 mm without an embryo is indicative of pregnancy failure, while MSD between 16 and 25 mm without an embryo is suggestive of possible pregnancy failure. Additional criteria for pregnancy failure diagnosis include failure of yolk sac to develop two or more weeks after visualizing the gestational sac and failure of an embryo with a heartbeat to develop 11 or more days after visualization of the yolk sac within the gestational sac. In this case, a repeat ultrasound is an option in 11 to 14 days.[8][10]
In the past, B-hCG “discriminatory levels” were the method to aid in the diagnosis and management of early pregnancy. However, research has shown that serum B-hCG levels vary significantly during pregnancy, and isolated B-hCG serum level should not be solely relied upon in the diagnosis of early pregnancy when there is no definitive IUP identified sonographically.[11] Rather, serial B-hCG levels are recommended in addition to repeat imaging when the diagnosis is unclear. In cases of early pregnancy, when there is an identified a nonspecific intrauterine fluid collection is detected in patients with elevated B-hCG levels who are clinically stable, the most appropriate diagnosis is the pregnancy of unknown location. Since the incidence of ectopic pregnancies is approximately 2%, a nonspecific intrauterine fluid collection with normal imaging of adnexa is more likely to represent an early intrauterine pregnancy. In these cases, the recommendation os for repeat imaging and B-hCG testing in 48 to 72 hours.[12]
Enhancing Healthcare Team Outcomes
Females presenting for evaluation of abdominal pain or vaginal bleeding with elevated B-hCG levels present a diagnostic dilemma in the early stage of pregnancy if an imaging study does not clearly demonstrate an intrauterine pregnancy. An interprofessional team effort will improve outcomes in diagnosing and treating these cases.
In a female of childbearing age pregnancy test is the first step in the evaluation of their presenting complaint. If the patient is clinically stable, and a pregnancy test is positive, a pelvic ultrasound is necessary to evaluate the location of the pregnancy. If there is an ectopic pregnancy identified, the OBGYN team must be involved in the patient’s care as soon as possible. However, in cases of pregnancy of unknown location, close follow up must be arranged by the evaluating clinician, and strict return precautions are necessary for the patient, given the possibility of early ectopic pregnancy. A nurse with obstetric/neonatal specialization may be of great assistance, as they can help irrespective of the diagnosis and direction of treatment by providing counsel to the patient and assisting in any procedures. This situation requires diligence and communication between different providers to ensure proper follow-up. Radiologists must be familiar with normal and abnormal ultrasound findings of early pregnancy and use the most conservative criteria when assessing the viability and diagnosing pregnancy failure. The referring physician should provide clinical history and order B-hCG quantitative level to assist the radiologist in the interpretation of imaging studies. As a team, referring physicians, nurse practitioners, OBGYN specialists, and radiologists must collaborate to protect the mother and baby and to intervene only in cases of definitive ectopic or failed pregnancy. (Level I)
The interprofessional team approach is necessary to manage these cases and arrive at the best management option. [Level 5]
Media
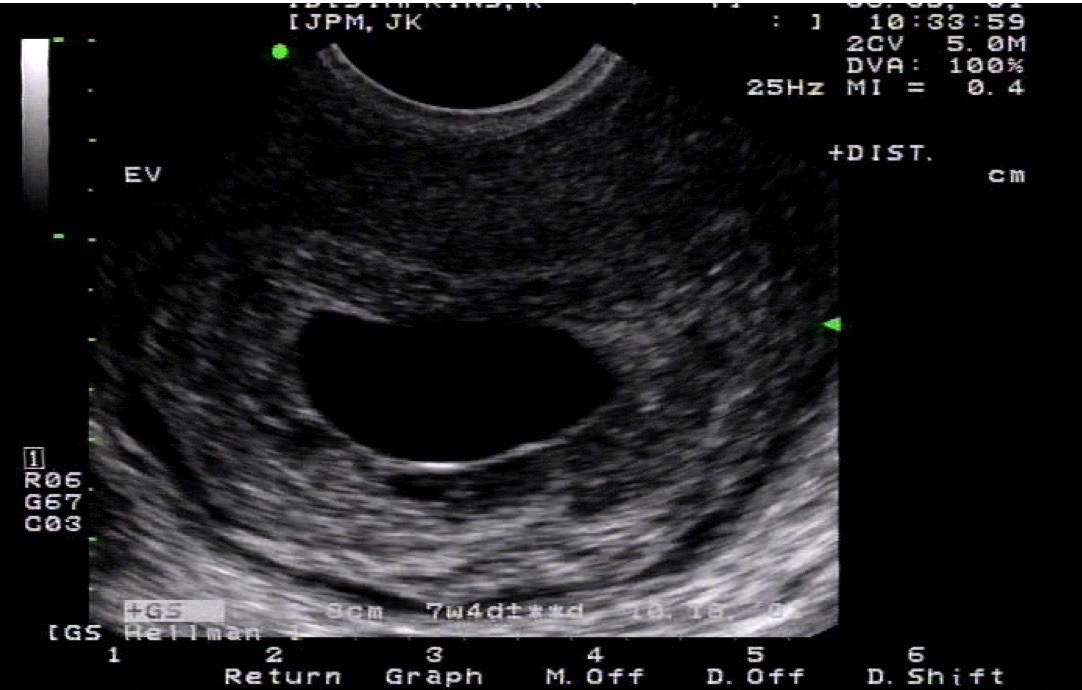
(Click Image to Enlarge)
(Click Image to Enlarge)
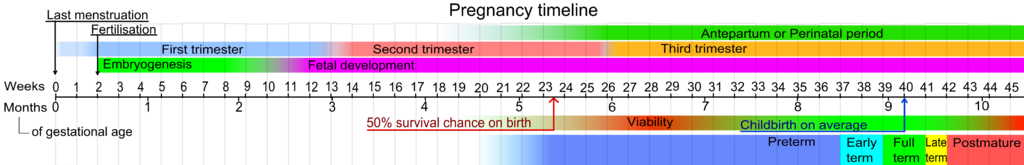
Pregnancy Timeline. The most important step in the initial evaluation of any pregnant patient is establishing an accurate delivery date or due date.
Mikael Häggström, Public Domain, via Wikimedia Commons
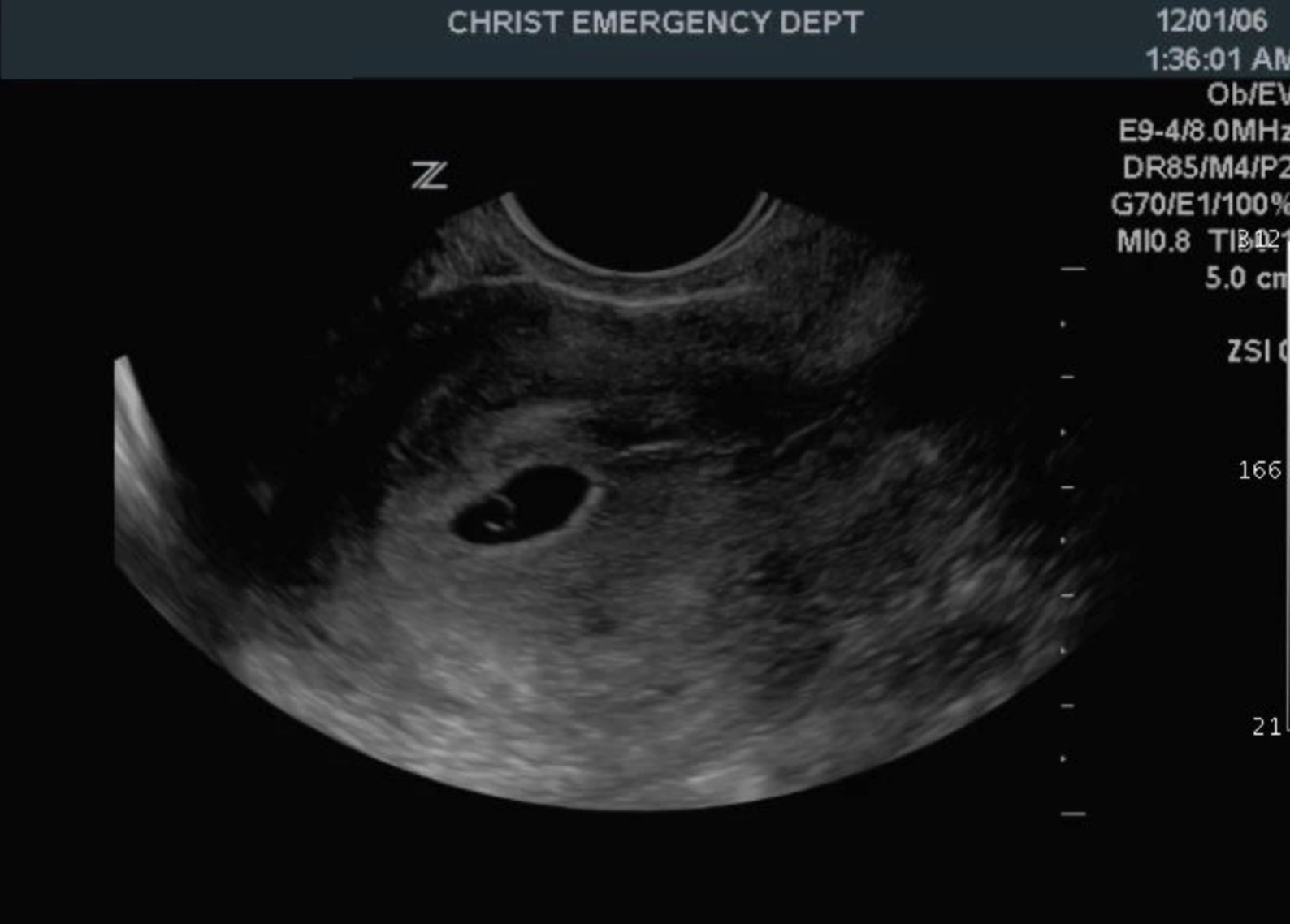
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Richardson A, Gallos I, Dobson S, Campbell BK, Coomarasamy A, Raine-Fenning N. Accuracy of first-trimester ultrasound in diagnosis of intrauterine pregnancy prior to visualization of the yolk sac: a systematic review and meta-analysis. Ultrasound in obstetrics & gynecology : the official journal of the International Society of Ultrasound in Obstetrics and Gynecology. 2015 Aug:46(2):142-9. doi: 10.1002/uog.14725. Epub 2015 Jun 29 [PubMed PMID: 25393076]
Level 1 (high-level) evidenceDoubilet PM. Ultrasound evaluation of the first trimester. Radiologic clinics of North America. 2014 Nov:52(6):1191-9. doi: 10.1016/j.rcl.2014.07.004. Epub 2014 Aug 24 [PubMed PMID: 25444100]
Salomon LJ, Alfirevic Z, Bilardo CM, Chalouhi GE, Ghi T, Kagan KO, Lau TK, Papageorghiou AT, Raine-Fenning NJ, Stirnemann J, Suresh S, Tabor A, Timor-Tritsch IE, Toi A, Yeo G. ISUOG practice guidelines: performance of first-trimester fetal ultrasound scan. Ultrasound in obstetrics & gynecology : the official journal of the International Society of Ultrasound in Obstetrics and Gynecology. 2013 Jan:41(1):102-13. doi: 10.1002/uog.12342. Epub [PubMed PMID: 23280739]
Level 1 (high-level) evidenceMausner Geffen E, Slywotzky C, Bennett G. Pitfalls and tips in the diagnosis of ectopic pregnancy. Abdominal radiology (New York). 2017 May:42(5):1524-1542. doi: 10.1007/s00261-016-1020-4. Epub [PubMed PMID: 28144719]
Moorthy RS. TRANSVAGINAL SONOGRAPHY. Medical journal, Armed Forces India. 2000 Jul:56(3):181-183. doi: 10.1016/S0377-1237(17)30160-0. Epub 2017 Jun 10 [PubMed PMID: 28790701]
Kapfhamer JD, Palaniappan S, Summers K, Kassel K, Mancuso AC, Ryan GL, Shah DK. Difference between mean gestational sac diameter and crown-rump length as a marker of first-trimester pregnancy loss after in vitro fertilization. Fertility and sterility. 2018 Jan:109(1):130-136. doi: 10.1016/j.fertnstert.2017.09.031. Epub 2017 Nov 23 [PubMed PMID: 29175064]
Blaas HG. Detection of structural abnormalities in the first trimester using ultrasound. Best practice & research. Clinical obstetrics & gynaecology. 2014 Apr:28(3):341-53. doi: 10.1016/j.bpobgyn.2013.11.004. Epub 2013 Dec 4 [PubMed PMID: 24355991]
Doubilet PM, Benson CB, Bourne T, Blaivas M, Society of Radiologists in Ultrasound Multispecialty Panel on Early First Trimester Diagnosis of Miscarriage and Exclusion of a Viable Intrauterine Pregnancy, Barnhart KT, Benacerraf BR, Brown DL, Filly RA, Fox JC, Goldstein SR, Kendall JL, Lyons EA, Porter MB, Pretorius DH, Timor-Tritsch IE. Diagnostic criteria for nonviable pregnancy early in the first trimester. The New England journal of medicine. 2013 Oct 10:369(15):1443-51. doi: 10.1056/NEJMra1302417. Epub [PubMed PMID: 24106937]
Doubilet PM, Benson CB. Double sac sign and intradecidual sign in early pregnancy: interobserver reliability and frequency of occurrence. Journal of ultrasound in medicine : official journal of the American Institute of Ultrasound in Medicine. 2013 Jul:32(7):1207-14. doi: 10.7863/ultra.32.7.1207. Epub [PubMed PMID: 23804343]
Preisler J, Kopeika J, Ismail L, Vathanan V, Farren J, Abdallah Y, Battacharjee P, Van Holsbeke C, Bottomley C, Gould D, Johnson S, Stalder C, Van Calster B, Hamilton J, Timmerman D, Bourne T. Defining safe criteria to diagnose miscarriage: prospective observational multicentre study. BMJ (Clinical research ed.). 2015 Sep 23:351():h4579. doi: 10.1136/bmj.h4579. Epub 2015 Sep 23 [PubMed PMID: 26400869]
Doubilet PM, Benson CB. Further evidence against the reliability of the human chorionic gonadotropin discriminatory level. Journal of ultrasound in medicine : official journal of the American Institute of Ultrasound in Medicine. 2011 Dec:30(12):1637-42 [PubMed PMID: 22123998]
Mazzariol FS, Roberts J, Oh SK, Ricci Z, Koenigsberg M, Stein MW. Pearls and pitfalls in first-trimester obstetric sonography. Clinical imaging. 2015 Mar-Apr:39(2):176-85. doi: 10.1016/j.clinimag.2014.10.009. Epub 2014 Oct 23 [PubMed PMID: 25457572]